Abstract
Purpose
The aim of the current study was to determine the incidence, clinical presentation, and treatment outcomes of "bone-only metastases" in patients with breast cancer and to analyze the impact of hormone receptor (HR) and human epidermal growth factor receptor 2 (HER2) status on prognosis.
Materials and Methods
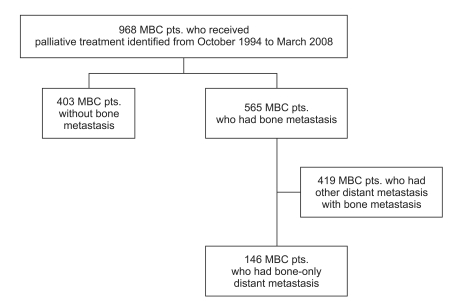
Between 1994 and 2007, of 968 patients with metastatic breast cancer who underwent palliative management at Samsung Medical Center, 565 (57%) relapsed with distant metastases. Of the 968, 146 (15%) had bone-only metastases during a median follow-up period of 75 months. Among the 146 patients with bone-only metastases, 122 (84%) were relapsed patients after curative surgery and 24 (26%) were initially metastatic cases.
Results
The median time from primary surgery to bone-only metastases of the 122 patients was 37 months (95% confidence interval [CI], 27 to 46 months). Bone-only metastases were more common in the HR-positive group than in the other subtypes (85% for HR+; 8.2% for HER2+; 6.8% for triple negative. Among all 146 patients, 75 (51%) were treated with hormone therapy. The median post-relapse progression-free survival was 15 months (95%CI, 13 to 17 months). The median overall survival was much longer in the HR+ patients than the HER2+ and triple negative breast cancer patients with marginal statistical significance (65 vs. 40 vs. 40 months, p=0.077).
Conclusion
Breast cancer patients with "bone-only metastases" had excellent clinical outcomes. Further study is now warranted to reveal the underlying biology that regulates the behavior of this indolent tumor, as it should identify 'favorable tumor characteristics' in addition to 'favorable preferential metastatic site.'
Bone is the most common site of metastatic recurrence in breast cancer and bone metastases are a major cause of morbidity for patients with metastatic breast cancer (MBC) [1]. Bone represents the first site of metastasis in >50% of patients who fail systematically [2,3]. After Sherry et al. [4,5] reported that MBC confined to the skeletal system is highly responsive to treatment and associated with prolonged survival, the concept of bone-only metastasis as a first site of relapse emerged. Bone-only metastasis means bone metastasis without evidence of any other organ involvement. Although metastatic spread to most end organs occurs by similar mechanisms [6,7], and survival is almost always poor in patients with extensive disease involving multiple organs, bone-only metastasis in breast cancer patients appears to show a relatively good prognosis [2,4,5,8]. For endocrine-sensitive breast cancer, the National Comprehensive Cancer Network (NCCN) guideline recommends endocrine therapy for the management of MBC confined to the bone and soft tissue [9].
One of the most intriguing biological aspects of metastasis is the pattern of organ dissemination [10]. Aggressive tumor cells typically enter the blood stream and reach distant tissues. This dissemination has stereotypical patterns of organ tropism that reflects the heterogeneity of tumor cells and depends on the cancer type. Estrogen receptor (ER)-positive tumors preferentially spread to bone. Recent data supports the view that bone metastasis is associated with the absence of Wnt signaling [11]. Considering that most bone metastases are associated with an indolent disease course and clinical dormancy, these cases may have characteristic clinical features with predominance of dormancy over aggressive metastatic disseminations.
Hence, we undertook this study; 1) to determine the incidence, clinical course, and treatment outcomes for breast cancer patients with of "bone-only metastases"; and 2) to analyze the impact of hormone receptor and human epidermal growth factor receptor 2 (HER2) status on the prognosis of this group.
