Abstract
The central nervous system (CNS) is an important area of involvement for both high-grade, aggressive primary and secondary lymphomas. Although follicular lymphoma represents a low-grade histology, it may rarely present with CNS involvement. Here, we describe a patient diagnosed with follicular lymphoma who was presented with cerebellar involvement.
The central nervous system (CNS) is an important area of involvement for both high-grade, aggressive primary and secondary lymphomas. Although follicular lymphoma represents a low-grade histology, it may rarely present with CNS involvement [1]. Here, we describe a patient diagnosed with follicular lymphoma who presented with cerebellar involvement.
A 57-year-old male patient was referred to the Department of Internal Medicine with complaints of dizziness, dyspnea and respiratory distress when conducting daytime activities. The patient also had unexplained fever over 38℃, sweating and loss of several kilograms in 5-months, which are B symptoms of lymphomas. A plain chest radiography revealed massive bilateral pleural effusion and the thoracentesis fluid represented chylothorax. Computed tomography of the thorax, abdomen and pelvic areas showed bilaterally enlarged multiple conglomerated lymph nodes in the anterior and posterior cervical, supraclavicular, mediastinal, axillary, paraaortic, and inguinal regions. A biopsy of the supraclavicular lymph node revealed grade 2 follicular lymphoma (Fig. 1A-C). The tumor cells stained positive for CD20, CD10, bcl-2, and bcl-6, which is concordant with the B-germinal center cell phenotype. A bone marrow biopsy showed paratrabecular lymphoid infiltration of the B-cell phenotype, which is also consistent with follicular lymphoma infiltration. Based on these findings, the case was classified as stage IV-B disease according to the American Joint Committee on Cancer (AJCC) staging [2]. Therefore, according to our institutional chemotherapy regimen for B-cell lymphomas including follicular lymphoma, we administered six courses of rituximab-based cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) chemotherapy. The patient achieved complete response according to the Response Evaluation Criteria in Solid Tumors (RECIST) criteria [3] and was followed up regularly every three months for one year, until he applied again with complaints of painless left cervical swelling, dizziness and disequilibrium progressing over a six-week period. He did not experience any contributing symptoms such as vomiting, headache or fever. His physical examination, including neurological and ear systems and vital signs, were inconclusive. Plasma levels of the metabolic parameters including fasting glucose, serum electrolytes and liver and renal function tests were within normal ranges. F-18 fluorodeoxyglucose (FDG)-positron emission tomography/computed tomography revealed a right cerebellar diffuse intensity and left supraclavicular lymph nodes with high maximum standardized uptake value (SUV max) uptake levels of 11.3 and 12.3, respectively (Fig. 2A and B). Moreover, lesser degrees of FDG uptake were detected in inferior cervical lymph nodes, the right mastoid antrum and left supraspinatus muscle regions. Excisional biopsy of one of the left cervical lymph nodes showed grade 2 follicular lymphoma as previously described. These clinical and pathological findings were consistent with relapse of the primary disease. Brain magnetic resonance imaging showed a homogeneously-contrasted lesion, with a maximum diameter of 1.5 cm and isointense appearence of gray matter, involving the dural surface completely on posterior, inferior, and lateral regions of the right cerebellum. Internal contours of the lesion were rough and extended into the cerebellar sulcus. There were also milimetric nonspecific gliotic focuses on both areas of frontoparietal subcortical white matter on the magnetic resonance image (Fig. 2C). Taken together, these findings led to a diagnosis of concurrent dural and lepto-meningeal involvement. Therefore, a second-line chemotherapy regimen consisting of 350 mg/m2 rituximab on day 1, 20 mg/m2 fludarabine on days 1 to 3 and 240 mg/m2 cyclophosphamide on days 1 to 3 was started. Whole brain radiotherapy was sequentially administered at a dose of 300 cGy and was scheduled for 10×300 cGy. During the first-year follow-up period, the patient's symptoms and complaints were completely resolved and this case was assessed as a complete response according to the RECIST criteria [3].
