Abstract
Purpose
This study aims to investigate the current situation of national colorectal cancer screening by analyzing participation rates, positive rates of screening methods and screening rate of secondary screening tests in colorectal screening of the national cancer screening program in 2008.
Materials and Methods
With database about target population and screened individuals of the national cancer screening program, the results of target population and participants of colorectal cancer screening in 2008 were analyzed. Among adults aged over 50 years of medical aid and beneficiaries of national health insurance paying lower 50% premiums in the total subscribers, 4,640,365 were target population of colorectal cancer screening and the data of 984,915 undergoing fecal occult blood test (FOBT) as a primary screening were analyzed.
Results
The colorectal cancer screening rate was 21.2% and the rates of national health insurance subscribers, females and the elderly aged 60-64 years were higher than those of others. The recipients with a positive result in FOBT recorded approximately 7.5%. Medical aid beneficiaries (7.9%), males (8.8%) and seniors aged over 75 years (9.1%) showed higher positive rates than the average one. Out of the FOBT positive recipients, 43.0% took a secondary screening and the rate undergoing colonoscopy (31.4%) was higher than that of doing double-contrast barium enema test (11.6%).
Conclusion
Colorectal cancer screening rate of medical aid beneficiaries and people paying lower 50% premiums among national health insurance subscribers, was different according to demographic characters (gender, age and types of health insurance). This finding meant that screening for the vulnerable needed to be encouraged by considering socio-demographic characters. Additionally, more efforts were necessary to increase the secondary screening rate of people with a positive result in primary one.
Go to : 
Colorectal cancer screening is known to contribute to reduction of incidence and mortality of colorectal cancer through detection of precursor lesions of cancer or early stage cancer, and the five-year survival rate of colorectal cancer diagnosed early was reported to around 90% (1,2). In addition, the screening has declined mortality of the cancer. In 12 to 18 years after beginning of cancer screening, the mortality rate of colorectal cancer became lower by 16% (3) and it was found to reduce mortality rate of persons aged 50 to 75 years (4).
In Korea, 2007 Annual Report of Korea Central Cancer Registry showed that the incidence rate of colorectal cancer ranked third in males by recording 49.7 per 100,000 population and the rate recorded the fourth highest level or 33.9 per 100,000 population in females (5). In particular, the incidence rate of colorectal cancer had increased every year and its mortality rate also tended to rise (5,6). Many researches insisted that because colorectal cancer had very long biological natural history as an advanced cancer (7) and long symptom-free interval but it could be treated through early detection, screening and preventive treatment were effective (8,9). For the national cancer screening program to detect and treat cancer early and to decrease mortality of cancer in South Korea, stomach, breast and cervix cancer screening have been conducted for medical aid beneficiaries, whose medical accessibility is weak, since 1999. In 2002 the target population was extended to medical aid beneficiaries and a low-income bracket paying lower 20% premiums among the national health insurance subscribers. In 2003, liver cancer screening was added and the target population became larger by including people paying lower 30% premiums among the total subscribers. In 2004 by adding colorectal cancer screening, the cancer screening program for five major cancer (stomach, liver, colorectal, breast and cervical cancer) was established (10). Since the range of target population was enlarged to medical aid beneficiaries and people paying lower 50% premiums among the people insured by national health insurance, the program has been maintained up to 2008.
The national colorectal cancer screening began in 2004, and males and females aged over 50 years take fecal occult blood test (FOBT) every year and participants with a positive result undergo an additional screening such as colonoscopy and double-contrast barium enema test (DCBE). Although studies on tests for colorectal cancer screening and their meaning and cost-effectiveness have been partially reported, researches on the current situation of the national colorectal cancer screening program are still insufficient. This study examined results of colorectal cancer screening according to demographic characteristics in 2008. In addition, we investigated the process of the colorectal cancer screening and characteristics of screening tests by analyzing participation rates according to test methods.