We retrospectively reviewed the medical records of patients with pathologically-confirmed invasive breast cancer who received palliative management between October 1994 and March 2007 at Samsung Medical Center. Among 968 MBC patients who had distant relapse, 565 (58.4%) had bone metastases. Of the 565, 146 (25.8%) had bone-only metastasis as the first distant site of relapse. Bone-only metastasis was defined as bone metastasis without evidence of involvement of any other organ. The following patient information was obtained from medical records: gender; age; prior treatment; primary treatment after bone metastasis; presence of progression to other metastatic sites; distant relapse-free survival (DRFS); post-relapse overall survival (PR-OS); and PR progression-free survival (PFS).
ER and progesterone receptor (PgR) positivity was defined as an Allred score from 3-8 by immunohistochemistry (IHC) using antibodies to the ER (Immunotech, Paris, France) and PgR (Novocastra, Newcastle, UK). HER2 status was evaluated using an antibody (Dako, Carpinteria, CA) and/or fluorescence in situ hybridization (FISH). Grades 0 and 1 for HER2 by IHC were defined as a negative result, and grade 3 as a positive result. Amplification of HER2 was confirmed by FISH if HER2 was rated 2+ by IHC. All core biopsies from referral institutes were reviewed by experienced pathologists in our institute including IHC staining at the time of initial referral. The pathology reviews for all surgical specimens were done prospectively and comprehensively by experienced pathologists in our institute. Our study protocol was approved by the Institutional Review Board of Samsung Medical Center.
After documentation of bone metastasis, patients received palliative local and/or systemic treatment. The agents used in hormonal therapy included tamoxifen, goserelin, and aromatase inhibitors (letrozole and anatrozole), according to menopausal status. Systemic chemotherapeutic regimens, including doxorubicin and taxanes, were given at the physician's discretion or the patients' preference. Anti-HER2 therapy with chemotherapy or hormonal therapy was administered for HER2 overexpressing metastatic breast cancer. Bisphosphonate treatment was performed at the physician's discretion, with or without hormonal therapy and/or chemotherapy.
DRFS was defined as the time from the date of curative surgery of breast cancer to the date of documentation of distant relapse. PR-OS was measured from the date of distant relapse to the date of death or the last follow-up day. PR-PFS was measured from the date of distant relapse to the date of documented disease progression or death. PR-PFS (other distant) was confined to progression to other distant metastasis besides progression to bone metastasis. PFS and OS were defined as the same for all 146 patients with bone-only metastases including 24 patients presented as stage IV at the time of diagnosis.
Clinicopathologic variables were compared between the "bone-only metastasis" group and the "other metastasis" group, and hormone receptor-positive and -negative patients in the bone-only metastasis group using the Pearson chi-square (χ2) test and Fisher's exact test for categorical variables. Survival curves were calculated using the Kaplan-Meier method and compared with other prognostic variables using the log-rank test. A p-value<0.05 was considered significant. A Cox proportional hazards regression model was used to assess the effect of each potential prognostic variable on PR-OS and PR-PFS.
The median duration of follow-up of all 146 patients with bone-only metastases was 75 months (range, 28 to 124 months).
The clinical characteristics of the patients who relapsed with bone metastasis only are summarized in Table 1. The median age was 47 years (range, 18 to 76 years). High nuclear and histologic grades were noted in 24.7% and 26.7%, respectively. Eighty-five percent were ER+ and/or PR+; the rest were HER2+ (8.2%) and triple negative breast cancer (TNBC) (6.8%). Of the 146 patients, 122 (83.6%) relapsed to bone metastasis after surgery; the remaining 24 (16.4%) were initially metastatic. Among the 122 (83.6%) relapsed patients, 91.8% received adjuvant hormonal therapy. Single bone metastasis occurred in 23.3% of the patients. The median