Abstract
Background
Arthroscopic shoulder surgery has been performed in the sitting position under interscalene block (ISB). Bradycardia hypotension (BH) episodes have a reported incidence of 13-29% in this setting. We performed a retrospective study to investigate contributing factors to the occurrence of BH episodes.
Methods
According to BH episodes, we divided 63 patients into two groups: BH group (n = 13) and non-BH group (n = 50). Anesthetic records and block data sheets were reviewed for demographic data, intraoperative medications, sites of ISB, use of epinephrine in local anesthetics, degree of sensory blockade, and percent change of heart rate or systolic blood pressure (SBP). Statistical analysis was done using Chi square test and Student's t-test.
Results
There were no significant differences in the use of epinephrine in local anesthetics between the two groups. The location of ISB site was different between the two groups in that there were relatively more right-sided ISBs in the BH group than in the non-BH group (P = 0.048). The degree of sensory blockade was lower, but not significantly, in the C8 and T1 dermatomes of the BH group than in the non-BH group (P = 0.060 and 0.077, respectively). There was a relatively higher incidence of fentanyl supplementation in the BH group than in the non-BH group (P = 0.000).
Arthroscopic shoulder surgery has been performed in the sitting or beach chair position [1,2] under interscalene brachial plexus block (ISB) [3,4] in a lot of organizations. Advantages of this position include a lower incidence of traction neuropathy [5], less intraoperative blood loss [3], and easier conversion to an open procedure [1]. ISB can be selected as the primary anesthetic technique for shoulder surgery with excellent intraoperative anesthesia, muscle relaxation [6], and low complication rate [7], as well as the opportunity for postoperative analgesia [8]. ISB has been shown to be successful when performed by dedicated anesthesiologists, but resistance to its use still exists because of cardiovascular instability such as bradycardia and/or hypotension (BH) episodes, which have been seen in 13-29% of patients who had ISB for shoulder arthroscopy in the sitting position [9-12]. Some authors believe that BH is a form of vasovagal syncope mediated by the Bezold-Jarisch reflex (BJR), which occurs when venous pooling and increased sympathetic tone induce a low-volume, hypercontractile ventricle [10-12]. This results in sudden activation of the parasympathetic nervous system and sympathetic withdrawal, causing bradycardia and hypotension. However, there is no definite evidence that cardioinhibitory receptors or the BJR per se have a primary role in this type of syncope [13]. A retrospective review found that perioperative use of epinephrine for ISB was associated with a much higher incidence of BH episodes [12]. However, at our institution, the perioperative use of epinephrine for ISB seems not to be a contributing factor to BH episodes. There is also controversy about the perioperative use of β-blockers to prevent BH episodes [9,11]. Therefore, the aim of this retrospective study is to reevaluate the known contributing factors to BH and to find new possible contributing factors to those episodes after ISB while in the sitting position during arthroscopic shoulder surgery.
This retrospective study was conducted by reviewing anesthetic records and block data sheets from the 63 patients who were American Society of Anesthesiologists physical status (ASA PS) I and ASA PS II and received ISB with 20 ml of 0.75% ropivacaine and 10 ml of 1% lidocaine or mepivacaine for arthroscopic shoulder surgery in the sitting position. Surgical procedures included shoulder arthroplasty, rotator cuff repair, and acromioplasty. The anesthesia records were reviewed for BH episodes, which we defined as bradycardia and/or hypotension. Bradycardia was defined as a decline in heart rate to less than 50 bpm and a requirement of atropine. Hypotension was similarly defined as a decline in systolic blood pressure (SBP) to less than 100 mm Hg and a requirement of ephedrine. According to BH episodes, we divided 63 patients into two groups; bradycardia-hypotension (BH) group (n = 13) and