Abstract
Thoracic outlet syndrome has neurologic symptoms caused by compression of brachial plexus, blood vessel symptoms are caused by compression of the artery or vein. The authors report a case of sudden decrease in blood pressure of the left arm after turning the patient from supine position to prone position. They confirmed that the patient had thoracic outlet syndrome after performing computed tomography.
Thoracic outlet syndrome (TOS), first reported by Paget (1875), is a disorder produced by compression of the components of brachial plexus and blood vessels caused by congenital anomaly, or hypertrophy or trauma on the scalenus in a triangular space formed by the first rib, the clavicle, and a superior margin of the scapula [1]. The subtypes of this disorder are referred to as arterial TOS, venous TOS, or neurologic TOS according to affected structures. The clinical symptoms include neurologic symptoms and blood vessel symptoms caused by compression at the brachial plexus and at the subclavian arteries and veins, respectively [2].
The authors experienced a decline in blood pressure in the left upper limb and an extreme difference in the blood pressure between the bilateral upper limbs during the operation after turning the patient from a supine position to a prone position after anesthesia, while we detected positive signs for TOS in Angio Computed Tomography.
A 12-year-old, 161 cm, 32 kg, female patient with idiopathic scoliosis in the thoracic vertebra presented for posterior fusion operation. She had no significant medical issues and was not taking any medication. Blood tests before the operation were in the normal range, and no abnormalities except for idiopathic scoliosis were found on the simple chest X-ray. X-rays on the vertebrae revealed severe scoliosis from the fifth thoracic vertebra to the first lumbar vertebra. Prior to anesthesia, atropine 0.3 mg was administrated. Before anesthesia, the pulse oximetry was 100% and the blood pressure was 120/79. The induction of anesthesia included administration of propofol 50 mg and succinylcholine 40 mg, followed by a catheterization. The anesthesia was maintained with N2O 2 L/min, O2 2 L/min, desflurane 5%, atracurium 15 mg. To check collateral circulation in the left hand before the induction of anesthesia, Allen's test was performed, and by inserting a 22 G catheter into the left radial artery, arterial pressure was measured. When a monitoring catheter was inserted into the right internal jugular vein, the central venous pressure was 10 mmHg.
For the surgery, the patient was turned from a supine position to a prone position, and then her shoulder joints were abducted at 120° and the elbow joints were flexed at 70° while the neck was maintained in neutral position.
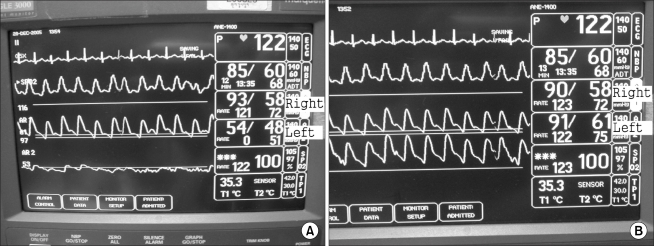
After the transition in position, the blood pressure indicated 100/60 mmHg and the central venous pressure was 10 mmHg, showing no change. However, the systolic blood pressure dropped from 90 to 40 mmHg while inserting an introducer needle after skin incision and muscle dissection. We suspected damage in great vessels and checked the operative field after consulting the surgeon, but not a significant bleeding was observed. The blood loss had amounted to about 500 ml, so 6% hydroxyethyl starch (HES) 500 ml (Salinhes®, Ilsung pharmaceuticals, Korea) was administrated in order to complement the volume in the vessels, and the urine was 90 ml, and the central venous pressure was maintained at 9 mmHg or so. While the operation was ceased, the systolic blood pressure was restored to 90 mmHg. When the operation was resumed, the systolic blood pressure repeatedly dropped back to 40 mmHg. Despite the sudden drop in the arterial pressure, no bleeding was found in the operative field, so we suspected blood pressure lowering caused by the reduction in venous return and cardiac output owing to a pressure on the inferior venacava resulted from a pressure on the vertebrae during the spine surgery. As the surgeon applied a compressing force to the surgical region with the same intensity as in usual surgical process in order to confirm such possibility, a drop close to the previous one was detected. The difference between compressing and not compressing on the region was 40-50 mmHg in the systolic blood pressure, but the central venous pressure was 9 mmHg, not showing much change while the arterial pressure was changing. Then, the possibility of the blood pressure reduction due to such causes was ruled out. While repeating the same process, the arterial pressure was measured at the right upper arm region by a automated noninvasive blood pressure device when the blood pressure in the left radial artery decreased, but the blood pressure did not change when compressing force was applied to the vertebrae. Then, to make a more exact comparison, a monitoring catheter was inserted into the right radial artery. Despite a series of repeated compressing that triggers a drop in the left radial arterial pressure, the blood pressure in the right radial artery did not show a significant change, while the systolic pressure in the left radial artery was lower than in the right one by 40-50 mmHg (Fig. 1). Suspecting a disease responsible for reducing blood flow in the left upper arm, we monitored the blood pressure in the right radial artery. The blood pressure at the radial artery in the left upper limb decreased every time there was a pressing force applied to the surgical site, but the surgery was resumed with close observation because the pulse oximetry on the left middle finger was maintained 100% and no abnormalities except for the blood pressure decline were observed. Thereafter, the surgery was finished without any particular incident and the patient was turned from the prone to the supine position for awakening. After the repositioning, the left radial artery pressure was restored to a similar level to that of the right one and the difference of the systolic blood pressure in the two limbs remained within 5 mmHg. The total length of the surgery was 3 hours and 50 minutes and the anesthesia lasted 5 hours and 15 minutes.
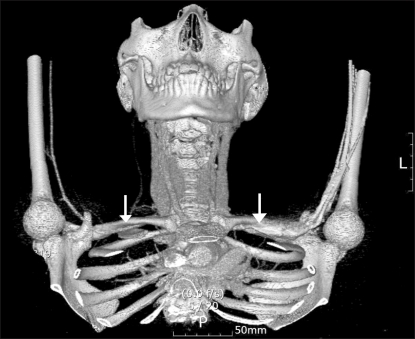
