Introduction
It is common for patients to feel anxious before surgery. The frequency varies depending on the measuring method of anxiety. Recently, Boker et al. [
1] reported that 60% of patients who present for elective surgery are known to experience anxiety. Preoperative anxiety not only requires larger amounts of anesthetics [
2,
3] but also increases the patient's catecholamine secretion, and catecholamine causes tachycardia, hypertension, and arrhythmia [
4,
5]. Moreover, preoperative anxiety affects the level of recovery and postoperative pain [
6]. The prevalence of preoperative anxiety depends on the patient group. According to studies, a high prevalence is found in females, relatively young patients, patients who ask many questions about the surgery, and patients without prior surgery experience. Gender and age especially have a correlation with preoperative anxiety [
3,
7-
9]. Most anesthesiologists have negative experiences with preoperative anxiety affecting patients; therefore, to reduce preoperative anxiety, anesthesiologists make preoperative visits, administer preoperative sedatives, and use many other methods. Even though the negative effects of preoperative anxiety are widely known, no studies even to the present day have been conducted on the correlation of the level of preoperative anxiety and hemodynamic changes during anesthetic induction.
There are many reported ways to measure a patient's anxiety level. Spielberger's state-trait anxiety inventory (STAI) is one of the most commonly used anxiety tests among the subjective self-measuring tests. At first, it was developed as a tool for measuring the anxiety level in mean healthy people, but then the test was found to be useful in measuring anxiety in patient groups. Therefore, the STAI is now the standard tool for measuring preoperative anxiety [
7]. The STAI measures anxiety with the state subscale and the trait subscale. The state subscale measures temporary anxiety. The value has variations for individuals for subjective feelings of tension, concern, and worries depending on the situation. The trait subscale is relatively stable in showing personal differences in how individuals differently experience anxiety [
10].
The authors used the STAI to evaluate the correlation between patients' preoperative anxiety and their hemodynamics during anesthetic induction. As age and gender are known to affect anxiety, we also aimed at finding out how age and gender play a role in the correlation. In addition, we aimed at discovering whether the STAI can be used as an indicator to predict hemodynamic changes after anesthetic induction.
Go to :

Materials and Methods
This research received the approval of the clinical research ethics committee and then received the consent of the patient subject groups. The patient subjects included 120 patients from age 18 to 65 who fell under ASA Class I & II and were due for elective surgery under general anesthesia. Patients were excluded from the study if they had a history of psychiatric illness, a frequent intake of sleeping pills or sedatives, a disease of the central nervous system, pregnancy, hypertension, chronic obstructive pulmonary disease, asthma, or other cardiopulmonary diseases, or if they were Mallampati classification III or above and predicted to have difficult tracheal intubation.
The day before the surgery, the anesthesiologist visited patients around 9 p.m. to 10 p.m. to explain the purpose of the research study and get their consent. The patients were made to fill out the STAI themselves. No patients were administered preoperative drugs. On the day of the surgery, an ECG, a noninvasive automatic hemodynamometer, and a peripheral oximeter (IntelliVue MP40, Philips, Eindhoven, Netherlands) were attached to the patient. Blood pressure and heart rate were measured 3 times, and the means were used as the base blood pressure and the base heart rate. With 100% oxygen 5 L/min, the patient was made to breathe deeply 5 times. After preoxygenation, anesthesia was induced. Thiopental sodium 5 mg/kg was intravenously infused. When the loss of the patient's eyelid reflex was checked, rocuronium 0.6 mg/kg was injected intravenously. Manual ventilation was performed for 2 minutes. Then tracheal intubation was performed. When manual ventilation was initiated, the noninvasive hemodynamometer was put in stat mode and was continuously checked. The highest blood pressure and heart rate within 5 minutes after tracheal intubation were recorded and defined to be the patient's highest blood pressure and highest heart rate. They were then compared to the base blood pressure and base heart rate. The amount of change was recorded in percentages. After measurements were taken for 5 minutes, sevoflurane 2 vol% and remifentanil 0.25-0.5 µg/min/kg were used for anesthetic maintenance. Tracheal intubation was performed by an anesthesiologist with 2 years of experience. If tracheal intubation was not successful on the first attempt, the patient was excluded from the research study.
For statistical analysis, MedCalc® 10.0 (Mariakerke, Belgium) was used. The results are shown in the mean ± standard deviation. The patient's level of anxiety and the correlation to the changes in blood pressure and pulse rate was checked with linear regression analysis. The primary objective of the research study was the correlation analysis. In a preliminary experiment, the correlation factor was found to be 0.285. Assuming α = 0.05 and β = 0.2, the minimum sample size was 94 patient subjects. The receiver operation characteristic (ROC) curve was used to evaluate if the patient's anxiety scores found with the STAI could help in predicting 20% or more hemodynamic changes during anesthetic induction. P < 0.05 was considered statistically meaningful. In a preliminary experiment, the AUC was found to be 0.5. If 0.7 or more AUC had predictability of 20% or more hemodynamic changes, the minimum sample size was 78 patients. We included 120 patients in our study to compensate for the expected exclusion of certain patients.
Go to :