non-bradycardia-hypotension (non-BH) group (n = 50). All patients received intramuscular premedication with 0.05 mg/kg of midazolam 30 minutes before going to the operating room. After placement of electrocardiogram (ECG) electrodes, blood pressure cuff and pulse oximeter to monitor each patient, ISB using Winnie's technique was performed in the preoperative area or operating room by an attending anesthesiologist. Each patient was in the supine position with the head turned to the opposite side to be blocked. The interscalene groove was identified at the level of the cricoid cartilage, and the patient was prepped in an aseptic manner with iodine topical solution. Using a 25-gauge needle, 0.5 to 1 ml of 1% lidocaine was injected subcutaneously for a skin wheal. A sterile 24-gauge 50-mm insulated block needle (Braun Contiplex Block set; Braun, Melsungen, Germany) was used with the multiplex nerve stimulator (B. Braun, Melsungen, Germany). The initial current output of the nerve stimulator was set at 1.0 mA. The insulated needle was advanced through the interscalene groove until a contraction of the biceps or deltoid muscle (or both), whichever appeared first, was elicited. Needle position was then adjusted until a twitch of either biceps or deltoid muscle group could still be elicited with the current output <0.5 mA, after which 20 ml of 0.75% ropivacaine and 10 ml of 1% lidocaine or mepivacaine was injected. After administering the local anesthetics, the degree of sensory blockade was evaluated by pinprick test 20 minutes after injection.
Anesthesia record and block data sheets were reviewed for sex, age, height, weight, ASA PS, NPO time, operation site, volume of local anesthetics, use of epinephrine in local anesthetics, minimal current, visible motor response at nerve stimulation and degree of sensory blockade. Sensory blockade was measured by pinprick test and graded as no block, 0; moderate block, 1; complete block, 2. We also evaluated the time from the end of block to operation start, duration of anesthesia, duration of surgery, amount of fluids, and use of intraoperative medications. The cardiovascular variables of each five-minute interval were changed to values of the percent change of that interval from the initial values found at sitting position. Rmax of heart rate or Rmax of SBP is defined as the maximal decrease (Rmax) of heart rate or SBP as compared to the initial values at sitting position. We also obtained Rmax time of heart rate or SBP which is defined as the time to reach Rmax of heart rate or SBP. Statistical analysis consisted of Student's t-tests for comparison of age, height, weight, NPO time, minimal current of nerve stimulation, degree of sensory blockade, all the time intervals, amount of fluid and Rmax or Rmax time of heart rate or SBP. Chi square analyses were performed to compare ASA physical status, gender, type and site of surgery, use of epinephrine in local anesthetics, visible motor response at nerve stimulation and intraoperative medications. A P value of less than 0.05 was considered significant. All data were reported as mean ± SEM.
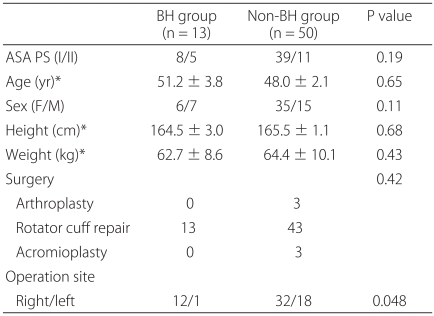
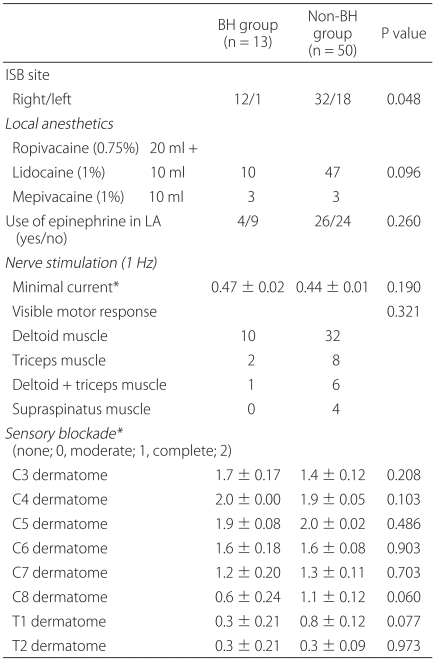
The overall percent of BH episodes in this retrospective study was 20.6%. The BH Group (n = 13) consisted of 4 patients with bradycardia, 6 with hypotension, and 3 patients with both simultaneously. Demographic data are presented in Table 1. There were no significant differences between the two groups in patients' sex, height, weight, ASA PS, or distribution of surgical cases. The ratio of right versus left operation site differed between the two groups in that the BH group had relatively more right side operations than the non-BH group (P = 0.048). Data of block sheets are shown in Table 2. The dose (20 + 10 ml) and choice of local anesthetic varied and included 20 ml of ropivacaine and 10 ml of lidocaine or mepivacaine. There was no significant difference in the ratio of the use versus non-use of epinephrine in local anesthetics between the two groups. Data from the nerve stimulation did not differ between the two groups regarding minimal electrical current at nerve stimulation and the site, such as deltoid or biceps muscles, of visible motor response. The degree of sensory blockade on C8 and T1 dermatomes for the BH group was slightly decreased, but not significantly (P = 0.060, P = 0.077 respectively), as compared with the non-BH group.
