This article has been
cited by other articles in ScienceCentral.
Abstract
Mucoepidermoid carcinoma in the external auditory canal is extremely rare. Strategies used for treatment of mucoepidermoid carcinoma remain controversial. We present a case of mucoepidermoid carcinoma of the external auditory canal. The patient underwent lateral temporal bone resection and the surgical defect was obliterated with temporal muscle. He is currently disease-free, four years after surgery. Proper diagnostic measures and strategy for treatment of mucoepidermoid carcinoma are discussed.
Go to :

Keywords: Mucoepidermoid carcinoma, Ear canal, Temporal bone
Introduction
Malignant lesions of the external auditory canal (EAC) are rare. Squamous cell carcinoma followed by adenoid cystic carcinoma and basal cell carcinoma is a more common type of EAC malignancy, whereas mucoepidermoid carcinoma is extremely rare. Only four cases of mucoepidermoid carcinoma arising from the EAC have been reported in the English literature [
1-
4]. One additional case has been reported in Korea [
5]. Symptoms of EAC malignancy are often nonspecific and are similar to those of external otitis. Thus, definite diagnosis could be delayed, resulting in an advanced tumor stage at the time of diagnosis. We report on a case of mucoepidermoid carcinoma of the EAC with a review of the literature, and suggest proper treatment of mucoepidermoid carcinoma in the EAC.
Go to :

Case Report
A 24-year-old male patient presented with bloody otorrhea, ear fullness, and foreign body sensation in the left EAC. He first noticed the bloody otorrhea one year prior to visiting the otolaryngologist and felt a small mass in the EAC while cleaning out the discharge using an ear pick. He denied hearing loss, tinnitus, and vertigo, but complained of intermittent ear fullness. Facial nerve function was intact. On the otoscopic examination, a pinkish mass was observed in the bony-cartilaginous junction of the postero-superior portion of the EAC (
Fig. 1A). The mass measured less than 8 mm in size. Normal tympanic membrane was visible through the space between the mass and EAC wall. A punch biopsy was performed, and the mass was diagnosed as intermediate grade mucoepidermoid carcinoma (
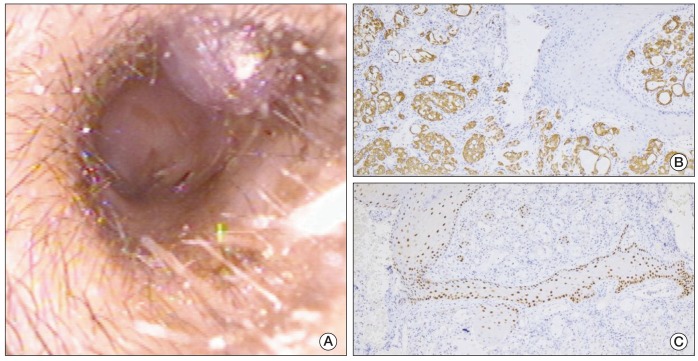
Fig. 1B and C). A high-resolution temporal bone computed tomography (CT) scan with contrast and fluorine-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography (PET)/CT scan were performed for evaluation of the extent of the mass and for detection of distant metastasis. A slightly enhanced protruding lesion measuring approximately 1.2 cm in size in the posterior aspect of the EAC was observed on the CT scan. The lesion was confined to the EAC and did not invade the parotid gland or adjacent bony structures. A faint FDG uptake was observed in the left EAC with a peak standard uptake value of 1.12, and no other abnormal absorption of the F-18 FDG was observed in distant organs (
Fig. 2). According to the University of Pittsburgh staging system for EAC carcinoma, the lesion was classified as T1N0M0 [
6]. A lateral temporal bone resection was performed through a retroauricular approach. In the operative view, the mass was firm and pink; it was removed
en bloc with the cartilaginous and bony EAC and tympanic membrane. A part of the temporal muscle was rotated in order to obliterate the surgical defect. A small retroauricular lymph node was observed and confirmed as "reactive hyperplasia" by frozen biopsy. No pathologic lymph nodes were observed at the parotid area and the facial nerve was intact in the operative field. Despite the risk of regional metastasis in intermediate-grade mucoepidermoid carcinoma, considering the early stage of disease and the patient's young age, neck dissection and parotidectomy were not performed in this patient. The final pathologic diagnosis was intermediate grade mucoepidermoid carcinoma confined to the EAC. Post-operative facial nerve function was normal. We obliterated the EAC with the temporal muscle, resulting in destruction of the sound transmission system of the middle ear. The patient suffered post-operative unilateral conductive hearing loss; however, the hearing level in the contralateral ear was normal. He did not want to use bone conduction hearing aids. In the four years of follow-up since surgery, there have been no signs of recurrence and no abnormal uptake of F-18 FDG has been observed on F-18 FDG PET/CT scans.
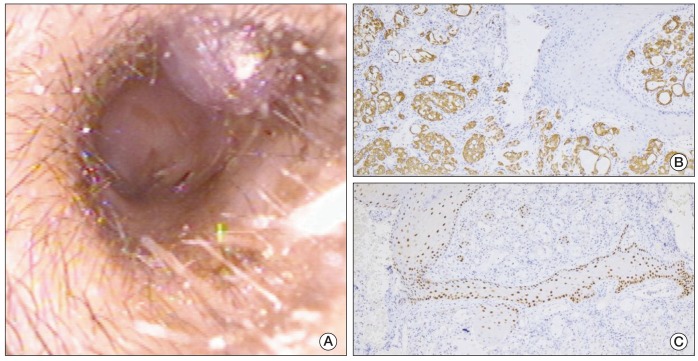 | Fig. 1Otoscopic findings of the left ear (A) and pathologic findings (B, C). (A) A pinkish mass was observed at the postero-superior portion of the external auditory canal. Normal tympanic membrane was observed. (B) Immunohistochemical staining of p63 revealed staining of the basal cell layer of epithelium (×100). (C) Immunohistochemical staining of cytokeratin 20 showed staining of cytoplasm of mucinous cells (×200). 
|
 | Fig. 2Temporal bone computed tomography (CT) with contrast enhancement (A) and fluorine-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography/CT scan (B). (A) A well-enhanced protruding skin lesion measuring 1.2 cm was observed at the postero-superior aspect of the external auditory canal. (B) Faint F-18 FDG uptake in the left external auditory canal was observed. The peak standard uptake value was 1.12. No distant metastasis was observed. 
|
Go to :

