Introduction
In general anesthesia, endotracheal intubation is used to secure the airway passage. When intubation using laryngoscopy is difficult or when one wants to reduce hemodynamic changes caused by it, a supraglottic airway device (SGA) may be used instead. The best known SGA is the laryngeal mask airway (LMA). Unfortunately it has a low sealing pressure. It can therefore cause inadequate ventilation and gastric distension during positive ventilation, and carries a risk of pulmonary aspiration in the event of regurgitation [
1]. Many devices have been developed to minimize these drawbacks. One of the most commonly used SGAs is the laryngeal mask airway ProSeal™ (PLMA, Laryngeal Mask Company, UK), a modified version of the classic LMA with an additional channel for gastric tube placement to prevent pulmonary aspiration and a superior cuff that can provide airway sealing pressures higher than those of the classic LMA [
1].
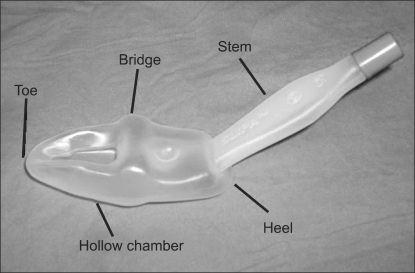
The newly developed SLIPA™ (stream lined liner of pharyngeal airway™, SLIPA Medical Ltd., UK) is replacing the LMA in general anesthesia. It is made of soft plastic in ananatomical shape which sticks to the pharynx and palate. It therefore does not require cuff inflation and extra straps to maintain a secure airway during positive pressure ventilation. Furthermore, a 50 ml empty internal space allows the removal of pharyngeal secretions, thus reducing the risk of pulmonary aspiration [
2] (
Fig. 1). Also, it can be inserted without the need for other devices, and as it is designed for single-use at a relatively cheaper price than the LMA, it has a lower risk of infection [
3].
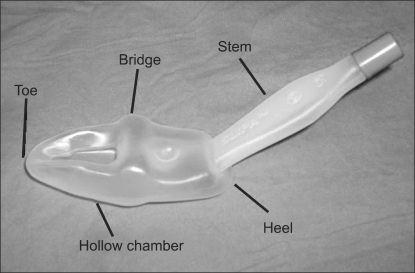 | Fig. 1The SLIPA in detail. The SLIPA is made of soft hollow plastic. Because the SLIPA resembles the anatomy of the pharynx, an inflatable cuff is unnecessary. Instead, the body serves as a reservoir for regurgitated liquids. 
|
While there has been much clinical research (in Korea and elsewhere) on other SGAs, there has, especially in Korea, been little study on the SLIPA. Also, there is as of yet no comparative research on SLIPA and PLMA.
In the present study, we compared the use of the PLMA and SLIPA during general anesthesia in regard to their first insertion success rate, ease of use, hemodynamic responses to insertion, ventilatory efficiency and postoperative complications. We also evaluated the clinical effectiveness of each method.
Go to :

Materials and Methods
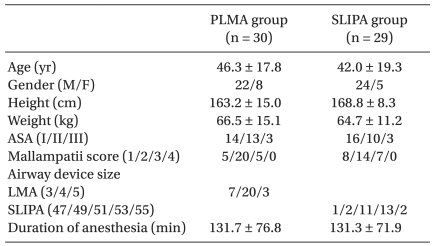
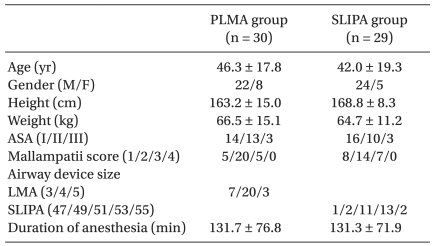
The 60 patients chosen for the study were ASA class I-III, were between the ages 12-75 years, and were undergoing elective surgery under general anesthesia. Excluded from the study were: patients with a history of diabetes mellitus, morbid obesity, gastroesophageal reflux, and pregnancy, patients at risk of pulmonary aspiration, and patients electing for surgery in the non-supine position. After receiving the approval of the hospital's ethics committee, all patients gave written informed consent. The patients were randomly divided into the SLIPA and PLMA groups with 30 patients in each. Randomization was based on Microsoft Excel random number generation. Patient group allocation was not revealed to investigator until immediately prior to induction of anesthesia by means of numbered, sealed envelopes. The two groups were comparable with respect to gender, age, height, weight, ASA classification, modified Mallampati classification, and the duration of anesthesia (
Table 1). To evaluate the airway, the modified Mallampati classification was recorded at preanesthetic evaluation.