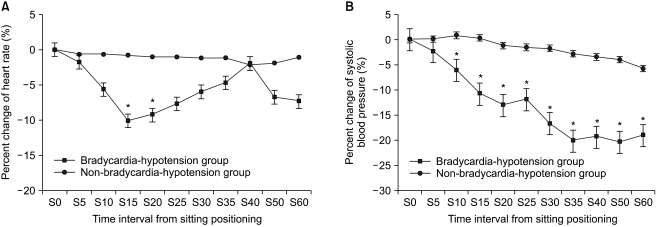
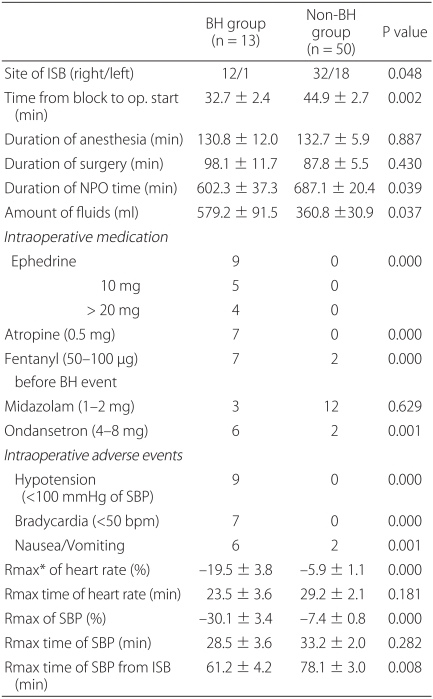
Anesthetic characteristics and anesthetic-related complications are shown in Table 3. The ISB site was different between the two groups in that there were relatively more right side ISBs in the BH group than in the non-BH group (P = 0.048). Readiness of surgery, which is defined as the time from the end of the interscalene block to the start of the operation, was sooner in the BH group as compared with the non-BH group (32.7 ± 2.4 min, 44.9 ± 2.7 min, respectively, P = 0.002). However, there were no differences in the duration of anesthesia and surgery. The duration of NPO time of the non-BH group was longer than that of the BH group, and the amount of intraoperative fluid was relatively more in the BH group than in the non-BH group. In the BH group, nine patients received over 10 mg of ephedrine to treat hypotension and seven patients received 0.5 mg of atropine to treat bradycardia. There was a relatively higher incidence of fentanyl supplementation in the BH group than in the non-BH group (P = 0.000), whereas there was no significant difference in whether or not they were given midazolam. The use of ondansetron for intraoperative nausea and vomiting was higher in the BH group than in the non-BH group (P = 0.001). Baseline heart rate and SBP did not significantly differ between two groups (P > 0.05) (BH group, 76 ± 12 bpm, 120 ± 10 mmHg; non BH group, 79 ± 15 bpm, 120 ± 10 mmHg, data not shown). Moreover, the initial heart rate and SBP in the sitting position was not significantly different between the two groups. However, mean Rmax of heart rate, or the maximal decrease in heart rate from the sitting position, for the BH group was significantly decreased compared to the non-BH group (-19.5 ± 3.8% versus -5.9 ± 1.1, respectively, P = 0.000) whereas mean Rmax time of heart rate, or the time it took to reach Rmax, did not differ significantly between the two groups. Similarly, mean Rmax of SBP for the BH group was significantly decreased compared with the non-BH group (-30.1 ± 3.4% versus -7.4 ± 0.8, respectively, P = 0.000) whereas mean Rmax time of SBP did not differ between the two groups (28.5 ± 3.6 min versus 33.2 ± 2.0 min respectively, P = 0.282). The percent change of heart rate 15 and 20 minutes after being in the sitting position was significantly decreased in the BH group, whereas it was at the time interval of 5 minutes where the percent change of SBP after the sitting position was significantly decreased compared to the non-BH group (Fig. 1).
The main purpose of this retrospective study was to reevaluate or find possible contributing factors to BH episodes that occur in the sitting position during arthroscopic shoulder surgery after ISB. The results of our study demonstrated a 20% incidence of BH episodes, which is consistent with previous reports [9-12]. The average Rmax time of SBP from the end of the interscalene block in the BH group was 61 minutes, which is also comparable to previous studies [10,12]. In contrast to the other studies, however, our results indicate that the site of ISB and fentanyl supplementation due to incomplete block or emotional stress may be new contributing factors to the occurrence of BH episodes.
One proposed mechanism for the occurrence of BH episodes is based on the activation of the Bezold-Jarisch reflex (BJR) [10,14]. The BJR is an inhibitory reflex usually denoted as a cardioinhibitory reflex. Animal experiments have shown that the BJR has its origin in cardiac receptors with nonmyelinated, type C vagal fibers constituting the afferent limb of the reflex [15]. Activation of BJR initiates from an empty hypercontractile ventricle, which causes stimulation of intramyocardial mechanoreceptors (C fibers) and produces an abrupt withdrawal of sympathetic outflow, increasing vagal tone and thus causing bradycardia and hypotension. D'Alessio et al. reported [10] that the mechanism of the BJR during shoulder arthroscopic surgery was thought to be due to venous