Abstract
Background
Neck flexion has been shown to increase cranial spread of contrast agent when a small fixed volume was injected into the high thoracic epidural space. The purpose of this study was to evaluate the effect of volume of contrast medium on its distribution through the high thoracic epidural space during neck extension and flexion using the rabbit model.
Methods
An epidural catheter was introduced into the epidural space of New Zealand white rabbits with the tip located at the T3-4 intervertebral level. The neck was extended or flexed (n = 8 for each group), and the contrast medium was injected with the volume increasing by increments of 0.1 ml/kg, up to 0.3 ml/kg. The spread of contrast medium was determined by counting the number of vertebral body units using lateral epidurographic images.
Results
In both groups, the total spread of contrast medium was similar, increasing continuously with injected volume. The cranial spread was greater in the flexion group than the extension group. However, the caudal spread was greater in the extension than in the flexion group. In the extension group, the contrast medium spread caudally about twice as far as it spread cranially, but there was no statistically significant difference between cranial and caudal spread in the flexion group.
Thoracic epidural anesthesia has been shown to induce adequate postoperative analgesia [1] and to be an alternative to general anesthesia in patients with impaired respiratory function [2] or those undergoing coronary artery bypass surgery [3,4], and its practice has accordingly increased [5]. But, if local anesthetics spread to cervical levels during high thoracic epidural anesthesia, a fatal phrenic nerve block can develop. Because of the anatomical differences between the lumbar and thoracic epidural space, the spreading pattern of local anesthetics can be different between for each epidural level [6]. It is important to understand the factors affecting the distribution of local anesthetics in the high thoracic epidural space in order to achieve safe and effective analgesia.
Although many factors have been identified which influence epidural spread of local anesthetics at the lumbar level [7-11], only a few studies have been published on its spread in the thoracic epidural space. In the high thoracic epidural space, it was consistently shown that the cranial spread of local anesthetics is limited, and the caudal spread is facilitated [12,13]. Recently, we have observed that this spreading pattern in the high thoracic epidural space can be affected by flexion and extension of the neck, with cranial spread increasing by neck flexion [14]. In that study, a small fixed volume of contrast medium was used. However, various doses of epidural agents are used in clinical practice. We therefore injected contrast medium in increments in the rabbit, and evaluated the effect of volume on the distribution of contrast medium in the high thoracic epidural space during neck extension and flexion.
The study protocol and experimental design were approved by the Institutional Animal Care Use Committee at our university hospital. Sixteen male conventional New Zealand white rabbits (2.4-2.6 kg) were used.
The study technique was based on the method from the previous paper [15]. Briefly, following intramuscular injection of xylazine (5 mg/kg) and ketamine (10 mg/kg), intubation was done and the rabbits were ventilated with an animal respirator (665, Harvard Apparatus, South Natick, MA, USA). Normal PaCO2 (35-45 mmHg) was maintained by ventilator adjustments and rectal temperature was maintained at 37.0-39.0℃ using a heating lamp.
With the rabbits in the prone position, the vertebral arches of T7 and T10 were surgically exposed and the spinous process of T8 was removed. After gentle elevation of the spinous process of T7 with forceps, the midline of the ligamentum flavum beneath the spinous process was carefully punctured with a round-tipped blunt hook. An end hole epidural catheter (19 G, 0.9 mm outer diameter, 0.1 ml priming volume, Portex, UK) was introduced into the epidural space. The catheter was advanced cranially until the tip of the catheter was located at T3-4 intervertebral level. The location of the catheter tip was confirmed using fluoroscopy with an injection of 0.1 ml of contrast medium (Iopamidol®, Bracco SpA, Milan, Italy) to prime the epidural catheter, which was then fixed to the skin.
While the rabbits were placed in the lateral decubitus position, the necks were extended (extension group, n = 8) or flexed (flexion group, n = 8) until a slight resistance was felt. After fixing the neck to that position, the contrast medium was injected via an epidural catheter. The contrast medium was injected with the volume increasing by increments of 0.1 ml/ kg up to a maximum of 0.3 ml/kg. The cranial or caudal spread of contrast medium from the catheter tip was determined by counting the number of spinal bodies contacted by contrast medium using lateral epidurographic images acquired 30 sec after each injection, and the next injection followed immediately. Spread from the intervertebral level to the midline of the next vertebral body was counted as 0.5 vertebral body unit (VBU), and spread from one intervertebral level to the next was counted as 1 VBU.
Radiographic spread data were expressed as median (interquartile range) [range]. The Mann-Whitney Rank sum test was used to compare the spread between the groups. A P < 0.05 was considered statistically significant.
The epidural catheter tip was located at the T3-4 intervertebral level in all rabbits. Fig. 1 shows representative radiographs of the position of the neck.
