Abstract
An interscalene brachial plexus block is an effective means of providing anesthesia-analgesia for shoulder surgery. However, it has a multitude of potential side effects such as phrenic nerve block. We report a case of a patient who developed atelectasis of the lung, and pleural effusion manifested as chest discomfort during a continuous interscalene brachial plexus block for postoperative analgesia.
Shoulder surgery is commonly performed under an interscalene brachial plexus block (ISB) [1]. Hemidiaphragmatic paralysis occurs in 100% of patients with a single ISB [2] but is generally well tolerated in patients with a normal respiratory function. Patients given continuous ISB are also at risk of diaphragmatic paralysis [3-5].
We report a unique case of a patient who developed basal atelectasis of the right lung and pleural effusion, which manifested as chest discomfort, during continuous ISB for analgesia after shoulder arthroscopy.
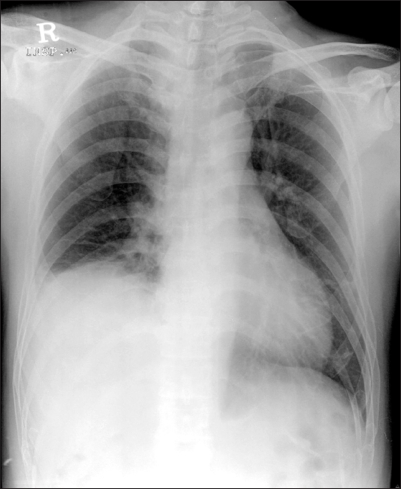
A 41-year-old man, 174 cm in height, weighing 72 kg, with American Society of Anesthesiologists (ASA) physical status I, was scheduled to under go right shoulder arthroscopy for rotator cuff repair under ISB. His prior medical history was unremarkable. He took no medication. A preoperative examination revealed there was equal air entry on both sides of his chest with no evidence of wheezing. All laboratory evaluations were within the normal limits, including electrocardiogram and chest roentgenogram (Fig. 1). He agreed to undergo regional anesthesia.
In the operating room, after applying routine monitors, his blood pressure, heart rate, respiratory rate and oxygen saturation was 130/80 mmHg, 70 beats/min, 16-18 breaths/min, and 99%, respectively. A right ISB was performed using the Borgeat's lateral modified approach. A nerve stimulator (Stimuplex®-DIG, B/Braun, Germany) connected to a 50 mm insulated Contiplex A needle and cannula (Contiplex® A, B/Braun, Germany) was used. After obtaining pectoralis major muscle twitching at a threshold of 0.5 mA, a 22-gauge catheter was inserted 5 cm through the cannula into the brachial sheath. Subsequently, 30 ml of 0.5% ropivacaine was injected slowly throgh the catheter. After continuous ISB, his vital signs were stable.
The patient was placed in a sitting "beach chair" position for surgery. Intraoperatively, he was sedated with sufentanil 10 µg and a propofol infusion at 50 µg/kg/min. Throughout the procedure, supplemental oxygen was given at 6 L/min through a mask. The operation and recovery room stay were uneventful and without complications.
After surgery, the patient was transported to the recovery room. The patient was pain free and comfortable. His blood pressure, heart rate, respiratory rate and oxygen saturation was 115/70 mmHg, 60 beats/min, 14 breaths/min, and 97%, respectively. 0.2% ropivacaine (Naropin®, AstraZeneca, Sweden) infusion was started in the recovery room through the interscalene catheter using a portable battery-powered pump (Accumate® 1,000, Wooyoung Medical, Korea) at a basal rate of 6 ml/h. The patient had the option of self administering a 3 ml bolus of 0.2% ropivacaine (with a 20-minute lock out time). The infusion was continued over the subsequent 2.5 days.
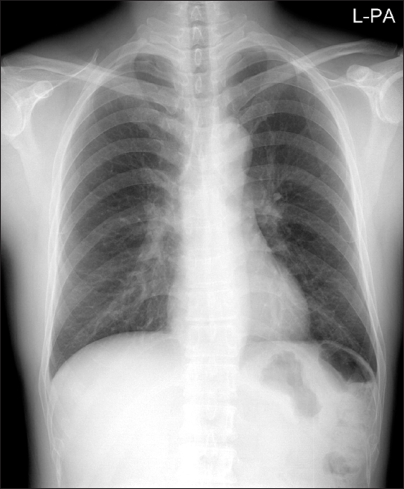
On the first postoperative day, the continuous ISB produced adequate analgesia (visual analogue scale, from 0-100 mm, was 40 mm), which avoided the need for additional analgesics. However, he reported mild chest discomfort. The chest x-ray revealed an elevation of the right hemidiaphragm, which was associated with basal atelectasis of the right lower lobe without pleural effusion (Fig. 2). The anesthetic team was not contacted.
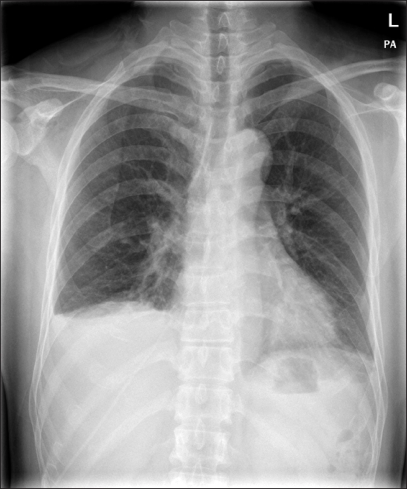