Go to : 
This study utilized the database of target population and participants of colorectal cancer screening of 2008 national cancer screening program. The target population was adults aged over 50 years among medical aid beneficiaries and national health insurance subscribers. For the subscribers, they or their dependants who paid lower 50% premiums based on those of November, 2007 (monthly 67,800 or less than 67,800 won for employee insured and 56,500 or less than 56,500 won for self-employed insured), were included in this study. When the data about the monthly premiums did not exist, the target population were selected by considering current premiums compared to those on the standard month (11). According to the inclusion criteria, totally 7,522,452 were the total target population of colorectal national cancer screening program and out of them 4,640,365 were the target population of colorectal cancer screening in 2008.
Colorectal cancer is recommended to be screened every year and FOBT was performed as a primary screening test by using fecal immunochemical tests (reversed passive haemagglutination assay [RPHA] or latex agglutination test) or fecal porphyrin quantification. For the participants with a positive result in FOBT, colonoscopy or DCBE test was conducted as a additional screening test. When DCBE result had abnormal findings (polypus, probably cancer, colorectal cancer and other diseases than cancer), colonoscopy was conducted additionally. When colonoscopy found abnormal findings (polypus, suspected colorectal cancer, colorectal cancer and others) biopsy was utilized according to decision of a physician (11). To analyze the current situation of colorectal cancer screening, the participants were defined as persons with at least one among a result of FOBT, a result in colonoscopy, result in DCBE, a result of biopsy or a result of final outcomes in screening record. Out of 985,148 with at least one of them in the record, 984,915 were recruited as participants in 2008 by excluding 111 ones aged less than 50 years, 101 ones thought as persons not screened without personal information and 21 already diagnosed cancer patients. In summary, the target population and the participants of colorectal cancer screening of the colorectal national cancer screening program in 2008 were 4,640,365 and 984,915, respectively.
Demographic characteristics examined in this study were age, types of insurance and region. Age was divided into subgroups by five years with the subjects aged over 50 years and the elderly aged 75 years was analyzed as a subgroup. Types of insurance were classified into medical aid beneficiaries and national health insurance subscribers. Region was divided into 16 cities and or provinces by using the specific number of organizing public health centers.
The results of screening were classified based on contents of the result sheet reported to National Health Insurance Cooperation. In the sheet, final outcomes of colorectal cancer were 'normal', 'need a follow-up', 'need diagnostic work-up for cancer', 'need treatment for cancer' and 'other diseases than cancer'. 'Normal' meant that a result of biopsy, colonoscopy or double-contrast barium enema test was normal or that FOBT showed a negative result. 'Need a follow-up' was written when biopsy revealed inflammatory, hyperplastic or pathologic findings, low/high grade adenoma or dysplasia, when colonoscopy or double-contrast barium enema test found polypus or when FOBT result was positive. 'Need diagnostic work-up for cancer' meant that colorectal cancer was suspected and inspection was needed immediately, and 'need treatment for cancer' showed that colorectal cancer was diagnosed and treatment for it was necessary immediately. 'Other diseases than cancer' was written for other diseases not related with colorectal cancer.
The results of the screening were analyzed with chi square test by demographic variables such as gender, age, type of insurance and region and by screening tests like FOBT, colonoscopy, DCBE and others. FOBT positive rate and participation rates of secondary screening tests were calculated with 95% confidence interval (CI) and all data analysis was conducted with SAS version 9.1 (SAS Inc., Cary, NC, USA).