Results
Out of 120 patients, 9 patients were excluded because they needed 2 attempts at tracheal intubation or because they declined to participate in the study.
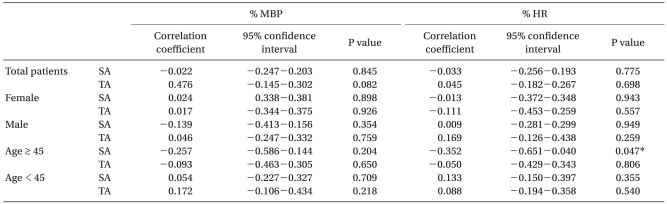
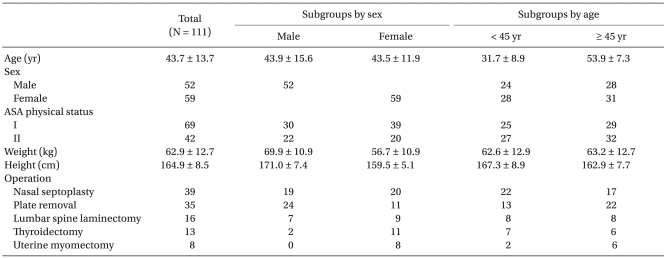
Table 1 shows the patients' age, gender ASA class, weight, height, and the name of their surgery for this study. Data on preoperative anxiety scores, length of surgery in hours, changes in percentages of pre/post tracheal intubation blood pressure, and pulse rate was analyzed by gender and by age. In the age subgroups, patients age 45 or older were grouped together, and patients below age 45 were grouped separately. There were significant differences between the age groups in state anxiety scores, blood pressure changes, and heart rate changes. However, no such differences were found between the genders (
Table 2).
Table 1
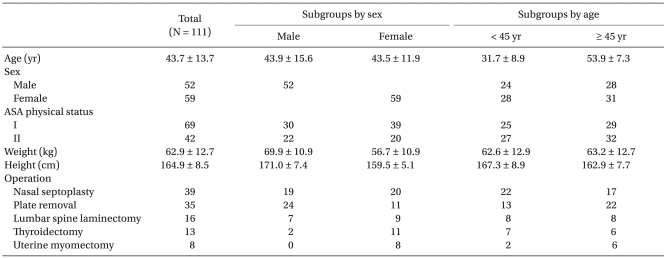

Table 2
Spielberger's State-trait Anxiety Inventory and Hemodynamic Changes
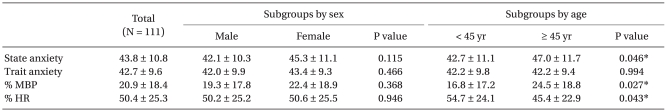

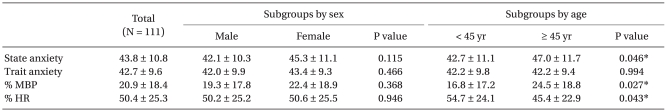
When the data by total patient group was analyzed, the changes from the base blood pressure and base pulse rate measured in the calm state to the highest blood pressure and the highest pulse rate in 5 minutes were not correlated to the patients' state anxiety scores and trait anxiety scores. When the data was sorted into the age subgroups 45 years of age or older or below 45, the state anxiety scores of those who were 45 years of age or older and their changes in pulse rate showed a significant correlation (P = 0.047 by Pearson correlation). But when the data was sorted by gender, the anxiety scores of neither the males nor the females showed a correlation with the changes in blood pressure and pulse rate (
Table 3).
Table 3
Correlation Coefficient between Spielberger's State-trait Anxiety Inventory Scale and Mean Blood Pressure/heart Rate during the Induction of Anesthesia
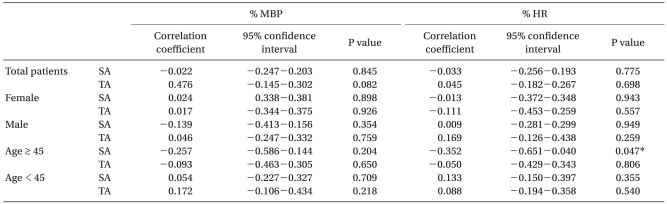

