Abstract
Patients with reduced dihydropyrimidine dehydrogenase (DPD) activity are at risk for experiencing serious adverse effects following 5-fluorouracil (5-FU) based chemotherapy. Neurotoxicity is considered an extremely rare side effect of 5-FU. We report here on an unusual case of 5-FU induced encephalopathy. A 38-year-old woman with advanced gastric carcinoma was treated with adjuvant chemotherapy that consisted of infused 5-FU (1,000 mg/m2) for 5 days and cisplatin (60 mg/m2) on day 1 following total gastrectomy. Nineteen days after starting chemotherapy, the patient displayed a sudden onset of slurred speech, confusion, cognitive disturbances and paranoia. A magnetic resonance image (MRI) of the brain showed no structural abnormalities, and the other laboratory tests provided no explanations for her symptoms, other than a slightly elevated ammonia level. The patient was treated with a lactulose retention enema and thiamine infusion, the 5-FU was halted and her symptoms then recovered after 7 days.
Go to : 
5-FU is an anti-metabolite and anti-neoplastic agent that has been used to treat a variety of cancers such as carcinoma of the breast, pancreas, colon, rectum and stomach (1). 5-FU is metabolized inside the cells to 5-fluoro-2-deoxyuridine-5-phosphate, and this metabolite inhibits thymidylate synthase. The common side effects of 5-FU are related to its effects on the bone marrow and the gastrointestinal epithelium. The symptoms include bone marrow suppression and such gastrointestinal toxicities as nausea, vomiting, diarrhea and stomatitis. Although 5-FU induced neurotoxicity is rare, the administration of 5-FU can cause both acute and delayed neurotoxicity.
We report here on a patient who developed acute neurotoxicity and hyperammonemia after systemic chemotherapy with a continuous infusion of 5-FU and cisplatin.
Go to : 
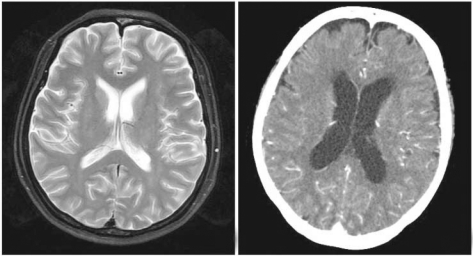
A 38-year-old female underwent curative radical total gastrectomy for her stage IIIB (T3N2M0) advanced gastric cancer followed by adjuvant chemotherapy that consisted of 5-FU (1,000 mg/m2, i.v. on days 1 to 5) and cisplatin (60 mg/m2, i.v. on day 1) in 3 week cycles. The patient complained of severe emesis during chemotherapy. Fourteen days after completion of her first cycle of chemotherapy, she visited the hospital because of her weakness, anorexia, oral mucositis and diarrhea. Her blood pressure was 100/60 mmHg, the respiratory rate was 20/min, the heart rate was 94 beats/min and her body temperature was 36.4℃. The patient appeared to be acutely ill with a poor nutritional status. The laboratory inves-tigations showed the following: a WBC of 2,390/µL (ANC 1061/µL), a Hb level of 10.8 g/dL, a platelet count of 26,000/µL, a BUN/Cr levels of 18/1.0 mg/dL and Na/K/Cl levels of 124/3.1/82 mmol/L. Four days after admission, the patient's mental status deteriorated, and she showed symptoms that included slurred speech, inappro-priate language and insomnia. The neurologic examination revealed a confused mental status, paranoid behavior, lethargy, slurred speech and somnolence. A magnetic resonance image of the brain showed no structural abnormalities (Fig. 1). Her ammonia level was elevated to 58 µmol/L (normal range: l~47 µmol/L), and the other labo-ratory tests provided no explanation for her symptoms. The patient was treated with a lactulose retention enema and thiamine infusion. The patient's symptoms, including the neuropsychiatric problems, neutropenia and thrombocytopenia, were recovered in a week. After this event, her regimen was changed to docetaxel with cisplatin, and she completed adjuvant chemotherapy. Up to now, she has recovered after treatment with no recurrence of tumor.
Go to : 
5-FU was first synthesized in 1957, and it is currently one of the most widely used anti-cancer, anti-metabolic agents as it shows activity against a broad range of solid tumors, including gastrointestinal, breast and head and neck cancer. The spectrum of 5-FU's toxicities is both dose and schedule-dependent (1). The main effects of this drug are on rapidly dividing tissues, and specifically the gastrointestinal mucosa and bone marrow. Myelosuppression is schedule-dependent, and this is more common when administering 5-FU as a bolus. The gastrointestinal tract toxicity is characterized by manifestations of epithelial ulceration such as mucositis, esophagitis, gastritis and colitis with diarrhea. Nausea and vomiting may also occur, but these symptoms are usually well controlled with antiemetics. The other toxicities associated with 5-FU therapy include dermatologic toxicities such as alopecia and fingernail changes, a pruritic erythematous rash, ocular toxicity and uncommonly, cardiotoxicity. Neurotoxicity is one of the rare adverse effects associated with 5-FU treatment. The acute and delayed forms of 5-FU related neurotoxicity have been reported (2). The acute form consists of cerebellar syndrome that's characterized by an acute onset and reversibility upon drug discontinuation, as well as encephalopathy, whereas the delayed variety takes the form of subacute multifocal leukoencephalopathy.