Go to : 
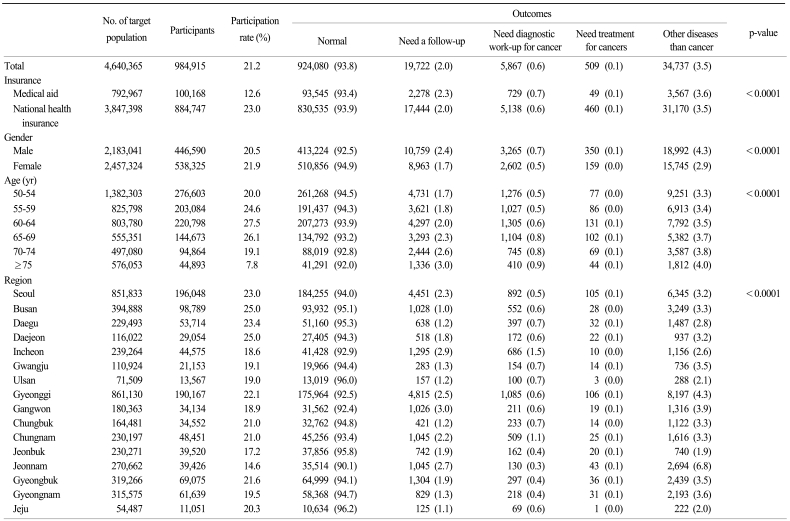
When the current situation of colorectal cancer screening in 2008 was examined, 984,915 out of totally 4,640,365 target population participated in the screening with the participation rate of 21.2% in average (Table 1). The screening rate of national health insurance subscribers was higher than that of medical aid beneficiaries by recording 23.0% and 12.6%, respectively. The rate of females was slightly higher than that of males by recording 21.9% and 20.5%, respectively. For age, the screening rate recorded the highest level or 27.5% in seniors aged 60 to 64 years and the lowest level or 7.8% in those aged over 75 years. For region, while the screening rate was the highest in Busan and Daejeon by recording 25.0%, it was the lowest in Jeonnam by recording 14.6%. When the results of colorectal cancer screening of the participants were investigated, 93.8% (924,080), 2.0% (19,722), 0.6% (5,867) 0.1% (509) and 3.5% (34,737) were found to be normal, need a follow-up, need a work-up for cancer, need treatment for cancer and be other diseases than cancer, respectively.
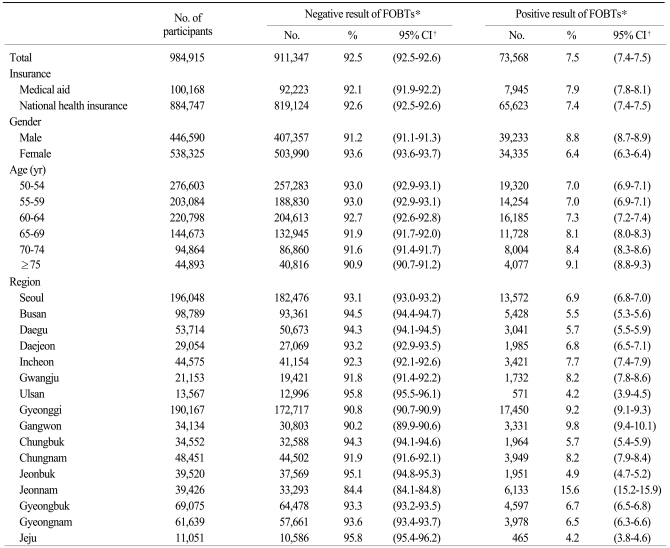
Out of the 984,915 FOBT results, 73,568 (7.5%) and 911,347 (92.5%) showed positive and negative results in FOBT, respectively (Table 2). The positive rate was relatively slightly higher in medical aid beneficiaries than in national health insurance subscribers by recording 7.9% (95% CI, 7.8 to 8.1) and 7.4% (95% CI, 7.4 to 7.5), respectively. The positive rate of males was higher than that of females by recording 8.8% (95% CI, 8.7 to 8.9) and 6.4% (95% CI, 6.3 to 6.4), respectively. The positive rate of the elderly aged over 75 years showed the highest level or 9.1% (95% CI, 8.8 to 9.3) and for region the rate of Jeonnam was the highest by recording 15.6% (95% CI, 15.2 to 15.9).