Table 1
Demographics Data and Duration of Anesthesia

In the PLMA group, size 3 was used for patients weighing below 50 kg, size 4 for those weighing 50-70 kg, and size 5 for those over 70 kg. After insertion, the cuff pressure was maintained at 60 cmH2O with a hand pressure gauge (VBM, Germany). In the female SLIPA group, size 47 was used for patients under 155 cm in height, size 49 for those between 155-165 cm, and size 51 for those over 165 cm. In the male SLIPA group, size 51 was used for patients less than 165 cm in height, size 53 for those between 165-175 cm, and size 55 for those over 175 cm.
Thirty minutes before being taken to the operating room, the patients were given muscular injections of glycopyrolate 0.2 mg as a preanesthetic medication. In the operating room, an electrocardiogram, a noninvasive arterial blood pressure cuff, and a pulse oximeter were attached for monitoring. Anesthetic induction was achieved by fentanyl 2 µg/kg, thiopental sodium 5 mg/kg and rocuronium 0.6 mg/kg. After 2 minutes of controlled positive pressure, ventilation by N2O/O2 each 1.5 L/min and sevoflurane 2.0 vol%, the same anesthesiologist placed the PLMA or SLIPA for all the patients. The anesthesiologist had 2 years experience with using the PLMA and had used the SLIPA 20 times before the present study. Normal saline was used for lubrication. When the first attempt failed, mask ventilation was performed for 1 minute and a second attempt was made with a different size. If that also failed, then the patient was excluded from the study, and the surgery was performed by endotracheal intubation. In the process of insertion, the insertion duration (from the point of starting placement to the point of successful mechanical ventilation), and the number of insertion attempts were measured. The level of difficulty of insertion (easy, moderate, difficult) was noted subjectively by the anesthesiologist who inserted the device.
The same anesthetic machines (Astiva/5, Datex-Ohmeda Inc., USA) were used throughout the study. Ventilation during the anesthesia was performed with a tidal volume of 10 ml/kg, respiratory rate of 12/min and the inspiratory: expiratory ratio was 1 : 2.
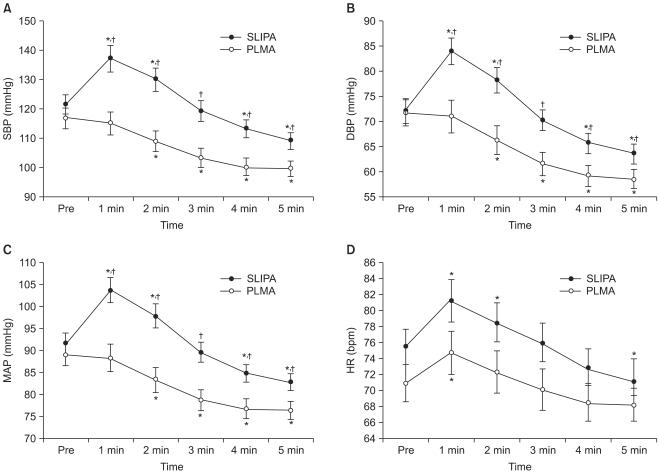
To assess the hemodynamic response to insertion of the device, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP), and heart rate (HR) were recorded 5 minutes before and after the insertion at 1 minute intervals. The maximal change in mean value (%) was calculated by the ratio of the mean value immediately before insertion to the highest mean value immediately after insertion. During insertion, if the blood pressure decreased by more than 20% of the blood pressure measured in the ward, ephedrine 5 mg was administered.
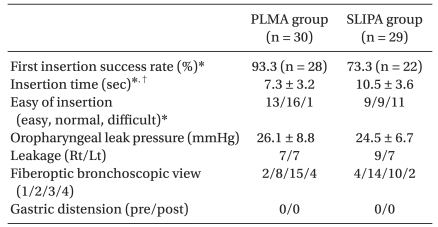
To evaluate if the airway was appropriately secured, the head was rotated 60 degrees to the right and left to see if there was any leakage. Also, oral leak pressure (OLP) was measured as the highest peak reached when the airway pressure measured in the anesthetic circuit by a pressure gauge did not rise anymore when the mechanical ventilation was stopped, the pop-off valve locked, and fresh gas flow 3 L/min supplied [
4]. Using a fiberoptic bronchoscope (Olympus BF-3C40, Olympus optical co., Japan), hypopharynx placement was scored as follows: only vocal cords seen, 4 points; vocal cords and back of the epiglottis seen, 3 points; vocal cords and front of epiglottis seen, 2 points; vocal cords not seen, 1 point [
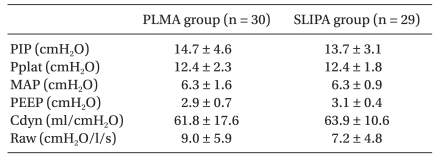
5]. At the beginning and end of ventilation, gastric distension was checked for with a stethoscope and the naked eye. 10 minutes after the insertion, a spirometer module (S/5 Compact anesthesia monitor™, Datex-Ohmeda, USA) was used to measure the maximum inspiratory pressure, plateau airway pressure (Pplat), mean airway pressure (MAP), peak end expiratory pressure (PEEP), airway resistance (Raw), and compliance (Cdyn). The spirometer module was attached to the patient's airway device as a side stream which allowed for extraction of respiratory gas. After the initial evaluation, the mid-surgery tidal volume and respiratory rate were controlled to achieve an end tidal carbon dioxide value of 35-40 mmHg.