Although some theories have been proposed, the mechanisms for the neurotoxicity of 5-FU are poorly understood. Some researchers believe that accumulated fluoroacetate, which is a product of 5-FU catabolism that inhibits the Krebs cycle enzyme, leads to impairment of the urea cycle (3). According to this theory, ammonia, which is a product of 5-FU metabolism, accumulates in large amounts after the administration of high dose 5-FU. Therefore, encephalopathy subsequently occurs and this is accompanied by hyperammonemia and lactic acidosis. Kim et al. have reported on a case for which an intermediate dose of 5-FU induced encephalopathy (4). Using real-time PCR, the patient's mRNA level of DPD enzyme was checked before and after treatment and this was compared with those levels of a control group of 16 patients who were treated with the same regimen. The results showed that the patient's pre-treatment level of DPD was in the control range, but its level was elevated up to 187% after 5-FU treatment. According to their results, the authors suggested that the transient stagnation of 5-FU's catabolites would play an important role in the development of neurotoxicity. Another theory to explain the neurologic adverse effect by 5-FU therapy is that this drug brings about a deficiency of thiamine. Thiamine pyrophosphate (TPP) is the active form of the vitamin. Exposure to 5-FU can increase the TPP level. These results indicate that 5-FU may increase the cellular thiamine metabolism, and this can possibly exacerbate thiamine deficiency (5). This theory is supported by the fact that the symptoms of the Wernicke-Korsakoff syndrome, including ataxia, nystagmus, mental confusion and cognitive changes, are similar to the neurotoxic effects of fluorouracil.
Dehydropyrimidine dehydrogenase (DPD) is a breakdown enzyme of 5-FU, and DPD is distributed in the liver, gastrointestinal mucosa and peripheral lymphocytes. More than 80% of the administered 5-FU is catabolized by DPD (6). Thus, a deficiency of this enzyme can cause life-threatening or fatal toxicity when a patient is treated with fluoropurimidine-based chemotherapy (2). The incidence of DPD deficiency in cancer patients has been estimated to be 2.7%, and this malady can be accompanied by severe fluorouracil toxicity (7).
The diagnosis of 5-FU related encephalopathy is one of exclusion: (1) the development of encephalopathy during or shortly after the completion of 5-FU administration, (2) exclusion of other metabolic factors that may affect a patient's consciousness and mental functioning, such as hypoglycemia, organ failure, electrolyte imbalance, sepsis and central nervous system involvement by cancer, and (3) exclusion of an adverse effect by concomitant medications (8).
The patient in this current study experienced a sudden onset of neurological symptoms 18 days after the first chemotherapy treatment. She complained at admission of persistent nausea and anorexia and a poor oral intake; however, she was not in a chronic state of malnutrition. The laboratory findings showed electrolyte imbalance with hyponatremia, neutropenia and thrombocytopenia, yet this problem was corrected with appropriate fluid therapy. Most of the 5-FU-associated neurotoxicities developed during 5-FU infusion, or shortly after completion of the 5-FU infusion. However, some previous studies have reported on symptoms that were expressed within a few days to five weeks after treatment (9), so that we can speculate on the notion that her symptoms could have been caused by chemotherapy-related side effects. She displayed severe bone marrow suppression, mucositis, nausea and vomiting, as well as neurotoxicity. The serum ammonia level was slightly elevated. Although we were not able to check the level of decreased DPD activity, we indirectly suspected she had a DPD enzyme deficiency according to her clinical symptoms. We thought that the cause of the neurotoxicity in this patient was the reduced level of DPD enzyme, and we stopped using the previous regimen, including the 5-FU, and we started conservative treatment for the encephalopathy such as fluid supplementation, a lactulose enema and intravenous thiamine supplementation (4,10). Her symptoms then recovered in a week.
Some reports on DPD deficiency confirmed this condition by performing DPD enzyme assay with using peripheral blood mononuclear cells (7,11), or by assessing the low mRNA levels of DPD enzyme, as estimated by real-time quantitative PCR (12). However, DPD deficiency has a low incidence, and if it is suspected, then a quick break in the medication, along with conservative treatment, can result in a recovery from symptoms.
In conclusion, physicians should take notice of the neurological symptoms of cancer patients who are being treated with 5-FU-based chemotherapy.
Go to : 
References
1. Grem JL. 5-Fluorouracil: forty-plus and still ticking. A review of its preclinical and clinical development. Invest New Drugs. 2000; 18:299–313. PMID: 11081567.
2. Pirzada NA, Ali II, Dafer RM. Fluorouracil-induced neurotoxicity. Ann Pharmacother. 2000; 34:35–38. PMID: 10669184.