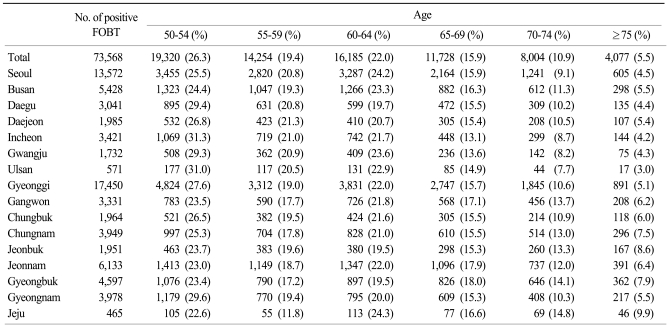
When 73,568 participants with a positive result in FOBT were analyzed according to age and region, adults aged 50 to 54 years accounted for the largest part or 26.3% while adults aged over 75 years did for the smallest part or 5.5% (Table 3). For region, among adults aged 50 to 54 those in Ulsan had the largest portion or 31.0% and those in Jeju captured the smallest portion or 22.6%. On the contrary, among adults aged over 75 years those in Jeju and Ulsan accounted for the largest (9.9%) and the smallest portions (3.0%), respectively.
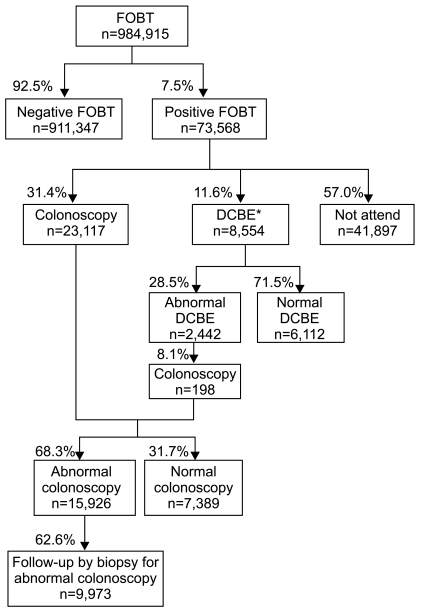
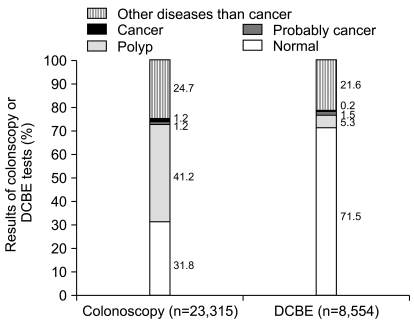
The national cancer screening program provided colonoscopy or DCBE as a secondary screening test for participants with a positive result in FOBT. Out of 73,568 showing the positive result in FOBT, 31,671 underwent a secondary screening test and the participation rate was 43.0% (95% CI, 42.7 to 43.4) (Fig. 1). As 23,117 and 8,554 underwent colonoscopy and DCBE as a secondary screening test with the participation rate of 31.4% (95% CI, 31.3 to 31.6) and 11.6% (95% CI, 11.4 to 11.9), respectively, the colonoscopy rate was higher than that of DCBE. The national cancer screening program recommended that persons with abnormal finding in DCBE took colonoscopy additionally. Among 2,422 with abnormal findings in DCBE 198 (participation rate 8.1%; 95% CI, 7.0 to 9.2) underwent colonoscopy. In a narrowed analysis, it was 143 who had 'probably cancer' or 'colorectal cancer' among 198 DCBE abnormal people, and 24 took colonoscopy (participation rate 16.8%; 95% CI, 10.7 to 22.9) out of 143 (data not shown). The program recommended that persons with abnormal findings in colonoscopy to have biopsy, and 9,973 out of 15,926 with abnormal findings in colonoscopy underwent biopsy (participation rate 62.6%; 95% CI, 61.9 to 63.4). Among 558 observed to have 'probably cancer' or 'colorectal cancer', 500 took biopsy (participation rate 89.6%; 95% CI, 87.1 to 92.1) (data not shown).