After the surgery, the airway device was removed and evidence of blood stains or regurgitation checked for. In the recovery room, one anesthesiologist, who did not know which group the patient belonged to, evaluated the postoperative sore throat pain on the visual analogue scale (VAS score, 0-10) and checked for other complications.
To calcluate the sample size required for this study, time taken for intubation in a similar clinical setting was taken account [
3]. A two-tailed α error of 5% and a β error of 20% was accepted in the detection of differences of 4 second in the time taken for intubation between the two groups. Based on this calculation, the required size per group was 30.
Normally distributed data were compared between groups by unpaired t-testing, and presented as mean value ± standard deviation and presents mean value ± standard error in the figure. Descriptive variables were analyzed, as appropriate, by Chi-square test or Fischer's exact test. The blood pressures and heart rates between groups were compared using two way repeated measures ANOVA. Within a group, comparison with the base data was performed by one way repeated measures ANOVA. P values less than 0.05 were considered statistically significant, and statistical analysis was performed with Sigmastat (version 2.03, SPSS Ins., USA).
Go to :

Discussion
An SGA is relatively easier to insert than an endotracheal tube and they are considered for patients in whom intubation is difficult, or for patients in emergency situations [
6]. Markus et al. [
7] compared classic LMA and SLIPA and had first insertion success rates of 100% and 98% respectively. Similarly, Miller et al. [
8] reported first insertion success rates for PLMA and SLIPA of 96% and 98% respectively. In the present study, the first insertion success rates for PLMA and SLIPA were 93.3% and 73.3% respectively. When the first attempt failed, all second attempts were successful in the PLMA group. Both attempts were unsuccessful in one patient in the SLIPA group. Unlike the PLMA, which achieves a pharyngeal seal through post-insertion cuff inflation, the SLIPA comes in a fixed preformed shape. Correct size selection is therefore important for successful SLIPA insertion. In the present study, most first attempt failures were due to inappropriate size selection. When chosen correctly, the second attempt was successful. Previous studies outside of Korea [
2,
3,
7,
8] selected SLIPA size by matching the transverse diameter with the patient's thyroid cartilage. However, in our pilot tests, the SLIPA size chosen by this method was too large and insertion failed in many cases. We therefore tried the size-rule provided by the SLIPA manufacturer, which involved gender and height. However, this rule was too wide range and selection areas often overlapping. It was thus difficult to select the right size on the first attempt. To improve the first attempt success rate, development of SLIPA selection guidelines for Asians is clearly needed. We plan to develop such guidelines in the future.
In the present study, compared to PLMA insertion, SLIPA insertion took longer and was more difficult. We assume this is due to both our relative lack of experience with SLIPA and the difficulty of selecting an appropriate size. Malik et al. [
9] found that inexperienced medical students who used Macintosh laryngoscopes for endotracheal intubation had a slow learning curve. It took them a long time to reach a competent level of maneuvering and this signifies that in times of emergency, endotracheal intubation can fail or can cause complications. In contrast, according to the research of Reinhart et al. [
10], the LMA (the most common SGA) has a shorter insertion time, higher success rate on the first attempt, and greater ease of use than endotracheal intubation. In a study on medical students with no experience of the SLIPA, SLIPA success rates and preference rates were higher than those of SS-LMs (soft seal laryngeal masks) and the SLIPA had a shorter insertion time [
11]. Inaddition, because it did not require extra handling like filling the cuff or using the strap, it was more convenient to use. It therefore seems likely that, as with the LMA, the SLIPA can take the place of endotracheal intubation for inexperienced users or in times of an emergency.