The patient was transported to the postanesthetic recovery unit after awakening, and on postoperative day 8, Roos' test was performed to confirm thoracic outlet syndrome. The test revealed a decrease in vascular tone and paleness in the left upper limb. There was no dysesthesia, but she complained about uncomfortable feeling in the left upper limb. On postoperative day 10, an Angio Computed Tomography found that the first rib and the clavicle compressed the right subclavian artery at the same position as in the operation, so we diagnosed her case with TOS (Fig. 2). The blood pressure at the supine position after the operation showed just insignificant difference between the bilateral upper limbs and there was no reproduction of the symptoms that she had felt. Then on postoperative day 18, she was discharged home under follow-up medical observation.
Blood Pressure is one of the principal signs to evaluate the status of cardiovascular system in patients during anesthesia or operation, and it plays a role of the base for clinical decisions about tissue perfusion. The normal differences in blood Pressure between the right and left upper limbs are -9 mmHg-11 mmHg in the systolic pressure and -10 mmHg-10 mmHg in the diastolic pressure [3]. Disorders that show abnormality in differences between left and right arm blood Pressure measurements include aortic dissection, peripheral vascular disease due to atherosclerosis, TOS, etc [4].
TOS is a disorder produced by compression of the components of nerves and blood vessels at the thoracic outlet. The involved structures are the first rib, the clavicle, the scapula, etc. Neurologic symptoms occur in 95% of cases, while 3% of cases represent compression at the subclavian vein and 1% at the subclavian artery [5]. The neurologic symptoms involve pain in the upper arm, dysesthesia, weakness, while the compression at the vein shows swelling of the arm, cyanosis, and pain. The cases of compression at the artery usually involve ischemia, dysesthesia, discolorization, coldness, etc [5].
The patient in this study is a case of the arterial TOS among the three subtypes of TOS, in whom there were no symptoms of compression of nerves or blood vessels, and no abnormalities of ischemia or loss of palpable pulse in the left upper limb at the supine position was observed after the anesthesia, while sudden blood pressure took place when her back was compressed with the shoulder joints abducted and the elbow joints flexed. The position is similar to that of Roos' test, which is a physical examination used for the diagnosis for TOS. The Roos' test is considered positive for a decrease in pulse and the arterial pressure in case of TOS patients [5].
To perform this test, the patient raises both arms and have the arms abducted 90° from the thorax and the elbows flexed 90°. The patient then opens and closes the hands slowly for three minutes. Normal people would complain a minor uncomfortableness, but patients with TOS experience being unable to keep the arms in the starting position due to pain in the neck and shoulders, ischemic pain in the forearm, and pallor or congestion in the arms [6].
Inoue [7] found edema in the left upper limb in a patient, who underwent a surgery for brain tumors at the prone position, right after the operation and diagnosed his case with TOS. Mouton et al. [8] reported, when a patient with temporal Arterio-venous malformation was turned from a supine position to a left lateral recumbent position, the waveform of the right radial artery pressure disappeared and pallor, coolness, and loss of pulse were observed in the right upper limb. A Doppler ultrasound test found that the subclavian artery was obstructed at the thoracic outlet, but they finished the operation with taking the patient to a position without obstructing the artery after careful efforts in changing positions.
In this case, massive hemorrhage was not observed in the surgical site and there was no dramatic change in the central venous pressure when the arterial pressure decreased. Therefore, we were able to rule out the injury of great vessels or the decrease of venous return owing to compression at the inferior vena cava from possible causes of the blood pressure decrease. Thereafter, in order to seek the causes of repetitive decrease in the blood pressure, we watched the arterial pressure in both of the bilateral upper limbs and detected the pressure difference between them, which leaded us to suspect an anomaly of vessels in the left upper limb.
As this case has shown, when a sudden decrease in blood pressure occurs during operation, it is required to check the amount of hemorrhage in the surgical site at first, and to measure and compare the blood pressure of the bilateral limbs and then to be suspicious of several possible disorders if there are no findings on the causes inducing an abrupt decrease in the blood pressure such as anaphylactic shock. Also, if a blood pressure decrease occurs according to a change in position, adjustment in position should be made for relieving compression and if such effort of repositioning does not produce a desirable effect, it is necessary to consult the surgeon to modulate the degree of compression on the vessels and to reach a decision for the operation. During the operation, close observation should be kept on the affected upper limb.
References
1. The Korean Orthopaedic Association. Orthopaedics. 2006. 6th. Seoul: Newest medicine company;p. 495.
2. Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist. 2008; 14:365–373. PMID: 19008742.
3. Orme S, Ralph SG, Birchall A, Lawson-Matthew P, McLean K, Channer KS. The normal range for inter-arm differences in blood pressure. Age Ageing. 1999; 28:537–542. PMID: 10604505.

4. Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006; 20:923–931. PMID: 17036043.

5. Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vasc Surg. 2007; 46:601–604. PMID: 17826254.

6. Brantigan CO, Roos DB. Diagnosing thoracic outlet syndrome. Hand Clin. 2004; 20:27–36. PMID: 15005381.

7. Inoue S. Thoracic outlet syndrome and anaesthestic problems. Acta Anaesthesiol Scand. 2004; 48:136. PMID: 14674987.
8. Mouton R, Oliver C, Shinde S. Thoracic outlet obstruction during neurosurgical positioning. Anaesthesia. 2008; 63:1151–1152. PMID: 18821907.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download