blood pooling (induced by the sitting position) and a heightened cardiac contractile state (induced by the β-adrenergic effects of epinephrine or isoproterenol), which result in reflex arterial vasodilation (mediated by activation of the parasympathetic nervous system) and a subsequent vagally mediated bradycardia. However, there is no convincing data in the literature to support these prerequisites. Although this empty ventricle concept was found during epidural anesthesia [16] and in the tilt-table testing to evaluate the underlying cause of syncope [17], echocardiography data failed to demonstrate either an empty ventricle or more vigorous ventricular contraction during syncopal episodes [18,19]. Campagn and Carter [13] recently pointed out that the BJR is not synonymous with vasovagal syncope, which is a loss of consciousness caused by reduced blood pressure and blood supply to the brain, mediated through neural mechanisms rather than primary cardiac dysfunction. The trigger factors for vasovagal syncope may be central, from psychic stress or pain, or may be initiated peripherally by a reduction in venous return to the heart. Unfortunately, there is no evidence that cardioinhibitory receptors or the BJR per se have a primary role in this type of syncope. Campagn and Carter [13] mentioned that BH episodes seen in shoulder surgery during ISB appear not to be related to BJR activation.
Liguori et al. [11] demonstrated that a β-blocker markedly decreases the incidence of BH episodes when given prophylactically immediately after the administration of the interscalene block. However, Kahn and Hargett [9] reported that there was a 13% incidence of BH episodes that were not affected by the use of β-blockers. Unfortunately, our results did not provide any clue to the prophylactic effects of β-blockers on BH episodes because there was no patient who had received a β-blocker. A randomized, prospective study is necessary to clarify this issue.
In the current study, we found that there was no significant difference between the BH and non-BH groups regarding the use of epinephrine (150 µg) in local anesthetics for ISB. These findings suggest that the use of epinephrine as a local anesthetic cannot be a contributing factor to the occurrence of BH episodes. However, Sia et al. [12] previously reported on a group of patients (Group E) who received exogenous epinephrine (200 ± 13 µg) and in whom the incidence of BH episodes was significantly higher than in a group of patients (Group P) who did not (29% versus 11%; P = 0.018). The authors suggested that even a small epinephrine dose, such as that administered with the local anesthetic mixture for ISB, can result in a blood level high enough in some patients to incite the BJR when associated with the placement of the patient in the sitting position. However, there is no evidence for increased contractility due to the epinephrine used in local anesthetic mixtures for nerve block [20]. We think that these differences regarding the exogenous epinephrine may occur from differences in study design or exclusion criteria. A significant percent of patients (31%) in a group of patients (Group E) received an antihypertensive drug in the study of Sia et al. [12], whereas there was no patient who received an antihypertensive in the present study.
In the current study, a significant percentage of patients in the BH group (92.3%) received a right side ISB. These findings suggest that the site of ISB can be a contributing factor to the occurrence of BH episodes. We think that right stellate ganglion block (SGB) induced by ISB can be involved in BH episodes. Vester-Andersen [21] reported an incidence of 75% of SGB, or Horner syndrome, as side effects of Winnie's technique. In addition, all major sympathetic cardiopulmonary nerves were found to arise from the stellate ganglia, and the caudal halves of the cervical sympathetic trunks lie below the level of the cricoid cartilage [22]. Therefore, it is an acceptable hypothesis that right SGB induced by ISB can prevent the compensatory response of hemodynamic changes caused by the sitting position and can contribute to the occurrence of BH episodes during shoulder surgery. Previous other results strongly support this