An advantage of SGA is that it removes the need for a laryngoscope during insertion, thus avoiding direct irritation of the trachea. During endotracheal intubation, a temporary elevation of blood pressure, tachycardia and arrhythmia may occur. Such cardiovascular changes are caused by irritation to the upper airway by the laryngoscope blade, and to the trachea by the intubation of the endotracheal tube and the expansion of the endotracheal tube cuff [
12]. Airway management by PLMA is reported to decrease hemodynamic responses compared with endotracheal intubation [
13]. Puri et al. [
3] reported that in SLIPA use, blood pressure and heart rate increase more than in PLMA uses, but this difference was not as significant as the difference in the use of endotracheal intubation. In this study, the PLMA group showed steady hemodynamic responses before and after insertion, whereas in the SLIPA group, 1 minute after insertion, the blood pressure and heart rate significantly increased to the maximum value. The longer the insertion time, the greater the risk of tachycardia and hypertension [
14]. Good SLIPA insertion technique and correct size selection can thus reduce insertion time and produce a more stable hemodynamic response. The maximal change of mean value (%) in blood pressure and heart rate during endotracheal intubation in the report by Kim et al. [
13] was 55.7% for SBP, 47.5% for DBP, and 48.2% for HR. According to Lee et al. [
15], these values were 51%, 58%, and 48% respectively. In the present study the respective values for the SLIPA group were 12.8%, 16.4%, and 7.6%. Although not directly measured in this study, SLIPA insertion in comparison to endotracheal intubation is assumed to bring fewer hemodynamic changes.
When positive pressure ventilation using LMA, gas leakage and gastric distension are caused by high airway pressure or the inappropriate location of the laryngeal mask. The LMA maintains the airway though a firm seal between its cuff and the structures surrounding the glottis. In contrast to endotracheal intubation, a PIP higher than the OLP can thus result in gas leakage around the cuff. This can trigger inadequate ventilation or gastric distension, heightening the risk of regurgitation and pulmonary aspiration and increasing the incidence of postoperative nausea [
16]. During LMA use, gas leakage and gastric distension have been reported when positive pressure ventilation was used with inspiratory gas pressures of over 20 cm H
2O [
16]. Devitt et al. [
17] reported gastric distension in 35% of patients at 30 cmH
2O airway pressure. The PLMA was designed so that the larger, wedge-shaped cuff would plug gaps in the proximal pharynx, and it forms a more effective seal with the upper airway than the conventional LMA [
18]. In a comparative study of OLP in PLMA and LMA usage [
19], the PLMA had a 10 cmH
2O higher OLP than the LMA. In the present study there was no significant difference in OLP between the PLMA and the SLIPA, and both groups had a higher OLP than the mean value of PIP during surgery. Furthermore, gas leakage and gastric distension were not observed during surgery, so in our judgment the risk of pulmonary aspiration caused by both devices was not high. Also, there was no significant difference in gas leakage associated with head position in the two groups. Both groups had relatively safe airway maintenance.
In addition, if the SGA in placed incorrectly it cannot seal effectively with the periglottic tissue and gas leakage may result. The leaked gas will then flow into the esophagus and cause gastric distension and pulmonary aspiration. As assessed by fiberoptic bronchoscope, a hypopharynx placement score of 3 or 4 points is considered to indicate appropriate insertion location. Gaitini et al. [
20] reported 60% of the LMAs as being in the appropriate location. When PLMAs and LMAs were compared, 48% of PLMAs and 74% of LMAs were reportedly successful. This means LMAs were easier to insert [
21]. In the present study, 60% of PLMAs and 40% of SLIPAs were deemed to be appropriately inserted at fiberoptic assessment. However, there are reported cases that the fiberoptic position was thought be accurate and effective ventilation was assumed to be achieved, but the actual location was improper [
22]. Therefore, fiberoptic findings cannot completely exclude the possibility of gastric distension. However, in the present study gastric distension was not observed before or after surgery. Lung mechanics data were the same for both SLIPA and PLMA, and they both gave adequate ventilation.
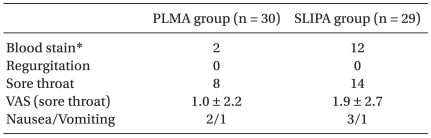
After removal of the airway devices, SLIPAs had significantly higher incidence of blood stains than PLMAs. The PLMA is made of a soft material with its position secured by insertion of air into the cuff, whereas the SLIPA is made of stiffer plastic material than the PLMA and is of a fixed shape. The SLIPA thus causes more direct trauma to the oral mucosa. In a comparison of postoperative complications in the recovery room, PLMAs have been reported to have fewer cases of sore throat compared to endotracheal tubes and a lower severity of pain [
23]. The incidences of sore throat according to Miller et al. [
8] were 57%, 49%, and 30% respectively for endotracheal tubes, SLIPA, and PLMA. The present study yielded similar results, with the SLIPA group having a relatively high incidence of sore throat (thoughwithoutstatistical significance), the VAS scores in more than half of the cases being below 3, and the severity of sore throat being mild. Compared to PLMAs, SLIPAs had more cases of sore throat, attributable to the stiff material the SLIPA is made of. The material can irritate and damage the pharyngeal mucosa, and it also causes a higher number of insertion attempts. Nausea, vomiting, and the other complications were uncommon in both groups.