3. Koenig H, Patel A. Biochemical basis for fluorouracil neurotoxicity. The role of Krebs cycle inhibition by fluoroacetate. Arch Neurol. 1970; 23:155–160. PMID: 5430334.
4. Kim YA, Chung HC, Choi HJ, Rha SY, Seong JS, Jeung HC. Intermediate dose 5-fluorouracil-induced encephalopathy. Jpn J Clin Oncol. 2006; 36:55–59. PMID: 16436463.

5. Heier MS, Dornish JM. Effect of the fluoropyrimidines 5-fluorouracil and doxifluridine on cellular uptake of thiamin. Anticancer Res. 1989; 9:1073–1077. PMID: 2530931.
6. Heggie GD, Sommadossi JP, Cross DS, Huster WJ, Diasio RB. Clinical pharmacokinetics of 5-fluorouracil and its metabolites in plasma, urine, and bile. Cancer Res. 1987; 47:2203–2206. PMID: 3829006.
7. Etienne MC, Lagrange JL, Dassonville O, Fleming R, Thyss A, Renee N, et al. Population study of dihydropyrimidine dehydrogenase in cancer patients. J Clin Oncol. 1994; 12:2248–2253. PMID: 7964939.

8. Yeh KH, Cheng AL. High-dose 5-fluorouracil infusional therapy is associated with hyperammonaemia, lactic acidosis and encephalopathy. Br J Cancer. 1997; 75:464–465. PMID: 9020500.

9. Cho IJ, Chang HJ, Lee KE, Won HS, Choi MY, Nam EM, et al. A case of Wernicke's encephalopathy following fluorouracil-based chemotherapy. J Korean Med Sci. 2009; 24:747–750. PMID: 19654964.

10. Cheung WY, Fralick RA, Cheng S. The confused cancer patient: a case of 5-fluorouracil-induced encephalopathy. Curr Oncol. 2008; 15:234–236. PMID: 19008998.

11. Takimoto CH, Lu ZH, Zhang R, Liang MD, Larson LV, Cantilena LR Jr, et al. Severe neurotoxicity following 5-fluorouracil-based chemotherapy in a patient with dihydropyrimidine dehydrogenase deficiency. Clin Cancer Res. 1996; 2:477–481. PMID: 9816193.
12. Baek JH, Kim JG, Kim SN, Kim DH, Sohn SK, Hong YJ, et al. Unpredicted severe toxicity after 5-fluorouracil treatment due to dihydropyrimidine dehydrogenase deficiency. Korean J Intern Med. 2006; 21:43–45. PMID: 16646564.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download