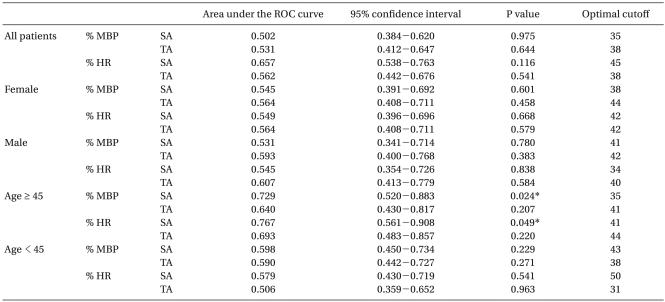
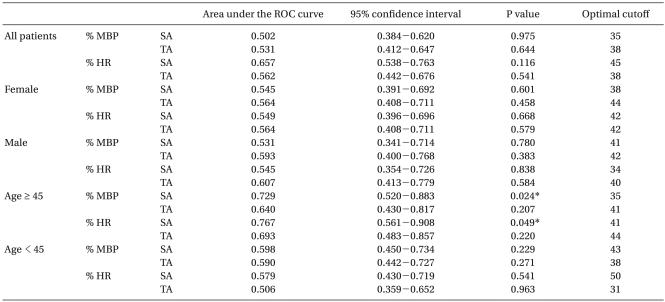
In the analysis to see if the state and trait anxiety subscale could predict a 20% or more change in blood pressure and pulse rate during anesthetic induction, the ROC analysis on the total patient group showed that state and trait anxiety scores were not appropriate predictors of hemodynamic changes related to anesthetic induction. This was the same for the gender-based analysis between the STAI scores and hemodynamic changes during anesthetic induction.
However, in the age-based analysis, the state anxiety scores of patients who were 45 years of age or older showed not only a close correlation with the change in heart rate (
Table 3) but also that the scores could be used to predict a 20% or more change in blood pressure during anesthetic induction (AUC = 0.729, P = 0.024) and 20% or more change in heart rate (AUC = 0.767, P = 0.049) (
Table 4).
Table 4
Analysis of Receiver Operating Characteristic (ROC) Curves and Determination of the Thresholds Spielberger's State-trait Anxiety Inventory Predicting the Occurrence of 20% Changes in mean Blood Pressure and Heart Rate during the Induction of Anesthesia

Go to :