On the second postoperative day, he reported moderate chest discomfort that was on right side that was increased by deep inspiration. He was afebrile, and his blood pressure, heart rate and respiratory rate was 110/80 mmHg, 70 beats/min, and 20 breaths/min, respecively. The physical cardiopulmonary examination was normal. The chest x-ray revealed an elevation of the right hemidiaphragm associated with basal atelectasis of the right lower lobe, and pleural effusion without pneumothorax (Fig. 3). The chest CT revealed the same findings. No signs of infection or other disorders were shown on the film. This pattern was suggestive of acquired phrenic nerve palsy. Arterial blood gas analysis was within the normal limits. The local anesthetic infusion was discontinued. Before discontinuing the local anesthetic, his pain was well controlled (visual analogue scale, from 0-100 mm, was 20 mm). There were no change in the vital signs after discontinuing the continuous ISB. Patients received oral lornoxicam 4 mg three times a day on a regular basis. Rescue analgesia with 60 mg of IM diclofenac was available on demand.
On the fourth postoperative day, his symptoms appeared to have improved but the chest x-ray showed no improvement. Although the right hemidiaphragm had returned to normal, the chest x-ray on the sixth postoperative day showed residual pleural effusion and atelectasis. He was discharged on the eighth postoperative day.
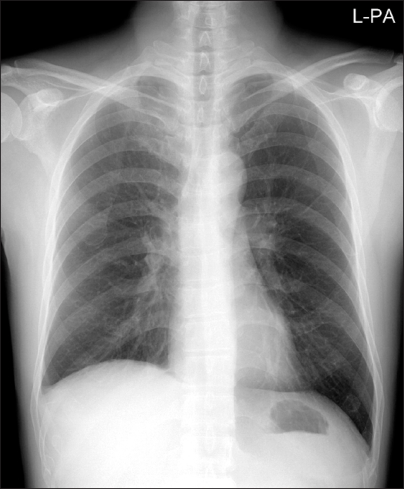
On the fifteenth postoperative day, the chest x-ray showed complete expansion of the collapsed right lower lobe (Fig. 4).
The 100% incidence of short-term hemidiaphragmatic paresis reported in patients undergoing ISB has been related to the spread of the local anesthetic solution, either on the C3-C5 roots or through the scalene anterior fascia. No prophylactic measure has been found to decrease the incidence of phrenic nerve block after a single-shot ISB. This is not prevented by digital pressure and occurs with a variety of local anesthetics and doses. Impairment of diaphragmatic movements can be rated from 50% to 77% for supraclavicular [6,7], 24% to 26% for proximal infraclavicular [8], and 0% for more distal infraclavicular blocks [9,10].
Paresis of one hemidiaphragm is not normally associated with adverse clinical symptoms, even though the lung volume, pulmonary function tests, and arterial blood gas analyses are all adversely affected. A normal individual can compensate for these changes by utilizing the accessory and intercostal muscles and enhanced respiratory effort. However ISB can lead to acute respiratory failure in patients with chronic respiratory disease or with preexisting contralateral phrenic nerve paralysis, and is contraindicated in such patients [11-13].
Patients undergoing continuous ISB are also at risk of diaphragmatic paresis. During continuous ISB, the paresis can occur as high as 75% of cases and often persists until the end of the infusion [3,4]. In contrast to single-shot ISB, continuous ISB producing long-duration phrenic nerve block is more likely to induce prolonged hemidiaphragmatic paresis and hypoventilation. The atelectasis of the right lower lobe caused by a prolonged phrenic nerve block can lead to the formation of a plural effusion.
In our case, the relationship between the phrenic nerve block and the pleural effusion was not obvious at first. On the first postoperative day, the chest x-ray revealed an elevation of the right hemidiaphragm associated with basal atelectasis of the right lower lobe, but no pleural effusion. However, on the second postoperative day, the chest x-ray showed an elevation of the right hemidiaphragm associated with basal atelectasis of the right lower lobe and pleural effusion. It was assumed that the atelectasis and pleural effusion on the same side of the continuous ISB was due to a phrenic nerve block. The rapid resolution of both clinical and radiologic signs after discontinuing the continuous ISB supports this hypothesis. Souron et al. [14] reported a patient who developed atelectasis of the lung and pleural effusion revealed by chest pain after continuous ISB. Sardesai et al. [15] also reported a case of left lower lobe collapse after interscalene local anesthetic infusion administered at home. As in our case, the treatment is to stop the local anesthetic first and check the chest x-ray regularly.
In conclusion, during continuous ISB, chest discomfort can indicate pleural effusion secondary to an ipsilateral phrenic nerve block, even in patients with a normal preoperative respiratory function. It is recommended that a chest x-ray be acquired rapidly to identify this uncommon complication and exclude a pneumothorax.
References
2. Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg. 1991; 72:498–503. PMID: 2006740.