number of involved bones was 2 (range, 1 to 5). Extensive bone metastases, defined as≥10 bones being involved with or without bone destruction or soft tissue formation, were demonstrated in 23.3%. The most commonly involved bone was the spine (55.5%). After palliative treatment, common progression sites were bone (73.3%) and lung (19.2%). The progression site was limited to bone in 55.5% of patients. The main treatment modality was hormonal therapy with or without radiation (45.9%). Systemic chemotherapy was administered to 28.1% of patients with or without radiation. Bisphosphonate therapy was administered to 68.5% of patients. The median time of bisphosphonate therapy was 15.6 months (range, 0.7 to 71.9 months). The 5-year survival rate after documentation of bone metastasis for a median follow-up duration of 75 months was 52.3%.
HR+ patients had superior, but not statistically significant metastatic OS compared to HER2+ and TNBCs patients (Fig. 2). The median PR-OS of HR+ breast cancer patients was 65 months. Conversely, the median OS of both HER2+ and TNBCs patients was 40 months, respectively (p=0.077).
Comparing the 34 patients with a single bone metastasis to the 112 patients with multiple bone metastases, much better outcomes (in terms of PR-PFS and PR-OS) occurred in patients with single bone metastasis, as expected. Median PR-PFS values for patients with single and multiple bone metastases were 24 and 14 months, respectively (p=0.002) (Fig. 3A). Median PR-OS values for these patients were 79 and 50 months (p=0.005) (Fig. 3B).
We divided patients into two groups according to a DRFS of 36 months in order to characterize metastatic behavior of bony preferences of metastasis in terms of the time of metastasis. There were significant differences in mean age, histologic grade, adjuvant hormonal therapy, and involved bone sites between patients who had a DRFS of ≥36 months and those who had an DRFS<36 months (Table 2). The numbers of patients for each group were 60 and 62, respectively. The mean age was younger in patients with a DRFS <36 months than in patients with a DRFS≥36 months (46 years vs. 50 years, p=0.041 by t-test). More patients with a DRFS≥36 months were HR+ than patients with a DRFS<36 months, but statistical significance was not reached (91.8% vs. 80.0%, p=0.156). Higher histologic grade (54.8% vs. 35.0%, p=0.072) and nuclear grade (50.0% vs. 26.7%, p=0.024) were more common in patients with a DRFS<36 months. The spine was more commonly involved in patients with a DRFS<36 months (62.1% vs. 43.5%, p=0.042). The sternum was not frequently involved in patients with a DRFS <36 months (8.6% vs. 27.4%, p=0.009). Adjuvant hormonal therapy was administered for patients with a DRFS≥36 months more commonly than patients with a DRFS<36 months (80.0% vs. 55.9%, p=0.005). A greater percentage of patients with a DRFS<36 months had liver (25.0% vs. 6.7%, p=0.011) and lung progression (26.7% vs. 11.7%, p=0.037) than patients with a DRFS≥36 months. The 1-year PR-progression free survival rate was 53.8% vs. 62.5%; the 5-year overall survival rate (OSR) was 50.0% vs. 72.6% (p=0.010).
Single bone metastasis was identified as a favorable independent prognostic factor for PR-OS (hazard ratio [HR], 0.280; p=0.003) with a DRFS≥36 months (HR, 0.280; p=0.038). High histologic grade was identified as an unfavorable independent risk factor for PR-OS (HR, 3.211; p=0.005).
Breast cancer with bone-only metastases is thought to be associated with a relatively favorable prognosis compared with breast cancer with other visceral metastatic sites. Clearly, breast cancer preferentially spreads to bone [12,13]. According to Paget's "seed" and "soil" hypothesis, the perceived compatibilities between disseminated cancer cells (the seed) and certain distant sites (the soil) have long influenced the view of the metastatic process [14]. Considering that metastasis is the end product of an evolutionary process involving diverse interactions between cancer cells and their microenvironment, bone metastasis may be a good example to