Because follicular lymphomas generally have an indolent diasease course, they are often treated with follow-up alone. Follicular lymphoma is a rare cause of secondary CNS involvement, although CNS is an important area of involvement for both primary and secondary lymphomas. When present, the involvement is derived from dura mater in the majority of cases. In the last several years, there has been increasing awareness about the importance of keeping the possibility of CNS involvement in mind for patients with an aggressive disease course, regardless of the histological features of lymphoma [1]. This report discusses a patient with follicular lymphoma, an indolent variant of non-Hodgkin's lymphoma with grade 2 histology, who developped cerebellar involvement after one year of the initial diagnosis.
Aggressive B-cell lymphomas are often driven by the Epstein-Barr virus in immunosuppressed patients [4,5]. The lymphoma derived from the CNS are often located deep in the brain parencyhma near the ventricles, but they may also be derived from the dura in mostly indolent extranodal marginal zone lymphomas [6]. Conversely, systemic lymphomas may commonly affect the CNS secondarily; however, nearly all available reports have mentioned this occurrence in aggressive lymphomas, but not in indolent variants. In these situations, systemic B-cell lymphomas that have an effect have CNS involvement, leptomeninges or occassionally affect the dura.
To date, large series of lymphoma cases have been published describing secondary CNS involvement, predominantly by aggressive diffuse large B-cell lymphomas or highly aggressive Burkitt's lymphomas. However, some of these series included very rare examples (0.01%) of indolent lymphomas [11,12]. Unfortunately, these exceptional cases were not well characterized with regard to histological typing due to difficulties in obtaining tissue from the tumor site and they did not identify whether brain parenchyma, dura, and/or leptomeninges were affected or not. Moreover, the time interval between diagnosis and extranodal spread to the CNS was not well-defined in these few examples and, therefore, could not be used to determine whether transformation to an aggressive lymphoma had occurred. Past studies have indicated that follicular lymphomas are among the least frequent types of indolent lymphomas to be recognized with secondary CNS involvement [13]. Although the avilable literature describing indolent lymphomas does not report a tendency for CNS involvement, there may be exceptions. Indolent lymphomas may spread to the CNS, especially through later phases of the clinical course; therefore, the spread of lymphoma to the CNS may not be diagnosed or detected throughout the patient's life time [14].
Very few reports of patients with low-grade follicular lymhoma spreading to the CNS have been presented to date (Table 1) [5,7-10,15]. Four of the patients in these reported cases were in good condition after treatment, but one had progressive disease. The patient described in the present study was still in good health after completion of chemotherapy and radiotherapy treatments.
All five other cases reported in the literature were treated with surgery. Specifically, three of the patients received combination therapy and four received radiotherapy. The outcome data for one patient is not available, one had progressive disease after 8 months, and the three other patients showed no evidence of disease for more than 1 year. In our case, we were not able to perform surgical resection because the tumor was located on the posterior, inferior and lateral regions of the right cerebellum, which made it unresectable.
In conclusion, the disease course of follicular lymphoma after secondary CNS involvement was indolent in contrast to aggressive lymphoma; therefore, these patients may have to be treated more aggressively using chemotherapy and/or radiotherapy. Currently, with rituximab-based CHOP chemotherapy, patients now attain a longer survival, which may cause unusual disease progression due to longevity. Lymphoma experts including oncologists, internists, neuroradiologists, and pathologists should always be in cooperation and be mindful of the different patterns of CNS involvement to enable correct diagnosis and management schedules of lymphoma.
References
1. Hollender A, Kvaloy S, Lote K, Nome O, Holte H. Prognostic factors in 140 adult patients with non-Hodgkin's lymphoma with systemic central nervous system (CNS) involvement: a single centre analysis. Eur J Cancer. 2000; 36:1762–1768. PMID: 10974623.

2. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging handbook. 7th ed. New York: Springer;2010.
3. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247. PMID: 19097774.

4. Kleinschmidt-DeMasters BK, Gilden DH. The expanding spectrum of herpesvirus infections of the nervous system. Brain Pathol. 2001; 11:440–451. PMID: 11556690.
5. Grupka NL, Seinfeld J, Ryder J, Lillehei KO, Kleinschmidt-Demasters BK. Secondary central nervous system involvement by follicular lymphoma: case report and review of the literature. Surg Neurol. 2006; 65:590–594. PMID: 16720183.

6. Kumar S, Kumar D, Kaldjian EP, Bauserman S, Raffeld M, Jaffe ES. Primary low-grade B-cell lymphoma of the dura: a mucosa associated lymphoid tissue-type lymphoma. Am J Surg Pathol. 1997; 21:81–87. PMID: 8990144.
7. Beriwal S, Hou JS, Miyamoto C, Garcia-Young JA. Primary dural low grade BCL-2 negative follicular lymphoma: a case report. J Neurooncol. 2003; 61:23–25. PMID: 12587792.
8. Low I, Allen J. Low-grade follicular lymphoma in the dura: rare mimic of meningioma. Neuropathology. 2006; 26:564–568. PMID: 17203594.

9. Hamilton DK, Bourne TD, Ahmed H, Cousar JB, Mandell JW, Sheehan JP. Follicular lymphoma of the dura: case report. Neurosurgery. 2006; 59:E703–E704. PMID: 16955025.
10. Riccioni L, Morigi F, Cremonini AM. Follicular lymphoma of the dura associated with meningioma: a case report and review of the literature. Neuropathology. 2007; 27:278–283. PMID: 17645243.

11. MacKintosh FR, Colby TV, Podolsky WJ, Burke JS, Hoppe RT, Rosenfelt FP, et al. Central nervous system involvement in non-Hodgkin's lymphoma: an analysis of 105 cases. Cancer. 1982; 49:586–595. PMID: 7059915.

12. Hoerni-Simon G, Suchaud JP, Eghbali H, Coindre JM, Hoerni B. Secondary involvement of the central nervous system in malignant non-Hodgkin's lymphoma: a study of 30 cases in a series of 498 patients. Oncology. 1987; 44:98–101. PMID: 3574856.
13. Tomita N, Kodama F, Sakai R, Koharasawa H, Hattori M, Taguchi J, et al. Predictive factors for central nervous system involvement in non-Hodgkin's lymphoma: significance of very high serum LDH concentrations. Leuk Lymphoma. 2000; 38:335–343. PMID: 10830740.

14. Jellinger K, Radiaszkiewicz T. Involvement of the central nervous system in malignant lymphomas. Virchows Arch A Pathol Anat Histol. 1976; 370:345–362. PMID: 826017.

15. Spectre G, Gural A, Amir G, Lossos A, Siegal T, Paltiel O. Central nervous system involvement in indolent lymphomas. Ann Oncol. 2005; 16:450–454. PMID: 15642707.

Fig. 1
(A) Form and structure that eliminates the normal pattern of lymph node in folliculary lymphoma (H&E staining, ×40). (B) CD-20 positivity in the follicle (×40). (C) Bcl-2 positivity in the follicle center (×40).
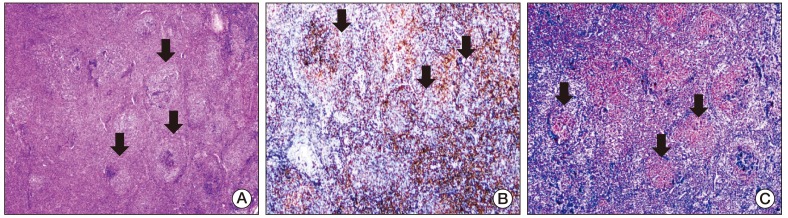
Fig. 2
(A) F-18 fluorodeoxyglucose-positron emission tomography/computed tomography (F-18 FDG-PET/CT) showing a right cerebellar diffuse intensity with high maximum standardized uptake value (SUV max) levels of 11.3. (B) F-18 FDG-PET/CT showing aleft supraclavicular lymph nodes with high SUV max levels of 12.3. (C) The brain magnetic resonance imaging showing a homogen-contrasted lesion, with a maximum 1.5 cm diameter and isointence appearence to gray mater, involving dural surface totally on posterior, inferior, and lateral regions of the right cerebellum.
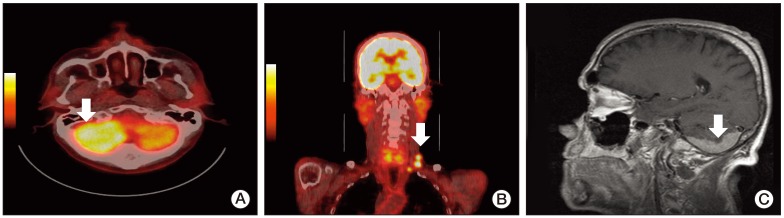
Table 1
PubMed data of indolent lymphoma cases with central nervous system involvement




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download