Abstract
Bronchial anthracosis was recently defined in the English radiology literature as a luminal narrowing associated with anthracotic pigmentation on bronchoscopy without a relevant history of pneumoconiosis or smoking. Anthracosis refers to the presence of carbon particles in the lungs, not to a disorder per se. Anthracofibrotic lesions carry the potential risk of massive hemorrhage during endobronchial procedures. This report describes a case of general anesthesia for a left modified radical mastectomy due to an intraductal carcinoma in a patient with known bronchial anthracofibrosis.
Endobronchial anthracofibrosis is a disease diagnosed by the endobronchail endoscopy findings of dark pigmentation (anthracosis) on the bronchial mucosa in patients without coniosis or a history of smoking that is associated with bronchial stenosis or an obstruction due to fibrosis in the same area [1-3]. In particular, most patients are not miners or lived in mining areas are non-smokers. Therefore, there is a strong possibility of the involvement of tuberculosis. An unexpected massive hemorrhage during the anesthetic management of anthracofibrosis patients can occur when physical stimulation is delivered to the lesion [4]. In the clinical anesthesia field, the possibility of such a condition is high in the following cases when endobronchial manipulation is performed frequently: in cases aspirating bronchial secretion after inserting a suction catheter through a endotracheal tube, cases whose bronchial management is difficult and require the use of a bronchial endoscope, and cases in whom a double lumen endotracheal tube is inserted during lung surgery. Considering that the incidence of tuberculosis in Korea is high, patients with anthracofibrosis could be encountered unexpectedly in clinics. Therefore, from the aspect of patient safety, it is very important to understand the physiology of this disease and during various endobronchial manipulations, and to pay close attention in advance to prevent the development of major complications, such as massive hemorrhage.
In Korea, in 2004, Huh and Kang et al. reported a case of anthracofibrosis in an 84-year-old male patient, who underwent a radical prostatectomy. A massive hemorrhage occurred in the airway due to endotracheal suction performed carelessly in the recovery room resulting in the patient's death, which could be considered to be a type of a mortality case report. The accurate incidence of anthracofibrosis in Koreans is unknown. Nevertheless, it is a disease that can be encountered frequently in tertiary medical institutions, such as university hospitals. Therefore, in our case, the definition of this disease, diagnostic methods, pathogenesis, and complications were examined carefully by a review of the literature.
Our case was a patient diagnosed with arthracofibrosis by bronchoscopic examination at another hospital prior to surgery. Based on this, a tuberculosis test was performed and the patient was diagnosed with tuberculosis. The patient underwent a modified radical mastectomy under general anesthesia. The experience of general anesthesia is described focusing on airway management.
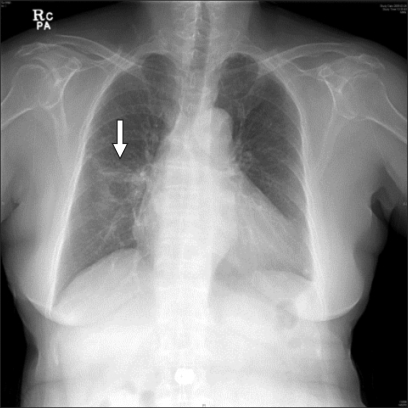
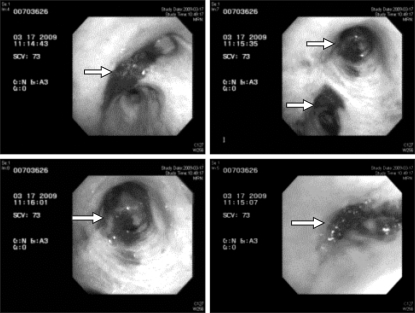
The patient was a 77-year-old female patient admitted for surgery for the chief complaint of an intraductal carcinoma in the left breast that was diagnosed at another hospital. Her height and weight was 150 cm and 68 kg, respectively. She had been diagnosed with hypertension 5 years earlier and was under medication. The plain chest radiographs taken 3 years earlier showed "no detection of abnormal findings", and dyspnea occurred during exercise from 2 years earlier. During a physical examination performed in March 2009, she was diagnosed with intraductal carcinoma in the left breast, 3.8 cm in size, with the possibility of invasion to the lower areola. In the presurgical tests, atelectasis in the right middle lobe was detected in plain chest radiographs (Fig. 1). The bronchial endoscopic examination revealed the deposition of dark pigmentation (anthracotic patches) in the distal area of the right main bronchus, right middle lobe, right lower lobe and area from the left upper lobe to the left lower lobe, as well as a narrowing of the bronchial lumen of the right middle lobe due to fibrosis (Fig. 2).