Discussion
Mucoepidermoid carcinoma is a malignant tumor that frequently originates in the major and minor salivary glands and also occurs in other glandular structures in both normal anatomic and ectopic sites. Thus, the ceruminous gland of the deep dermis in the EAC is a possible site of growth. However, the actual pathogenesis is not known [
1].
On otoscopy, mucoepidermoid carcinoma does not differ from other types of malignancy, and histologic confirmation is essential to diagnosis. Under histologic examination, mucoepidermoid carcinomas appear to be composed of scattered, solid and cystic mucinous areas. Due to the mixed components, classification is based on the proportion of the solid part that is present.
In low-grade tumors, there is a high percentage of mucinous cells and cystic or microcystic structures. High-grade tumors consist of solid nests or cords of mostly squamous cells. Therefore, with regard to its epithelial components, high-grade mucoepidermoid carcinoma is very similar to poorly differentiated squamous cell carcinoma. Histologic grade plays a major role in treatment and prognosis of mucoepidermoid carcinoma.
Currently, there is no consensus regarding the appropriate staging and treatment of mucoepidermoid carcinoma in the EAC. The University of Pittsburgh staging system for the EAC is widely used for squamous cell carcinoma; however, its applicability to mucoepidermoid carcinoma of the EAC remains uncertain [
6]. In the general treatment of EAC cancers, a tumor confined to the cartilaginous EAC may be managed sufficiently with sleeve resection of the EAC. When a tumor invades the bony canal, a lateral temporal bone resection should be performed, and, in the case of middle ear involvement, subtotal temporal bone resection should be performed. Mucoepidermoid carcinoma of the EAC is extremely rare and its characteristics can differ significantly from those of squamous cell carcinoma; therefore, precise guidelines for treatment and treatment strategies have not been established [
7].
Magliulo et al. [
3] reported on a case of T2, intermediate-grade mucoepidermoid carcinoma arising from the bony-cartilage junction of the EAC. The patient underwent lateral temporal bone dissection, total parotidectomy, and unilateral elective neck dissection without postoperative radiotherapy. Histologic examination showed no cartilage or parotid gland involvement. The authors warned of hidden metastasis in intermediate and high-grade mucoepidermoid carcinoma and recommended an aggressive treatment strategy, including elective neck dissection [
3]. However, Bared et al. [
1] reported a step-by-step surgical approach for malignancies of the EAC in order to minimize operative morbidity and postoperative dysfunction based on the histologic type and extent of disease. Malignancies of the EAC have a poor prognosis and a high rate of recurrence; therefore, most authors advocate aggressive treatment at the time of diagnosis. On the other hand, an aggressive approach to treatment is associated with higher risk of postoperative morbidity, including hearing loss and facial nerve dysfunction. In treatment of mucoepidermoid carcinoma of the EAC, both oncologic outcome and surgical morbidity must be considered.
Our case was a T1N0M0 intermediate-grade mucoepidermoid carcinoma limited to the EAC, and was treated with lateral temporal bone dissection. We thought that elective neck dissection and postoperative radiotherapy were not necessary in the early stage of disease; therefore, parotidectomy, elective neck dissection, and postoperative radiotherapy were deferred. Thus, we achieved minimal postoperative morbidity and normal facial nerve function. So far, during the four years following surgery, no evidence of recurrence has been found on physical examination and F-18 FDG PET/CT scans. Continuation of careful follow-up is planned for detection of any recurrence.
Based on this case, we suggest that lateral temporal bone resection is an appropriate surgical method for treatment of early stage mucoepidermoid carcinoma arising from the EAC. For establishment of a general treatment strategy, further study including a larger number of cases will be necessary.
Go to :






 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download