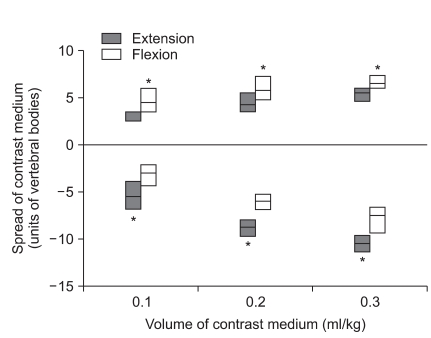
The cranial spread was greater in the flexion group than the extension group at the doses tested (Fig. 2) (P < 0.05). In the extension group, the median radiographic spread to the cranial direction was 3.5 VBU (2.6-3.5) [2.5-4.5], 4.3 VBU (3.5-5.5) [3.5-6.0], and 5.5 VBU (4.8-6.0) [4.0-6.5] at the doses of 0.1, 0.2, and 0.3 ml/kg, respectively. In the flexion group, median cranial spread was 4.5 VBU (3.6-5.8) [3.5-7.0], 5.8 VBU (5.0-7.0) [4.5-8.5], and 6.5 VBU (6.0-7.3) [5.0-8.5] at the doses of 0.1, 0.2, and 0.3 ml/kg, respectively.
On the contrary, caudal spread was greater in the extension group than the flexion group at the doses tested (Fig. 2) (P < 0.01). The median radiographic spread in the caudal direction was 6.0 VBU (5.0-6.9) [3.5-7.0], 8.8 VBU (8.0-9.5) [7.0-10.0], and 10.5 VBU (9.8-11.3) [9.0-11.5] at the doses of 0.1, 0.2, and 0.3 ml/kg, respectively. In the flexion group, median caudal spread was 3.0 VBU (2.6-4.4) [2.0-5.0], 6.0 VBU (5.5-6.8) [5.0-9.0], and 7.5 VBU (6.8-9.3) [5.5-11.0] at the doses of 0.1, 0.2, and 0.3 ml/kg, respectively.
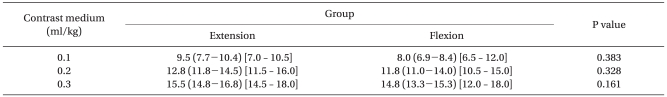
In the extension group, the contrast medium spread caudally about twice (1.7-2.1 times) as far as it spread cranially (P < 0.01). However, in the flexion group, there was no statistically significant difference between cranial and caudal spread. The total spread of the contrast medium was similar between the two groups at the doses tested (Table 1).
In this study, neck flexion increased cranial spread of contrast medium injected into the high thoracic epidural space in accordance with our previous report [14], and this spreading pattern was consistently shown at all the doses of contrast medium used. The total spread of contrast medium was similar between the two groups. At the lumbar level, spinal flexion increases the size of the spinal canal [16], and dorsal epidural pressure increases with neck extension, while decreasing with flexion [17]. It was also reported at the cervical level that the distance between the spinal cord and the posterior arch of the cervical canal is increased by neck flexion and decreased by neck extension [18]. Therefore, if cervical epidural pressure decreases with neck flexion and increases with neck extension, as lumbar epidural pressure does, cranial spread can be augmented by neck flexion and disturbed by neck extension, as shown in this study.
In contrast to the cranial spread, the caudal spread was augmented during the extension of the neck. However, in the previous human study, no difference was found in caudal spread during the different neck postures [14]. The reason for this discrepancy may be due to the different definitions of the neck extension. We may have hyperextended the neck, while in the previous study, neck extension was accomplished by asking the patients to tilt the head back until the face became vertically disposed to the trunk. Thus, the possible increase of the dorsal epidural pressure caused by the neck extension in our study could be more significant than that in the human study, so as to lead to more caudal spread. However, the possibility also exists that excessive neck flexion in the previous study may have decreased the drainage of jugular veins, which increases intracranial pressure and consequently, epidural pressure [19,20].
Various doses of local anesthetics can be injected into thoracic epidural space. A bolus of 2% lidocaine, 12-14 ml, for instance, was instilled into the high thoracic epidural space during the epidural anesthesia for the breast procedure [21,22]. Although there are many factors that may influence the spread in the epidural space, the volume of 14 ml is approximately 0.2 ml/kg for a body weight of 70 kg. In our study, contrast agents were administered up to 0.3 ml/kg. However, injecting an extremely large volume of contrast medium, of which viscosity is significantly higher than that of local anesthetics, might cause a transient pressure of the spinal cord [13]. Thus, we used an animal model in order to include large volume. The rabbit model was chosen for its adequate size, relative ease of its epidural puncture [23], and its comparable anatomy of rabbit cervical spine to that of the human [24]. Also, the previous epidural injection study using rabbit showed a similar spreading pattern to that of human when the injection sites were at the mid- or lower thoracic level [15].
This study might suggest that neck flexion may cause unintentional cervical block during high thoracic epidural anesthesia in clinical situations. However, because of the anatomic and physiologic factors, such as absorptive surface area-to-volume relationships and relative amounts of epidural adipose tissue [25], extreme caution is required to extrapolate the results from animal models to the human.
In conclusion, in the high thoracic epidural space of rabbit, the contrast medium administered in varying doses showed limited cranial spread during neck extension. The flexion of the neck increased cranial spread and extension of the neck increased caudal spread at all the doses of contrast medium used.
References
1. Hansdottir V, Philip J, Olsen MF, Eduard C, Houltz E, Ricksten SE. Thoracic epidural versus intravenous patient-controlled analgesia after cardiac surgery: a randomized controlled trial on length of hospital stay and patient-perceived quality of recovery. Anesthesiology. 2006; 104:142–151. PMID: 16394700.
2. Visser WA, Liem TH, Brouwer RM. High thoracic epidural anesthesia for coronary artery bypass graft surgery in a patient with severe obstructive lung disease. J Cardiothorac Vasc Anesth. 2001; 15:758–760. PMID: 11748529.