When a cuff is used to seal the pharynx, as is the case with PLMAs, the initial cuff pressure of 60 cm H
2O gradually increases because of N
2O diffusion across the cuff wall. The intra cuff pressure significantly increases over 30 minutes [
24], increasing the risk of ischemic damage of the laryngopharyngeal mucosa. It is thus important to constantly monitor the intracuff pressure [
25]. Additionally, the LMA cuff can also cause pressure neuropraxia of the lingual nerve, hypoglossal nerve, and recurrent laryngeal nerve, while N
2O use can cause an increase incompressive and/or stretching forces on oralorpharynx [
26]. In the present study, usage of the PLMA was also associated with elevation of cuff pressure during surgery, with adjustment of the cuff pressure to 60 cmH
2O with a hand pressure gauge necessary on several occasions. Furthermore, in 2 cases the change in cuff pressure caused PLMA slippage and hence gas leakage, with the PLMA thus requiring repositioning. The advantage of SLIPAs is that they do not have cuffs, and thus are unaffected by the use of N
2O.
The PLMA is designed for multiple sterilizations and reuse. The manufacturer explains that autoclaving can be performed up to 40 times. However, washing and autoclaving cannot completely remove protein deposits. Many different methods for cleaning and sterilizing have thus been discussed, but complete removal of protein is known to be impossible [
27]. Protein contamination of reused medical devices can cause the transmission of prion proteins, with PLMA reuse running the risk of aiding in the transmission of variant Creutzfelt-Jacob disease. Also, when many PLMAs are washed together, protein cross-contamination can occur [
28]. For such reasons, using disposable devices which have no difference in effectiveness lowers the risk of contamination and is more hygienic. As SLIPA is cheaper than PLMA, disposal after single use is advised. A further economical advantage is the lower cost of cleaning and sterilization.
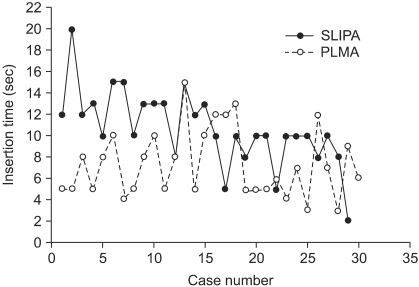
As a limitation of the present study, while we have much experience and skill at PLMA insertion, we have comparatively little experience with using SLIPA. Puri et al. [
3] stated that SLIPA had a short learning curve, with a plateau at 13 cases. In the present study, all the SLIPA insertions were performed by one anesthesiologist who had experience of more than 20 SLIPA insertions before this study. The time taken for SLIPA insertion and the number of attempts required both decreased as the study progressed (
Fig. 3). In contrast, the PLMA insertion time and required attempts did not change (
Fig. 3). We assume this difference to be due to accumulated experience and accept that it may have affected the results of the study. Another limitation was that evaluation in the recovery room was performed by a blinded anesthesiologist while all other evaluations were performed by the anesthesiologist who performed the insertions. This may have affected the results.
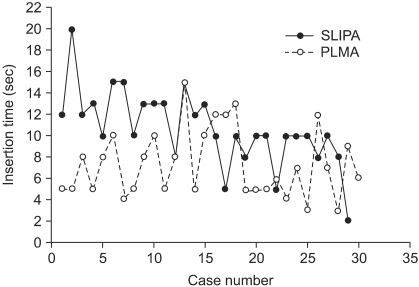 | Fig. 3Time taken for insertion (seconds) according to case numbers. SLIPA: streamlined liner of the pharynx airway, PLMA: laryngeal mask airway ProSeal™. 
|
In conclusion, as a newly developed SGA, SLIPA, compared to PLMA, showed statistically significant differences in ease of insertion and low hemodynamic response to insertion. However, the differences are of an acceptable level and there were no differences in airway maintenance and ventilatory efficiency. SLIPA usage was unaffected by N2O the lower cost of the SLIPA means it is suitable for single-use. We expect SLIPA usage to replace PLMA usage and the SLIPA will be used widely.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download