Discussion
STAI scores usually range from 20 to 80. Anxiety is present when the score is above 50. In the current study, the mean state anxiety and trait anxiety scores were 43.8 and 42.7, respectively. Forty-eight patients scored 50 or more for state anxiety (48/111, 43%), and 31 patients scored 50 or more for trait anxiety (31/111, 28%). Because cancer patients, except thyroid cancer, were excluded from the study and the surgeries were relatively short and had low morbidity, the scores were slightly low. These scores were lower than what Boker et al. [
1] reported but were not very different from what Kindler et al. [
11] and Badner et al. [
12] reported. Preoperative anxiety reportedly occurs 11% of the time at the minimum [
13], or up to 80% of the time at the highest [
14]. However, these reports had unclear anxiety scales and uncontrolled preoperative measures and other factors. Therefore, the frequency in the current experiment was closer to the frequency found in controlled studies.
According to Sun et al. [
9], patient groups of 40 years of age and younger have increased prevalence of anxiety compared to other groups. The current study used the age 45 as the divider for the 2 age groups. A significant difference between the 2 groups was in their state anxiety scores. Unlike Sun et al.'s report, in this study, the older group had higher state anxiety scores. This difference may be due to the fact that the report by Sun et al. used a visual analog scale to measure the preoperative anxiety and may have defined anxiety more broadly. The current study used the STAI to distinguish state anxiety from trait anxiety and measured them separately, and this study aimed at seeing what affects a specific event, such as surgery, has on state anxiety. According to Spielberger et al., a specific event such as surgery has a close correlation with state anxiety [
15]. Although the current study used age 45 as the dividing age for the 2 age groups, Sun et al. qualified the younger group as 20 to 39. These differences in how the groups were defined may have played a part in the difference observed in the analysis results.
In the older age group, the increase in mean arterial pressure was greater. In the lower age group, the increase in pulse rate was greater. This may be because the older the patient is, the more of a varying effect the increase in catecholamine has on the cardiopulmonary system. Catecholamine increase in heart rate occurs more commonly in younger age groups. But in older groups, the rise in catecholamine increases mean arterial pressure even more noticeably [
16,
17]. However, the hemodynamic response was not proportional to the increase in the patient's age. The hemodynamic change due to tracheal intubation is greatest if the patient's age is between 40 and 50, according to Ismail et al. [
18], or 35 to 50, according to Bullington et al. [
19]. We chose age 45 as the dividing mark for the 2 ages groups after carefully reviewing Sun et al.'s report on anxiety and Ismail et al. and Bullington et al.'s reports on hemodynamic responses. At age 45 or above, the change in heart rate and the state anxiety was statistically significant. This means that an event like surgery can show that state anxiety, unlike trait anxiety, has a strong correlation with hemodynamic changes.
In the older age group, the analysis on whether state anxiety can predict hemodynamic changes during anesthetic induction showed that state anxiety proved to be valuable in predicting the change in mean arterial pressure and heart rate. This proves that patients with high preoperative state anxiety have high occurrences of hemodynamic changes during anesthetic induction. In a clinical practice, older patients with high state anxiety scores may experience great hemodynamic changes, so it is important to prepare for this. In older patients, the mean arterial pressure change does not show a correlation with state anxiety but appeared to be a significant predictor. This may be due to the method of statistical analysis.
In many other reports, females have been shown to have higher preoperative anxiety. In the current study, females had a higher mean STAI score than the males; however, no statistical significance was observed (mean state anxiety score; male = 42.1 < female = 45.3, mean trait anxiety score; male = 42.0 < female = 43.4). In addition, there was no difference between the genders in terms of hemodynamic change. This may be because there was no difference between the genders in the levels of anxiety. Or it may be because the difference in hemodynamic changes following anesthetic induction may not be related to gender. This requires further research.
To measure the patient's preoperative anxiety, the authors visited patients around 9-10 p.m. the night before their surgery and gave them questionnaires to fill out. The STAI has 40 questions, which takes too much time just before entering the operation room. Thus, conducting the STAI before entering the operation room was difficult. Lichtor et al. [
20] stated that a patient's anxiety level in the afternoon of the day before surgery was not different from the anxiety level of the patient before entering the operation room on the day of surgery. They stated that the anxiety level in the afternoon the day before surgery can predict the anxiety level of the day of surgery. Therefore, the measurements of anxiety levels in the current study may be seen as measurements right before surgery.
Patients with Mallampati classification III, who were assumed to have difficult tracheal intubation, were excluded, and the intubations were performed by one doctor. But the physical force used for each patient may have been different. However, according to Suh et al. [
21], the difference in the amount of force put on the soft tissue is irrelevant to the level of the circulatory system's response after laryngoscope manipulation. The reflex is caused by more than the threshold amount of stimuli. Therefore, variances in the patients' tracheal intubation environment causing misinterpretation of results do not have to be considered.
One of the limitations of the current study is that the change in blood pressure during tracheal intubation was not measured continuously. The stat mode was used, and blood pressure was not measured in real-time, so there was a time lapse when blood pressure was measured. However, tracheal intubation caused hemodynamic changes to occur within 10 seconds to 2 minutes [
22]. The exact highest blood pressure during tracheal intubation may not have been measured, but the current study measured the highest mean blood pressure within 1 minute after tracheal intubation. Direct arterial blood pressure measurement may have been more accurate and could have shown real-time results. However, since most patients in the study were healthy and did not require invasive blood pressure monitors, we could not take invasive measurements. In addition, the other problem was that the current study could not eliminate other factors affecting preoperative anxiety besides age and gender. Moreover, information on patients with past surgical experience and the varying levels of curiosity of the patients who had many questions on the surgery were not included in the research study, which limited the analysis. However, the sample number of patient subjects was adequate, so the authors think that the effects of the limitations on the results were low.
The current study illuminated the relationship between patients' preoperative anxiety and hemodynamics in tracheal intubation, and found the utility of state anxiety as a predictor of hemodynamic responses. Past studies focused on anesthetic maintenance as the measuring point of hemodynamics. However, the current study was different in that it focused on the anesthetic induction period when there is greater variance in hemodynamics. In addition, the current study found that, in predicting hemodynamic responses, state anxiety was more useful than trait anxiety.
In conclusion, the state anxiety of patients 45 years old and older was found to have a strong connection with the hemodynamic change during anesthetic induction and discovered to be an important predictor. Therefore, preoperative anxiety, especially the patient's state anxiety, should be given more attention. Older patients with high preoperative anxiety can be predicted to have more exaggerated hemodynamic responses, so more proactive measures in reducing these patients' preoperative anxiety should be taken. Attention should be given to hemodynamic responses during anesthetic induction to keep the patient safe from complications.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download