show a favorable outcome with the indolent disease course of breast cancer, even when there is distant metastasis. Recurrence after curative resection and durable remission is not infrequent. In fact, 20-45% of patients with breast cancer relapse years or decades later [15-17]. To address the role of bone as a single distant end organ in the metastatic process of breast cancer, we analyzed late-onset relapse with a DRFS≥36 months separately. According to our results, late-onset relapses after a DRFS≥36 months developed more in the HR+ subgroup with a low histologic grade (Table 2). In addition, these late-onset relapses confined to bone showed an excellent outcome of 72.6% in terms of the 5-year PR-OSR. The objective tumor burden as metastasis proceeds might be the main problem. A pause in progression has to be considered the most likely explanation for the discrepancy between the estimated and observed disease-free periods [18]. To understand this dormancy, cells must be characterized during the dormant state. Given the results that many of the late-onset bone-only metastatic breast cancers progressed to bone with visceral metastasis, bone may provide a good microenvironmental condition to maintain the 'dormant state.'
Traditionally, this 'favorable preference to the bone' in breast cancer is known to have a relationship with the ER [15,19,20]. The rate of late-onset metastasis was significantly higher in ER+ cases. ER+ breast tumors relapse most prominently to the bones over a protracted period [20]. Furthermore, the overall rate of bone metastasis and the rate of late-onset bone metastasis were significantly higher in ER+ cases than in ER- cases [21,22]. This finding is also supported by our data. Most of the breast cancer subtypes in bone-only metastasis were HR+ (Table 2). Recently, some plausible data explaining the relationship between ER and bone metastases has been reported. Specifically, transforming growth factor-β/bone morphogenic proteins have been reported to have a role in bone metastasis together with the epithelium-to-mesenchyme transition [21]. In addition, there is a report that Src selectively promotes bone metastasis in ER+ breast cancers and supports the idea that there is survival of indolent breast cancer cells in bone marrow [19]. Src is the prototypic member of the non-receptor tyrosine kinase family. Src participates in the activation of various downstream pathways through molecular interactions with growth factor receptors (epidermal growth factor receptor and HER2), integrin cell adhesion receptors, steroid hormone receptors, G protein-coupled receptor, focal adhesion kinase, and cytoskeleton components [23]. The importance of these candidate biomarkers is increased by the urgent need for development of new treatment targets as well as for understanding tumor biology. The identification of mechanisms that support the survival of disseminated cancer cells in their host microenvironments has clear implications for improving the treatment of latent metastatic disease. Survival of indolent and latent tumors eventually results in tumor recurrence. Thus, further prolongation of latency or a permanent stop in dormancy can be equated to 'cancer-free' life.
Cleary, this study was limited by its being a retrospective analysis and by the small size of the bone-only metastases group. Despite these drawbacks, our study successfully demonstrated the clinical characteristics and disease course of bone-only metastases in breast cancer patients. This is from a homogeneous cohort from a single institution with a sizable sample and a long follow-up duration.
The bone-only metastases in breast cancer show excellent clinical outcomes, which developed mainly in the HR+ subgroup. A further study to determine how to regulate this indolent tumor behavior is warranted because it would help identify 'favorable tumor characteristics' in addition to 'favorable preferential metastatic site.'
References
1. Coleman RE. Skeletal complications of malignancy. Cancer. 1997; 80(8 Suppl):1588–1594. PMID: 9362426.