3. Royse C, Royse A, Soeding P, Blake D, Pang J. Prospective randomized trial of high thoracic epidural analgesia for coronary artery bypass surgery. Ann Thorac Surg. 2003; 75:93–100. PMID: 12537199.

4. Salvi L, Sisillo E, Brambillasca C, Juliano G, Salis S, Marino MR. High thoracic epidural anesthesia for off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2004; 18:256–262. PMID: 15232802.

5. Pennefather SH, Gilby S, Danecki A, Russell GN. The changing practice of thoracic epidural analgesia in the United Kingdom:1997-2004. Anaesthesia. 2006; 61:363–369. PMID: 16548957.
6. Usubiaga JE, Wikinski JA, Usubiaga LE. Epidural pressure and its relation to spread of anesthetic solutions in epidural space. Anesth Analg. 1967; 46:440–446. PMID: 4952222.
7. Hodgkinson R, Husain FJ. Obesity, gravity, and spread of epidural anesthesia. Anesth Analg. 1981; 60:421–424. PMID: 7195164.

8. Park WY. Factors influencing distribution of local anesthetics in the epidural space. Reg Anesth. 1988; 13:49–57.
9. Curatolo M, Orlando A, Zbinden AM, Scaramozzino P, Venuti FS. A multifactorial analysis of the spread of epidural analgesia. Acta Anaesthesiol Scand. 1994; 38:646–652. PMID: 7839771.

10. Higuchi H, Adachi Y, Kazama T. Factors affecting the spread and duration of epidural anesthesia with ropivacaine. Anesthesiology. 2004; 101:451–460. PMID: 15277929.

11. Kim JT, Lee JH, Yoon SZ, Lim YJ, Bahk JH, Kim CS, et al. Effect of lumbar flexion on the extent of epidural blockade. Reg Anesth Pain Med. 2007; 32:471–474. PMID: 18035291.

12. Visser WA, Liem TH, van Egmond J, Gielen MJ. Extension of sensory blockade after thoracic epidural administration of a test dose of lidocaine at three different levels. Anesth Analg. 1998; 86:332–335. PMID: 9459244.