hypothesis; D'Alessio et al. [10] did not find a predominance of right side blocks in the BH group. Masuda and Fujiki [23] reported a case of sinus arrest that occurred after head-up tilt in right SGB, probably because of a vasovagal reflex. Rogers et al. [24] demonstrated a significantly slowed heart rate after right SGB but not so after left-sided block. We also reported a case of a 32 year-old male patient who had Horner syndrome and asystolic cardiac arrest 15 minutes after being in the sitting position during shoulder arthroscopic surgery under right ISB [25]. Fujii et al. [26] reported that right SGB induces significant increases of QT interval and rate-corrected QT (QTc) interval for 50 minutes after the block, but left SGB induces a significant decrease of QT interval and QTc interval. Nakagawa et al. [27] reported that a 70° head-up tilt produced significant increases of QT interval and rate-corrected QT dispersion (QTcD), because head-up tilt increased sympathetic tone and/or decreased vagal tone. These findings suggest that right SGB and head-up tilt are associated with increased risks of ventricular arrhythmias and cardiovascular diseases. Unfortunately, Horner syndrome induced by SGB was not described in anesthesia records and block data sheets, which was a limitation of this retrospective study. As such, a prospective and randomized study is needed to confirm that right side ISB is associated with the occurrence of BH episodes.
In the current study, there were no differences of the degree of sensory blockade between the two groups. However, the P values of C8 and T1 dermatomes (0.060 and 0.077, respectively) are very close to the statistically significant value 0.05. Therefore, it is a possible explanation that, in receiving more fentanyl supplementation, the BH group demonstrated incomplete blockade. We also think that fentanyl supplementation due to incomplete block, which may cause emotional stress, can be a possible contributing factor to the occurrence of BH episodes. The limbic system is concerned with emotions, and in some animal species stimulation of the limbic sympatho-inhibitory center causes hypotension and bradycardia [28]. In addition, there is some evidence that endogenous opioid, which is an important neurotransmitter in the nucleus tractus solitaries, is involved in syncopal reactions in animals [29]. Griffioen et al. [30] demonstrated that fentanyl inhibits GABAergic transmission to cardiac vagal neurons in the nucleus ambiguus, providing one mechanism for opioid-induced bradycardia.
There are several limitations to the current study, which is basically derived from the characteristics of a retrospective study. Each block sheet after ISB in the current study did not include a clear description of the side effects of ISB. We could not check the incidence of SGB as a complication of ISB in the current study. Readiness of surgery in the current study was achieved sooner in the BH group than in the non-BH group. Although these findings might be related to inadequate hemodynamic compensation in the sitting position after ISB or emotional stress before starting the operation, our results cannot provide a definitive evidence for these assumptions. In addition, NPO time, which ranges from midnight to the start of the surgical anesthesia, was longer in the non-BH group than in the BH group. This suggests that the duration of NPO time cannot be a contributing factor to BH episodes in our setting.
In summary, although BH episodes are unpredictable events, our results demonstrate that the site of ISB and fentanyl supplementation due to incomplete block can be possible new contributing factors to the occurrence of BH episodes in shoulder arthroscopic surgery. BH episodes are usually of minor significance, but in the extreme they may lead to cardiac arrest. Therefore, we suggest that careful observation of patients who have received shoulder arthroscopic surgery in the sitting position is needed when given fentanyl supplementation due to incomplete block after right side ISB.
References
1. Skyhar MJ, Altcheck DW, Warren RF, Wickiewicz TL, O'Brien SJ. Shoulder arthroscopy with the patient in the beach-chair position. Arthroscopy. 1988; 4:256–259. PMID: 3233114.