Results of colonoscopy and DCBE were compared by designating the participants showing a positive result in FOBT and undergoing each of the two tests as 100 (Fig. 2). 'Normal' accounted for 31.8% and 71.5% in the results of colonoscopy and DCBE, respectively, so the latter fraction was two times higher than that in the former one. The fractions of 'Polyp' were 41.2% and 5.3% in the results of colonoscopy and DCBE, respectively, and those of 'probably cancer' were 1.2% and 1.5% in the results of colonoscopy and DCBE, respectively. 'Colorectal cancer' was observed in 1.2% and 0.2% of the participants undergoing colonoscopy and DCBE, respectively, and the fraction of the former test was higher than that of the latter test.
Go to : 
The target population of colorectal cancer screening in national cancer screening program in 2008 was totally 4,640,365 and their participation rate was averagely 21.2%. FOBT positive rate out of the participants was approximately 7.9% and males, the elderly aged over 75 years and medical aid beneficiaries recorded relatively higher positive rates compared to females, other age groups and people insured health insurance, respectively. For secondary screening rate of the participants with a positive result in FOBT, the rate of colonoscopy was higher than that of DCBE.
That FOBT was conducted as a primary screening test of colorectal cancer in the national cancer screening program in Korea, which is similar with the national colorectal cancer screening program in England, Japan and Finland operating (8), and persons showing a positive result in FOBT underwent colonoscopy and DCBE (12-14). Colorectal cancer screening program has been operated since 2004 and we have been reporting our program results in a monograph every year. Target population of colorectal cancer screening tended to increase from 2.26 million in 2004 to 3.27 million in 2005, 4.40 million in 2006 and 4.34 million in 2007 (15). The target population of a current colorectal cancer screening conducted in 2008 was about 4.60 million and out of them 0.98 million participated in the screening by recording the rate or 21.2%. The level was slightly lower than 25.7% or 1.73 million out of 6.73 million target population of colorectal cancer screening shown by a report (16) of National Health Insurance Cooperation in 2008 investigating the total beneficiaries of national health insurance. In addition, even though a direct comparison is hard to be performed, the participation rate of FOBT or colonoscopy within 10 years was 50 to 60% in the U.S. in 2006 and the participation rate of FOBT every two years or of colonoscopy within five years recorded 28 to 53% in Canada in 2008 (14). So South Korea needs more efforts to encourage the colorectal cancer screening rate in the national cancer screening program. In comparison of participation rates according to demographic characteristics, the rates were even by gender and age but the rate of seniors aged over 75 years reduced sharply. As the screening rate of national health insurance subscribers was two times higher than that of medical aid beneficiaries, this finding suggested that types of insurance could mean economic differences and socio-economic differences could lead to differences in screening rates. However, because various factors such as comorbidity, accessibility of medical institutions for screening, educational background and recognition on diseases were not considered, a direct interpretation on correlation between economic levels and screening rates had some limitations in this study. In the meantime, the results of colorectal cancer screening showed that medical aid beneficiaries and older recipients recorded higher rates of additional tests, so the screening of the vulnerable needed to be encouraged.
Among the participants of a primary colorectal cancer screening, FOBT positive rate was about 7.5%. As this study did not include national health insurance subscribers paying higher 50% premiums and private health examination, it could not represent the total people in South Korea. Despite these limitations, the positive rate was compared with the results of national cancer screening in foreign countries to determine the level of South Korea roughly. In the screening of Japan conducted with about 4.00 million adults aged over 40 years in 1995, the FOBT positive rate was 7.3% (7). The pilot study of England reported in 2004 (13) showed that the colorectal cancer screening rate was approximately 59.2% but the FOBT positive rate was about 1.6%. As other studies in Korea, a randomized clinical trial in Gumi found that the FOBT positive rate of the general public was around 1.0 to 2.4% (7), and it was said that the positive rate of persons visiting health examination centers of hospitals from January, 2004 to April, 2005 was around 1.8% (17). The difference in FOBT positive rates of the national screening program and community-based studies was thought to be caused by considering that the national screening program was conducted by hospitals and clinics around the nation. In this study, the regional distribution of FOBT positive rate showed relatively higher deviation from 4.2 to 15.6% and the rate of Jeonnam was outstandingly high. When the rates were stratified according to region and age, the positive rate of Jeonnam was higher than that of other regions but there was no significant increase by age and no specific correlation according to region and age in the distribution of positive rates. Therefore, the deviation was considered to be caused by properties of health examination institutions. However, it is the third year of the quality control the National Cancer Screening Program including FOBT tests by the Ministry of Health and Welfare, National Cancer Center of Korea and with academic societies. We expect that the discrepancy of quality of the FOBT tests between institutions may diminish and the quality overall to be increased afterward. For gender, males recorded 1.4 times higher positive rate or 8.8% than females and for age the elderly aged over 65 years showed a high positive rate by recording 8.1 to 9.1%. Although this study could not determine correlation between older age and higher positive rate of FOBT and between older age and higher incidence rate and mortality rate of colorectal cancer, it showed at least that the tendency of higher FOBT positive rate at older age was same with the tendency of incidence of colorectal cancer by age in South Korea (5,6).