2. Coleman RE, Rubens RD. The clinical course of bone metastases from breast cancer. Br J Cancer. 1987; 55:61–66. PMID: 3814476.

3. Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999; 49:33–64. 1PMID: 10200776.

4. Sherry MM, Greco FA, Johnson DH, Hainsworth JD. Breast cancer with skeletal metastases at initial diagnosis. Distinctive clinical characteristics and favorable prognosis. Cancer. 1986; 58:178–182. PMID: 2423224.

5. Sherry MM, Greco FA, Johnson DH, Hainsworth JD. Metastatic breast cancer confined to the skeletal system: an indolent disease. Am J Med. 1986; 81:381–386. PMID: 2428242.
6. Lee YT. Patterns of metastasis and natural courses of breast carcinoma. Cancer Metastasis Rev. 1985; 4:153–172. PMID: 3893684.
7. Kamby C, Ejlertsen B, Andersen J, Birkler NE, Rytter L, Zedeler K, et al. The pattern of metastases in human breast cancer: influence of systemic adjuvant therapy and impact on survival. Acta Oncol. 1988; 27:715–719. PMID: 3219223.

8. Coleman RE, Smith P, Rubens RD. Clinical course and prognostic factors following bone recurrence from breast cancer. Br J Cancer. 1998; 77:336–340. PMID: 9461007.

9. Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, et al. Breast cancer: clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2009; 7:122–192. PMID: 19200416.

10. Nguyen DX, Massagué J. Genetic determinants of cancer metastasis. Nat Rev Genet. 2007; 8:341–352. PMID: 17440531.

11. Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JG, et al. Subtypes of breast cancer show preferential site of relapse. Cancer Res. 2008; 68:3108–3114. PMID: 18451135.

12. Chiang AC, Massagué J. Molecular basis of metastasis. N Engl J Med. 2008; 359:2814–2823. PMID: 19109576.

13. Lacroix M. Significance, detection and markers of disseminated breast cancer cells. Endocr Relat Cancer. 2006; 13:1033–1067. PMID: 17158753.

14. Paget S. The distribution of secondary growths in cancer of the breast. Lancet. 1889; 133:571–573.

15. Karrison TG, Ferguson DJ, Meier P. Dormancy of mammary carcinoma after mastectomy. J Natl Cancer Inst. 1999; 91:80–85. PMID: 9890174.

16. Pfitzenmaier J, Ellis WJ, Arfman EW, Hawley S, McLaughlin PO, Lange PH, et al. Telomerase activity in disseminated prostate cancer cells. BJU Int. 2006; 97:1309–1313. PMID: 16686730.

17. Weckermann D, Müller P, Wawroschek F, Harzmann R, Riethmüller G, Schlimok G. Disseminated cytokeratin positive tumor cells in the bone marrow of patients with prostate cancer: detection and prognostic value. J Urol. 2001; 166:699–703. PMID: 11458120.

18. Demicheli R. Tumour dormancy: findings and hypotheses from clinical research on breast cancer. Semin Cancer Biol. 2001; 11:297–306. PMID: 11513565.

19. Zhang XH, Wang Q, Gerald W, Hudis CA, Norton L, Smid M, et al. Latent bone metastasis in breast cancer tied to Src-dependent survival signals. Cancer Cell. 2009; 16:67–78. PMID: 19573813.

20. Schmidt-Kittler O, Ragg T, Daskalakis A, Granzow M, Ahr A, Blankenstein TJ, et al. From latent disseminated cells to overt metastasis: genetic analysis of systemic breast cancer progression. Proc Natl Acad Sci U S A. 2003; 100:7737–7742. PMID: 12808139.

21. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005; 365:1687–1717. PMID: 15894097.
22. Hess KR, Pusztai L, Buzdar AU, Hortobagyi GN. Estrogen receptors and distinct patterns of breast cancer relapse. Breast Cancer Res Treat. 2003; 78:105–118. PMID: 12611463.

23. Bromann PA, Korkaya H, Courtneidge SA. The interplay between Src family kinases and receptor tyrosine kinases. Oncogene. 2004; 23:7957–7968. PMID: 15489913.