2. D'Alessio JG, Rosenblum M, Shea KP, Freitas DG. A retrospective comparison of interscalene block and general anesthesia for ambulatory surgery shoulder arthroscopy. Reg Anesth. 1995; 20:62–68. PMID: 7727331.
3. Tetzlaff JE, Yoon HJ, Brems J. Interscalene brachial plexus block for shoulder surgery. Reg Anesth. 1994; 19:339–343. PMID: 7848934.
4. Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone JN, et al. Interscalene regional anesthesia for arthroscopic shoulder surgery: a safe and effective technique. J Shoulder Elbow Surg. 2006; 15:567–570. PMID: 16979050.

5. Ellman H. Arthroscopic subacromial decompression: analysis of one to three year results. Arthroscopy. 1987; 3:173–181. PMID: 3675789.
6. Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU. Interscalene block for shoulder arthroscopy: comparison with general anesthesia. Arthroscopy. 1993; 9:295–300. PMID: 8323615.

7. Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone J, et al. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am. 2005; 87:974–979. PMID: 15866958.

8. Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: a comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg. 2004; 99:589–592. PMID: 15271745.

9. Kahn RL, Hargett MJ. β-adrenergic blockers and vasovagal episodes during shoulder surgery in the sitting position under interscalene block. Anesth Analg. 1999; 88:378–381. PMID: 9972760.
10. D'Alessio JG, Weller RS, Rosenblum M. Activation of the Bezold-Jarisch reflex in the sitting position for shoulder arthroscopy using interscalene block. Anesth Analg. 1995; 80:1158–1162. PMID: 7762845.
11. Liguori GA, Kahn RL, Gordon J, Gordon MA, Urban MK. The Use of metoprolol and glycopyrrolate to prevent hypotensive/bradycardic events during shoulder arthroscopy in the sitting position under interscalene block. Anesth Analg. 1998; 87:1320–1325. PMID: 9842820.

12. Sia S, Sarro F, Lepri A, Bartoli M. The effect of exogenous epinephrine on the incidence of hypotensive/bradycardic events during shoulder surgery in the sitting position during interscalene block. Anesth Analg. 2003; 97:583–588. PMID: 12873958.

13. Campagna JA, Carter C. Clinical relevance of the Bezold-Jarisch reflex. Anesthesiology. 2003; 98:1250–1260. PMID: 12717149.
14. Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: relationship to vasovagal syncope and the Bezold-Jarisch reflex. Br J Anaesth. 2001; 86:859–868. PMID: 11573596.