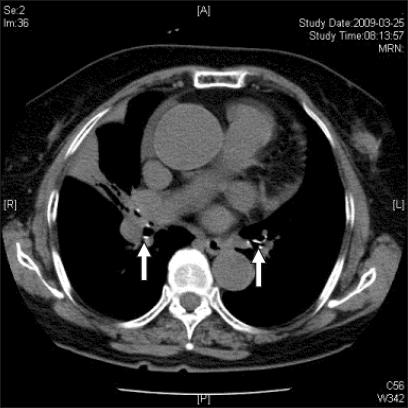
Chest computed tomography revealed atelectasis in the right middle lobe associated with a calcified and ruptured lymph node and anthracofibrosis in the entire airway (Fig. 3). The presurgical pulmonary function test showed a FVC, FEV1 and FEV1/FVC of 1.59 L (73%), 1.04 L (71%) and 66%, respectively. With the exception of a mild increase in liver enzymes in the blood test performed before surgery, no special findings were detected in the electrocardiogram, cardiac ultrasonography, and other tests. The patient tested positive to the M. tuberculosis polymerase chain reaction test performed after the bronchial endoscopic examination, and she was placed on antituberculosis medicines from 3 weeks before surgery.
For the induction of anesthesia, 200 mg thiopental, 50 mg rocuronium, and 50 µg fentanyl were injected, and the anesthesia was maintained with 2.0-2.5 vol% sevoflurane, 1 L/min oxygen, and 1 L/min Air. Because of the characteristics of the planned modified radical mastectomy, a large change in position from the supine position was not required, and a laryngeal mask airway (proseal #4) was used instead of endotracheal intubation to minimize airway stimulation. To reduce respiratory secretion, 0.2 mg glycopyrrolate was injected intramuscularly during the induction of anesthesia. In the preparation for airway hemorrhage that might occur accidentally during the perioperative period, an intensive care unit was prepared in advance and entered the operation room. After inducing anesthesia, the arterial blood pressure and central venous pressure were monitored by inserting a 20 G and 7 Fr, 3 lumen vascular catheter into the right radial artery and right internal jugular vein respectively. In arterial blood gas analysis performed at the initiation of surgery under the conditions of 0.5 FiO2, 37 mmHg EtCO2, and 100% SpO2, the pH was 7.480, pCO2 was 37.1 mmHg, pO2 was 286.0 mmHg, HCO3 was 27.0 mmol/L, BE was 3.4 mmol/L, Hb was 10.7 g/dl, Hct was 31%, Na was 136.0 mmol/L, K was 3.47 mmol/L, Ca was 1.03 mmol/L, and Glu was 89 mg/dl. During surgery, the respiratory tidal volume, respiratory rate, peak pressure and pulse oximetry saturation level was 360 ml per respiration, 10-14 times, 15 mmHg and 100%, respectively. The operation time was 1 hour 20 minutes, anesthesia time was 1 hour and 50 minutes, and surgery was completed without special events. Arterial blood gas analysis was performed at the time of the induction of mild hypercapnia by manual ventilation to recover self respiration and awaken the patient from anesthesia under the conditions of 0.5 FiO2, 45 mmHg EtCO2, and 100% SpO2. The results revealed a pH of 7.365, pCO2 of 49.5 mmHg, pO2 of 233.6 mmHg, HCO3 of 27.7 mmol/L, BE of 1.7 mmol/L, Hb of 11.1 g/dl, Hct of 33%, Na of 136.3 mmol/L, K of 3.45 mmol/L, Ca of 1.04 mmol/L, and Glu of 108 mg/dl. The results were similar to those obtained at the initiation of surgery. After the recovery of sufficient self respiration, the laryngeal mask airway was removed under the inflation state, and endotracheal suction was not performed. The patient did not cough severely or show a large amount of airway secretion. She recovered smoothly from anesthesia, and was transported to the ward via a recovery room.
