1. Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P. Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology. 1998; 89:1313–1321. PMID:
9856704.

2. Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000; 162:134–138. PMID:
10903232.

3. Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001; 92:984–989. PMID:
11273937.

4. Heenen S, De Backer D, Vincent JL. How can the response to volume expansion in patients with spontaneous respiratory movements be predicted? Crit Care. 2006; 10:R102. PMID:
16846530.
5. Soubrier S, Saulnier F, Hubert H, Delour P, Lenci H, Onimus T, et al. Can dynamic indicators help the prediction of fluid responsiveness in spontaneously breathing critically ill patients? Intensive Care Med. 2007; 33:1117–1124. PMID:
17508201.

6. Shyr MH, Yang CH, Tan PP, Chan SH. Power spectral analysis of arterial and central venous pressure signals during graded hemorrhage in anesthetized rats. Shock. 1999; 11:187–192. PMID:
10188771.

7. Lai HY, Yang CC, Huang FY, Lee Y, Kuo YL, Kuo TB. Respiratory-related arterial pressure variability as an indicator of graded blood loss: involvement of the autonomic nervous system. Clin Sci. 2003; 105:491–497. PMID:
12817986.

8. Egi A, Kawamoto M, Kurita S, Yuge O. Systolic arterial pressure variability reflects circulating blood volume alterations in hemorrhagic shock in rabbits. Shock. 2007; 28:733–740. PMID:
17621261.

9. Kim TH, Kang SJ, Sang BH, Shin WJ, Kim YK, Hwang GS, et al. Effects of magnesium infusion on hemodynamic and autonomic changes in healthy volunteers. Korean J Anesthesiol. 2008; 55:691–699.

10. Cho SK, Hwang GS, Kim YK, Huh IY, Hahm KD, Han SM. Low-dose atropine amplifies cardiac vagal modulation and increases dynamic baroreflex function in humans. Auton Neurosci. 2005; 118:108–115. PMID:
15795184.

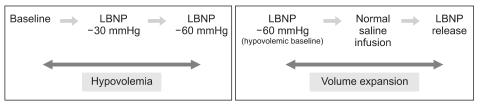
11. Cooke WH, Ryan KL, Convertino VA. Lower body negative pressure as a model to study progression to acute hemorrhagic shock in humans. J Appl Physiol. 2004; 96:1249–1261. PMID:
15016789.

12. Penaz J. Criteria for set point estimation in the volume clamp method of blood pressure measurement. Physiol Res. 1992; 41:5–10. PMID:
1610779.
13. Wesseling KH, Jansen JR, Settels JJ, Schreuder JJ. Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol. 1993; 74:2566–2573. PMID:
8335593.

14. Leonetti P, Audat F, Girard A, Laude D, Lefrere F, Elghozi JL. Stroke volume monitored by modeling flow from finger arterial pressure waves mirrors blood volume withdrawn by phlebotomy. Clin Auton Res. 2004; 14:176–181. PMID:
15241646.

15. Akselrod S, Gordon D, Madwed JB, Snidman NC, Shannon DC, Cohen RJ. Hemodynamic regulation: investigation by spectral analysis. Am J Physiol. 1985; 249:H867–H875. PMID:
4051021.

16. Pagani M, Lucini D, Rimoldi O, Furlan R, Piazza S, Porta A, et al. Low and high frequency components of blood pressure variability. Ann N Y Acad Sci. 1996; 783:10–23. PMID:
8853630.

17. Kawase M, Komatsu T, Nishiwaki K, Kobayashi M, Kimura T, Shimada Y. Heart rate variability and arterial blood pressure variability show different characteristic changes during hemorrhage in isoflurane-anesthetized, mechanically ventilated dogs. Anesth Analg. 2002; 94:16–21. PMID:
11772794.

18. Brychta RJ, Shiavi R, Robertson D, Biaggioni I, Diedrich A. A simplified two-component model of blood pressure fluctuation. Am J Physiol Heart Circ Physiol. 2007; 292:H1193–H1203. PMID:
17012354.

19. Toska K, Eriksen M. Respiration-synchronous fluctuations in stroke volume, heart rate and arterial pressure in humans. J Physiol. 1993; 472:501–512. PMID:
8145156.

20. Siebert J, Drabik P, Lango R, Szyndler K. Stroke volume variability and heart rate power spectrum in relation to posture changes in healthy subjects. Med Sci Monit. 2004; 10:MT31–MT37. PMID:
14737053.
21. Pinna GD, Maestri R, Mortara A, La Rovere MT. Cardiorespiratory interactions during periodic breathing in awake chronic heart failure patients. Am J Physiol Heart Circ Physiol. 2000; 278:H932–H941. PMID:
10710362.
22. Cooke WH, Cox JF, Diedrich AM, Taylor JA, Beightol LA, Ames JE 4th, et al. Controlled breathing protocols probe human autonomic cardiovascular rhythms. Am J Physiol. 1998; 274:H709–H718. PMID:
9486278.
23. Lee K, Picard G, Beske SD, Hwang GS, Taylor JA. Effects of fitness and age on the response to vagotonic atropine. Auton Neurosci. 2008; 139:60–67. PMID:
18321791.

24. Monge Garcia MI, Gil Cano A, Diaz Monrove JC. Arterial pressure changes during the Valsalva maneuver to predict fluid responsiveness in spontaneously breathing patients. Intensive Care Med. 2009; 35:77–84. PMID:
18830578.

25. Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med. 2007; 33:1125–1132. PMID:
17508199.

26. De Backer D, Pinsky MR. Can one predict fluid responsiveness in spontaneously breathing patients? Intensive Care Med. 2007; 33:1111–1113. PMID:
17508200.

27. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996; 93:1043–1065. PMID:
8598068.
28. Convertino VA, Ludwig DA, Cooke WH. Stroke volume and sympathetic responses to lower-body negative pressure reveal new insight into circulatory shock in humans. Auton Neurosci. 2004; 111:127–134. PMID:
15182742.

29. Goswami N, Loeppky JA, Hinghofer-Szalkay H. LBNP: past protocols and technical considerations for experimental design. Aviat Space Environ Med. 2008; 79:459–471. PMID:
18500042.

30. Jansen JR, Schreuder JJ, Mulier JP, Smith NT, Settels JJ, Wesseling KH. A comparison of cardiac output derived from the arterial pressure wave against thermodilution in cardiac surgery patients. Br J Anaesth. 2001; 87:212–222. PMID:
11493492.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download