3. Tuominen M, Tarkkila P. Diaphragmatic motion during continuous interscalene brachial plexus block. Reg Anesth. 1995; 20:543–544. PMID: 8608075.
4. Pere P, Pitkanen M, Rosenberg PH, Bjorkenheim JM, Linden H, Salorinne Y, et al. Effect of continuous interscalene brachial plexus block on diaphragm motion and on ventilatory function. Acta Anaesthesiol Scand. 1992; 36:53–57. PMID: 1539480.

5. Borgeat A, Perschak H, Bird P, Hodler J, Gerber C. Patient-controlled interscalene analgesia with ropivacaine 0.2% versus patient-controlled intravenous analgesia after major shoulder surgery: effects on diaphragmatic and respiratory function. Anesthesiology. 2000; 92:102–108. PMID: 10638905.
6. Mak PH, Irwin MG, Ooi CG, Chow BF. Incidence of diaphragmatic paralysis following supraclavicular brachial plexus block and its effect on pulmonary function. Anaesthesia. 2001; 56:352–356. PMID: 11284823.

7. Neal JM, Moore JM, Kopacz DJ, Liu SS, Kramer DJ, Plorde JJ. Quantitative analysis of respiratory, motor, and sensory function after supraclavicular block. Anesth Analg. 1998; 86:1239–1244. PMID: 9620512.

8. Rettig HC, Gielen MJ, Boersma E, Klein J, Groen GJ. Vertical infraclavicular block of the brachial plexus: effects on hemidiaphragmatic movement and ventilatory function. Reg Anesth Pain Med. 2005; 30:529–535. PMID: 16326337.

9. Rodriguez J, Barcena M, Rodriguez V, Aneiros F, Alvarez J. Infraclavicular brachial plexus block effects on respiratory function and extent of the block. Reg Anesth Pain Med. 1998; 23:564–568. PMID: 9840851.
10. Dullenkopf A, Blumenthal S, Theodorou P, Roos J, Perschak H, Borgeat A. Diaphragmatic excursion and respiratory function after the modified Raj technique of the infraclavicular plexus block. Reg Anesth Pain Med. 2004; 29:110–114. PMID: 15029545.

11. Smith MP, Tetzlaff JE, Brems JJ. Asymptomatic profound oxyhemoglobin desaturation following interscalene block in a geriatric patient. Reg Anesth Pain Med. 1998; 23:210–213. PMID: 9570613.

12. Hashim MS, Shevde K. Dyspnea during interscalene block after recent coronary bypass surgery. Anesth Analg. 1999; 89:55–56. PMID: 10389778.

13. Gentili ME, Lefoulon-Gourves M, Mamelle JC, Bonnet F. Acute respiratory failure following interscalene block: complications of combined general and regional anesthesia. Reg Anesth. 1994; 19:292–293. PMID: 7947432.
14. Souron V, Reiland Y, Delaunay L. Pleural effusion and chest pain after continuous interscalene brachial plexus block. Reg Anesth Pain Med. 2003; 28:535–538. PMID: 14634945.

15. Sardesai AM, Chakrabarti AJ, Denny NM. Lower lobe collapse during continuous interscalene brachial plexus local anesthesia at home. Reg Anesth Pain Med. 2004; 29:65–68. PMID: 14727282.

Fig. 2
Chest x-ray on the first postoperative day showing an elevation of the right hemidiaphragm, associated with a basal atelectasis of the right lower lobe, but no pleural effusion.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download