13. Yokoyama M, Hanazaki M, Fujii H, Mizobuchi S, Nakatsuka H, Takahashi T, et al. Correlation between the distribution of contrast medium and the extent of blockade during epidural anesthesia. Anesthesiology. 2004; 100:1504–1510. PMID: 15166571.

14. Lee CJ, Jeon Y, Lim YJ, Bahk JH, Kim YC, Lee SC, et al. The influence of neck flexion and extension on the distribution of contrast medium in the high thoracic epidural space. Anesth Analg. 2007; 104:1583–1586. PMID: 17513662.

15. Kim YC, Lim YJ, Lee SC. Spreading pattern of epidurally administered contrast medium in rabbits. Acta Anaesthesiol Scand. 1998; 42:1092–1095. PMID: 9809094.

16. Fujiwara A, An HS, Lim TH, Haughton VM. Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biochemical study. Spine. 2001; 26:876–882. PMID: 11317109.
17. Takahashi K, Miyazaki T, Takino T, Matsui T, Tomita K. Epidural pressure measurements. Relationship between epidural pressure and posture in patients with lumbar spinal stenosis. Spine. 1995; 20:650–653. PMID: 7604339.
18. Muhle C, Wiskirchen J, Weinert D, Falliner A, Wesner F, Brinkmann G, et al. Biomechanical aspects of the subarachnoid space and cervical cord in healthy individuals examined with kinematic magnetic resonance imaging. Spine. 1998; 23:556–567. PMID: 9530787.

19. Yokoyama T, Ushida T, Yamasaki F, Inoue S, Sluka KA. Epidural puncture can be confirmed by the Queckenstedt-test procedure in patients with cervical spinal canal stenosis. Acta Anaesthesiol Scand. 2008; 52:256–261. PMID: 17999711.

20. Patel TR, Chiocca EA, Freimer ML, Christoforidis GA. Lack of epidural pressure change with neck flexion in a patient with Hirayama disease: case report. Neurosurgery. 2009; 64:E1196–E1197. PMID: 19487864.
21. Nesmith RL, Herring SH, Marks MW, Speight KL, Efird RC, Rauck RL. Early experience with high thoracic epidural anesthesia in outpatient submuscular breast augmentation. Ann Plast Surg. 1990; 24:299–302. PMID: 2101579.

22. Lynch EP, Welch KJ, Carabuena JM, Eberlein TJ. Thoracic epidural anesthesia improves outcome after breast surgery. Ann Surg. 1995; 222:663–669. PMID: 7487214.

23. Hughes PJ, Doherty MM, Charman WN. A rabbit model for the evaluation of epidurally administered local anaesthetic agents. Anaesth Intensive Care. 1993; 21:298–303. PMID: 8342758.

24. Wetzel FT, Panjabi MM, Pelker RR. Biomechanics of the rabbit cervical spine as a function of component transection. J Orthop Res. 1989; 7:723–727. PMID: 2760744.

25. Doherty MM, Hughes PJ, Korszniak NV, Charman WN. Prolongation of lidocaine-induced epidural anesthesia by medium molecular weight hyaluronic acid formulations: pharmacodynamic and pharmacokinetic studies in the rabbit. Anesth Analg. 1995; 80:740–746. PMID: 7893028.
Fig. 1
The position of the neck in the rabbits during the injection of contrast medium. The rabbits were placed in the lateral decubitus position, and the neck was extended (left) or flexed (right) until a slight resistance was felt. The arrows indicate epidural catheter.
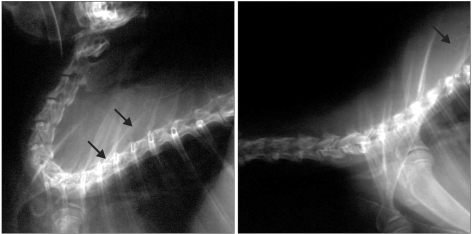
Fig. 2
Cranial and caudal spread of contrast medium in the high thoracic epidural space during extension or flexion of the neck. Cranial spread was greater in the flexion group, while caudal spread was greater in the extension group, *P < 0.05 versus the extension and flexion groups. Data are shown as box-and-whisker plots (10th percentile, 25th percentile, median, 75th percentile, 90th percentile). Cranial spread is expressed as positive values on the vertical axis, and caudal as negative values.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download