Our patient was a 77-year-old female. In the past history, she did not live in a mining area, and farmed in Yeongcheon City, Gyeongsangbuk-do, which is believed to be less polluted than the larger cities. She moved to Seoul 40 years ago. She did not have prior history of tuberculosis or treatments for tuberculosis, and was a non-smoker. Therefore, the cause of the anthracofibrosis in this patient was speculated to be an undiagnosed tuberculosis infection. She was confirmed to have bronchial tuberculosis by the positivity for M tuberculosis polymerase chain reaction performed prior to surgery.
As the mechanism for the deposition of pigment within the bronchus and fibrosis associated with tuberculosis, there is a theory that inflammation in the tubercular lymph nodes induces tuberculosis in the endobronchus through the bronchial wall, resulting in pigment deposition and stenosis [6]. Consequently, endobronchial anthracofibrosis is the state of the development of the most undesirable sequelae of endobronchial tuberculosis. Chung and Lee suggested that endobronchial tuberculosis progresses in 6 stages. Among these stages, the infiltration of submucosal lymphocytes into the bronchus forms granulation tissues, and endobronchial stenosis occurs inevitably in cases in whom the disease progresses more than this decisive stage [5]. Therefore, the most important point in the treatment of endobronchial tuberculosis is not to miss the critical time. For this, a bronchial endoscopic examination is required for both diagnosis and treatment. The incidence of endobronchial tuberculosis is 5.88% of all tuberculosis patients [6]. Anthracofibrosis associated with tuberculosis and tubercular endobronchial diseases occur more often in females than males (2.4 times and 5.4 times, respectively) [6]. The typical characteristics of patients with bronchial stenosis due to anthracofibrosis are elderly women, without a prior history of pneumoconiosis or smoking, a chief complaint of cough without systemic symptoms or dyspnea, and findings of segmental or lobar consolidation on the plain chest radiographs. In addition, chest computed tomography reveals diverse bronchial abnormalities surrounded by soft tissue or lymph nodes. The most common invaded area is the right middle lobe bronchus, and an active tuberculosis infection is demonstrated in more than 60% patients [6], which concurs with the present findings.
A case of endobronchial anthracofibrosis was reported in this journal. Huh and Kang [7] reported a case of an 84-year-old male patient with undiagnosed endobronchial anthracofibrosis before surgery, who developed severe endobronchial hemorrhage after endotracheal suction by a routine method performed in the recovery room. In the recovery room, the hemorrhage began while inserting a suction catheter through an endotracheal tube and aspirating airway secretion. Although the blood was aspirated continuously, the volume did not decrease, and the patient was transported to the intensive care unit. Bronchial endoscopy was performed to stop the hemorrhage, where at that time, together with a large hematoma, bronchial fibrosis and the deposition of dark pigment in a wide area of the right main bronchus adjacent to the carina were detected. Endobronchial anthracofibrosis was diagnosed while treating the hemorrhage in the airway after surgery. The patient showed repeated deterioration and improvement, and acute respiratory distress syndrome developed on the day 5 after surgery. The patient died of multiple organ failure on day 63 after surgery. In our case, to reduce the risk of endobronchial hemorrhage, the amount of airway secretion was reduced using anticholinergic agents, and endotracheal suction using a suction catheter was not performed.