Fig. 2
Overall survival (OS) from metastasis according to breast cancer subtypes. Blue line represents OS of hormone receptor (HR)-(+) patients; green line represents OS of human epidermal growth factor receptor 2 (HER2)-(+) patients; red line represents OS of triple negative breast cancer (TNBC) patients.
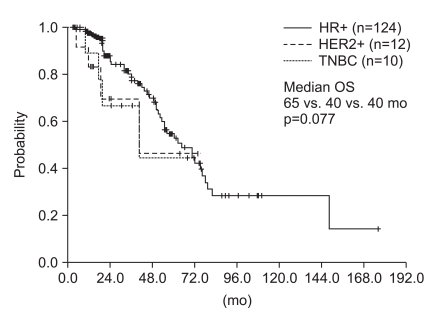
Fig. 3
Progression free survival (PFS) (A) and overall survival (OS) (B) between the patients with single and multiple bone involvement; green line represents survival of patients with single bone metastasis; blue line represents survival of patients with multiple bone metastases.
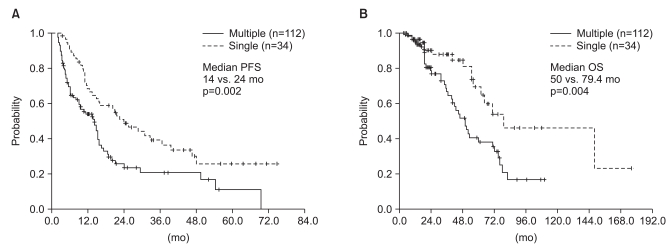
Table 1
Characteristics of 146 bone-only breast cancer patients
Table 2
Comparison of clinicopathologic characteristics according to duration of DRFS for relapsed patients (n=122)
| Characteristics |
DRFS<36 mo (n=60) (%) |
DRFS≥36 mo (n=62) (%) |
p-value |
|---|---|---|---|
| Mean age (±SD) | 46 (±11.7) | 50 (±11.2) | 0.041 (t-test) |
| Initial stage 3 | 30 (50.8) | 26 (42.6) | 0.137 |
| Subtypes (n=121) | 0.156 | ||
| HR+ (ER+ and/or PR+) | 48 (80.0) | 57 (91.9) | |
| HER2+ (ER-/PR-/HER2+) | 6 (10.0) | 2 (3.2) | |
| TNBC (ER-/PR-/HER2-) | 6 (10.0) | 3 (4.9) | |
| Histologic type | |||
| IDC vs. non-IDC | 50 (94.3) | 50 (90.9) | 0.716 |
| Histologic grade (n=82) | |||
| High (Grade 3) | 23 (54.8) | 14 (35.0) | 0.072 |
| Nuclear grade (n=89) | |||
| High (Grade 3) | 22 (50.0) | 12 (26.7) | 0.024 |
| Adjuvant chemotherapy (n=121) | 57 (95.0) | 56 (91.8) | 0.717 |
| Adjuvant endocrine therapy (n=112) | 33 (55.0) | 48 (77.4) | 0.005 |
| Involved bone sites | |||
| Spine | 62.1 | 43.5 | 0.042 |
| Pelvis | 47.4 | 32.3 | 0.092 |
| Sternum | 8.6 | 27.4 | 0.009 |
| Femur | 19.0 | 16.1 | 0.683 |
| Humerus | 5.2 | 0 | 0.110 |
| Rib | 41.4 | 35.5 | 0.507 |
| Skull | 8.8 | 11.5 | 0.764 |
| Clavicle | 3.3 | 3.2 | 0.237 |
| Single bone metastasis | 3 (5.0) | 31 (50.0) | <0.0001 |
| Extensive bone metastasesa) | 15 (25.9) | 10 (16.1) | 0.190 |
| Skeletal eventsb) | 14 (24.1) | 7 (11.3) | 0.064 |
| Progression sites | |||
| Bone | 78.3 | 71.7 | 0.399 |
| Liver | 25.0 | 6.7 | 0.011 |
| Lung | 26.7 | 11.7 | 0.037 |
| Lymph nodes | 11.7 | 8.3 | 0.762 |
| Pleura | 13.3 | 1.7 | 0.032 |
| Brain | 10.0 | 6.7 | 0.743 |
| 1 yr PR-PFSR | 53.8 | 62.5 | 0.362 |
| 5 yr PR-OSR | 50.5 | 72.6 | 0.010 |
DRFS, distant relapse free survival; SD, standard deviation; HR, hormone receptor; ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor 2; TNBC, triple negative breast cancer; IDC, invasive ductal carcinoma; PFSR, progression free survival rate; OSR, overall survival rate. a)Extensive bone metastases,≥10 bones involvement with or without bone destruction soft tissue formation, b)Skeletal events, associated with bone metastases as pain, fracture, and limit of motion.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download