The participants with a positive result in FOBT were recommended to undergo colonoscopy or DCBE and the participation rate of colonoscopy was about 2.7 times higher than that of DCBE by recording 31.4% and 11.6%, respectively. Additional analysis on difference in participation rates of the two secondary tests by gender, age, region and types of insurance was performed although its results were not presented as results. According to the analysis, colonoscopy rate was higher in males (32.1%) and national health insurance subscribers (32.2%) than the average rate or 31.4% but DCBE rate was higher in females (12.0%) and medical aid beneficiaries (13.1%) than the average rate or 11.6%. In addition, colonoscopy rate was decreased at older age by recording 17.2 to 37.1% and DCBE rate did not show a tendency according to age by recording 10.5 to 12.9%. For region, colonoscopy rate was higher in 14 regions except two ones (Gwangju and Gangwon) and its deviation was 19.2 to 54.7%. These results suggested that gender, types of insurance and age affected preference to or recognition on more invasive colonoscopy needing longer examination time. The difference in participation rates of secondary screening tests by region was observed and it was considered to be caused by the difference in the real condition of medical institutions and medical circumstances. Future studies were necessary to determine that clearly.
According to a study assuming MarKov model in terms of cost-effectiveness of colorectal cancer screening tests (18), as a colonoscopy screening was effective in reducing mortality rate compared to others and showed a high cost-effectiveness. A research performed in South Korea also insisted that colonoscopy was cost-effective (9). As a secondary test was recommended based on these results, the participation rate of colonoscopy was considered to be high. In addition, persons with abnormal findings in DCBE were recommended to undergo colonoscopy in the screening process, so the participation rate of colonoscopy was higher. Colonoscopy rate out of persons with abnormal findings in DCBE and biopsy rate out of persons with abnormal findings in colonoscopy recorded 8.1% and 62.6%, respectively, and the rates of persons found to have 'probably cancer' or 'colorectal cancer' were higher than the former ones by recording 16.8% and 89.6%, respectively. Like this, as abnormal findings included 'polypus', 'probably cancer', 'colorectal cancer' and 'other diseases than cancer', high rates of 'polyps' and 'other diseases than cancer' were considered to provoke reduced participation rate of secondary tests in total participants with abnormal findings. In particular, the rate of persons showing a positive result in FOBT but not taking secondary test recorded a high level or 57.0%. That was considered to be because this study analyzed only the data of the national cancer screening program, and if cases undergoing secondary tests through private health examination or private medical sector were included the secondary screening rate was expected to become higher. Moreover, even though persons were recommended to undergo a secondary screening test, low recognition on colonoscopy or DCBE and inconvenience of taking it were thought to increase the rate of not attending secondary screening. This study found that the secondary colorectal cancer screening rate was low although the national program provided free secondary test for persons with a positive result in FOBT and that needed to be dealt with properly.