15. Donald DE, Shepard JT. Reflexes from the heart and lungs: physiological curiosities or important regulatory mechanisms. Cardiovasc Res. 1978; 12:446–469. PMID: 363264.

16. Baron JF, Decaux-Jacolot A, Edouard A, Berdeaux A, Samii K. Influence of venous return on baroreflex control of heart rate during lumbar epidural anesthesia in humans. Anesthesiology. 1986; 64:188–193. PMID: 3080922.

17. Nwosu EA, Rahko PS, Hanson P, Grogan EW Jr. Hemodynamic and volumetric response of the normal left ventricle to upright tilt testing. Am Heart J. 1994; 128:106–113. PMID: 7912470.

18. Liu JE, Hahn RT, Stein KM, Markowitz SM, Okin PM, Devereux RB, et al. Left ventricular geometry and function preceding neurally mediated syncope. Circulation. 2000; 101:777–783. PMID: 10683352.

19. Novak V, Honos G, Schondorf R. Is the heart "empty' at syncope? J Auton Nerv Syst. 1996; 60:83–92. PMID: 8884700.

20. Bonica JJ, Akamatsu TJ, Berges PU, Morikawa K, Kennedy WF Jr. Circulatory effects of peridural block. II. Effects of epinephrine. Anesthesiology. 1971; 34:514–522. PMID: 5556242.
21. Vester-Andersen T, Christiansen C, Hansen A, Sørensen M, Meister C. Interscalene brachial plexus block: area of analgesia, complications and blood concentrations of local anesthetics. Acta Anaesthesiol Scand. 1981; 25:81–84. PMID: 7324828.
22. Janes RD, Brandys JC, Hopkins DA, Johnstone DE, Murphy DA, Armour JA. Anatomy of human extrinsic cardiac nerves and ganglia. Am J Cardiol. 1986; 57:299–309. PMID: 3946219.

23. Masuda A, Fujiki A. Sinus arrest after right stellate ganglion block. Anesth Analg. 1994; 79:607. PMID: 8067580.

24. Rogers MC, Battit G, McPeek B, Todd D. Lateralization of sympathetic control of the human sinus node: ECG changes of stellate ganglion block. Anesthesiology. 1978; 48:139–141. PMID: 655444.
25. Park CH, Kwon HT, Roh WS. A case of asystolic cardiac arrest in the sitting position for shoulder arthroscopy using an interscalene block. Korean J Anesthesiol. 2006; 51:383–386.
26. Fujii K, Yamaguchi S, Egawa S, Hamaguchi S, Kitajima T, Minami J. Effects of head-up tilt after stellate ganglion block on QT Interval and QT Dispersion. Reg Anesth Pain Med. 2004; 29:317–322. PMID: 15305250.

27. Nakagawa M, Takahashi N, Iwao T, Yonemochi H, Ooie T, Hara M, et al. Evaluation of autonomic influences on QT dispersion using the head-up tilt test in healthy subjects. Pacing Clin Electrophysiol. 1999; 22:1158–1163. PMID: 10461291.

28. Van Lieshout JJ, Wieling W, Karemaker JM, Eckberg DL. The vasovagal response. Clin Sci (Lond). 1991; 81:575–586. PMID: 1661644.

29. Wallbridge DR, Maclntyre HE, Gray CE, Oldroyd KG, Rae AP, Cobbe SM. Role of endogenous opioids and catecholamines in vasovagal syncope. Eur Heart J. 1996; 17:1729–1736. PMID: 8922923.

30. Griffioen KJ, Venkatesan P, Huang ZG, Wang X, Bouairi E, Evans C, et al. Fentanyl inhibits GABAergic neurotransmission to cardiac vagal neurons in the nucleus ambiguous. Brain Res. 2004; 1007:109–115. PMID: 15064141.
Fig. 1
Percent change of heart rate (A) and systolic blood pressure (B) according to time interval from sitting position. Values are expressed as means ± SD. Sn: n minutes after sitting position. *P < 0.05 compared with non-bradycardia-hypotension group.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download