The entire length of the endotracheal tube (Mallincrodt medical Inc., Ireland) with a 7.0 mm inner diameter, which is generally used for the general anesthesia in adult women, is approximately 34 cm when it is firmly fitted with force to prevent the separation of the connector from a catheter. When a 12 Fr suction catheter (PVC suction catheter, Qingdao Sewoon medical Co. Ltd., China) was pushed to the end through this endotracheal tube, even the suction catheter completely passed the end of the endotracheal tube, and descends to the lumen of the bronchus by approximately 13 cm. If a 14 Fr suction catheter with a slightly larger inner diameter is used, it would enter the lumen of the bronchus by approximately 12 cm. Considering that the length of Korean women from the upper incisors to the carina is approximately 18.5-25 cm, a suction catheter could enter the lumen of the lobar bronchus readily [7]. In our case, pigment deposition plaque due to anthracofibrosis were formed at the distal area of right main broncus, and presented in the right middle and lower lobe and the left upper and lower lobe, too. Therefore, if endotracheal suction was performed without paying particular attention, a suction catheter possibly irritates the anthracofibrotic lesion at the distal area of the right main bronchus, and may induce the development of mass hemorrhage.
The standard guidelines for the airway management for the cases with anthracofibrosis have not been established. In cases placing endotracheal tubes, particularly during the recovery of anesthesia, severe cough may develop due to bronchial stimulation and more hemodynamic changes may occur during the insertion and removal of the endotracheal tube. It is possible that in cases using the laryngeal mask airway, as in our case, direct airway stimulation on the vocal cord and the proximal area of trachea could be decreased relatively. Nevertheless, if it is not installed accurately, saliva, etc. may be aspirated, which may cause airway irritation. In addition, in cases with obstructive lung diseases due to endobronchial anthracofibrosis, adequate ventilation may be impossible with the laryngeal mask airway only. In our case, sufficient ventilation was achieved only by the placement of a laryngeal mask airway, and the maintenance of anesthesia and recovery were achieved without a large amount of airway secretion. Similar to surgery that must use a laparoscope, for cases in whom an endotracheal tube must be inserted because of the characteristics of surgery itself requiring a high airway pressure, it would be desirable to assess the accurate position of anthracofibrosis lesions by performing a bronchoscopic examination in advance, to use agents that could reduce the level of airway secretion, and to restrain the use of a suction catheter as much as possible.
In conclusion, for anthracofibrosis patients, anesthesia plans should be made by considering the possibility of the development of severe hemorrhage within the bronchus if airway suction is performed without paying attention. In Korea, where the incidence of tuberculosis is high, there is a strong likelihood of undiagnosed endobronchail anthracofibrosis in elderly women. Therefore, it is important to minimize airway stimulation. If continuous abnormal hemorrhage is detected after endotracheal suction, it is important to consider the possibility of massive hemorrhage within the bronchus caused by underlying anthracofibrosis. In addition, in cases with anthracofibrosis findings detected accidentally during the endobronchial manipulation using a bronchoscope, it is highly probable that undiagnosed tuberculosis would be the cause. Therefore, a tuberculosis test should be performed after surgery.
References
1. Chung MP, Lee KS, Han J, Kim H, Rhee CH, Han YC, et al. Bronchial stenosis due to anthracofibrosis. Chest. 1998; 113:344–350. PMID: 9498950.

2. Kim HY, Im JG, Goo JM, Kim JY, Han SK, Lee JK, et al. Bronchial anthracofibrosis (inflammatory bronchial stenosis with anthracotic pigmentation). AJR Am J Roentgenol. 2000; 174:523–527. PMID: 10658734.

3. Kumar V. Robbins and Cotran Pathologic basis of disease. 2004. 7th ed. p. 39. p. 733.
4. Kim JY, Park JS, Kang MJ, Yu CG, Kim YH, Han SG, et al. Endobronchial anthracofibrosis is causally associated with tuberculosis. Korean J Med. 1996; 51:351–357.
5. Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000; 117:385–392. PMID: 10669679.

6. Abraham GC. Atelectasis of the right middle lobe resulting from perforation of tuberculus lymph nodes into bronchi in adults. Ann Intern Med. 1951; 35:820–835. PMID: 14878325.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download