Among persons with a positive result in FOBT, those observed to have cancer in secondary tests such as colonoscopy and DCBE accounted for approximately 1.2% and 0.2%, respectively, and those done to have 'probably cancer' were 1.2% and 1.5%, respectively. Considering that FOBT positive rate showed a large deviation by region and its average was higher than those in previous studies, the result suggested that more efforts to improve the sensitivity of FOBT were necessary. Foreign studies also reported that the sensitivity of FOBT was lower by recording 30 to 50% (8). In future, it is needed to supplement FOBT and to enhance policies to increase the effect of the national colorectal screening based on cost-effectiveness studies using national data on colonoscopy and DCBE as secondary screening tests.
Go to : 
This study was conducted to investigate the results of the national cancer screening program and to assess outcomes of colorectal cancer screening by analyzing the colorectal cancer screening in the national cancer screening program in 2008. In future, more efforts to increase the colorectal cancer screening rate need to be continued and specialized advertisement strategies according to age, gender and region are also necessary. Also, a faithful participation such as higher participation rates of secondary tests should be guided and high-quality screening should be provided in all health examination institutions through quality control or education.
Go to : 
References
1. Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008; 134:1570–1595. PMID: 18384785.

2. Smith RA, von Eschenbach AC, Wender R, Levin B, Byers T, Rothenberger D, et al. American Cancer Society guidelines for the early detection of cancer: update of early detection guidelines for prostate, colorectal, and endometrial cancers. Also: update 2001--testing for early lung cancer detection. CA Cancer J Clin. 2001; 51:38–75. PMID: 11577479.

3. Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008; 149:638–658. PMID: 18838718.

4. U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008; 149:627–637. PMID: 18838716.
5. Ministry of Health and Welfare. Annual report of the Korea Central Cancer Registry. 2007. Seoul: Ministry of Health and Welfare.
6. Korea National Statistical Office. Annual report of the cause of death statistics. 2007. Daejeon: Korea National Statistical Office.
7. Lee BH, Jeong SY. Korean national recommendation guidelines on screening and surveillance for early detection of colorectal cancers. J Korean Med Assoc. 2002; 45:981–991.

8. Han DS, Park JY, Yun HR, Bae SC. Cost-effectiveness analysis of colon cancer screening by colonosopic examination in Korea. Korean J Gastrointest Endosc. 2004; 28:1–8.
9. Park SM, Chang YJ, Yun YH, Yoo TW, Huh BY, Kwon S. Cost-effectiveness analysis of colorectal cancer screening in Korean general population. J Korean Acad Fam Med. 2004; 25:297–306.
10. Choi KS, Park EC, Shin HR, Kim CM, Oh DK. National cancer screening program in Korea. J Korean Assoc Cancer Prev. 2004; 9:116–122.
11. Ministry of Health and Welfare. National cancer screening programes guideline. 2008. Seoul: Ministry of Health and Welfare.
12. Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2008: a review of current American Cancer Society guidelines and cancer screening issues. CA Cancer J Clin. 2008; 58:161–179. PMID: 18443206.

13. UK Colorectal Cancer Screening Pilot Group. Results of the first round of a demonstration pilot of screening for colorectal cancer in the United Kingdom. BMJ. 2004; 329:133. PMID: 15237087.
14. Wilkins K, Shields M. Colorectal cancer testing in Canada--2008. Health Rep. 2009; 20:21–30. PMID: 19813436.
15. National Cancer Center. Support and evaluation of national cancer control program. 2010. Goyang: National Cancer Center.
16. National Health Insurance Corporation. National health screening statistical yearbook. 2008. Seoul: National Health Insurance Corporation.
17. Kwon JH, Choi MG, Suh JP, Chang JH, Nam KW, Park HS, et al. The significance of fecal occult blood testing to screen for colon cancer. Korean J Gastrointest Endosc. 2007; 35:68–73.
18. Sonnenberg A, Delcò F, Inadomi JM. Cost-effectiveness of colonoscopy in screening for colorectal cancer. Ann Intern Med. 2000; 133:573–584. PMID: 11033584.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download