1. Cooperberg MR, Broering JM, Litwin MS, Lubeck DP, Mehta SS, Henning JM, et al. The contemporary management of prostate cancer in the United States: lessons from the cancer of the prostate strategic urologic research endeavor (CapSURE), a national disease registry. J Urol. 2004; 171:1393–1401. PMID:
15017184.

2. Cooperberg MR, Broering JM, Kantoff PW, Carroll PR. Contemporary trends in low risk prostate cancer: risk assessment and treatment. J Urol. 2007; 178:S14–S19. PMID:
17644125.

3. Oesterling JE, Chan DW, Epstein JI, Kimball AW Jr, Bruzek DJ, Rock RC, et al. Prostate specific antigen in the preoperative and postoperative evaluation of localized prostatic cancer treated with radical prostatectomy. J Urol. 1988; 139:766–772. PMID:
2451037.

4. Partin AW, Oesterling JE. The clinical usefulness of prostate specific antigen: update 1994. J Urol. 1994; 152:1358–1368. PMID:
7523702.

5. Presti JC Jr, Shinohara K, Bacchetti P, Tigrani V, Bhargava V. Positive fraction of systematic biopsies predicts risk of relapse after radical prostatectomy. Urology. 1998; 52:1079–1084. PMID:
9836558.

6. Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC. Natural history of progression after PSA elevation following radical prostatectomy. JAMA. 1999; 281:1591–1597. PMID:
10235151.

7. Freedland SJ, Wieder JA, Jack GS, Dorey F, deKernion JB, Aronson WJ. Improved risk stratification for biochemical recurrence after radical prostatectomy using a novel risk group system based on prostate specific antigen density and biopsy Gleason score. J Urol. 2002; 168:110–115. PMID:
12050502.

8. Moul JW, Connelly RR, Lubeck DP, Bauer JJ, Sun L, Flanders SC, et al. Predicting risk of prostate specific antigen recurrence after radical prostatectomy with the Center for Prostate Disease Research and Cancer of the Prostate Strategic Urologic Research Endeavor databases. J Urol. 2001; 166:1322–1327. PMID:
11547066.

9. Hull GW, Rabbani F, Abbas F, Wheeler TM, Kattan MW, Scardino PT. Cancer control with radical prostatectomy alone in 1,000 consecutive patients. J Urol. 2002; 167:528–534. PMID:
11792912.

10. Amling CL, Bergstralh EJ, Blute ML, Slezak JM, Zincke H. Defining prostate specific antigen progression after radical prostatectomy: what is the most appropriate cut point? J Urol. 2001; 165:1146–1151. PMID:
11257657.

11. Iselin CE, Robertson JE, Paulson DF. Radical perineal prostatectomy: oncological outcome during a 20-year period. J Urol. 1999; 161:163–168. PMID:
10037390.

12. Freedland SJ, Sutter ME, Dorey F, Aronson WJ. Defining the ideal cutpoint for determining PSA recurrence after radical prostatectomy. Prostate-specific antigen. Urology. 2003; 61:365–369. PMID:
12597949.
13. Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D'Amico AV, Dmochowski RR, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol. 2007; 177:540–545. PMID:
17222629.

14. Heidenreich A, Aus G, Bolla M, Joniau S, Matveev VB, Schmid HP, et al. EAU guidelines on prostate cancer. Eur Urol. 2008; 53:68–80. PMID:
17920184.

15. Boccon-Gibod L, Djavan WB, Hammerer P, Hoeltl W, Kattan MW, Prayer-Galetti T, et al. Management of prostate-specific antigen relapse in prostate cancer: a European Consensus. Int J Clin Pract. 2004; 58:382–390. PMID:
15161124.

16. Stephenson AJ, Kattan MW, Eastham JA, Dotan ZA, Bianco FJ Jr, Lilja H, et al. Defining biochemical recurrence of prostate cancer after radical prostatectomy: a proposal for a standardized definition. J Clin Oncol. 2006; 24:3973–3978. PMID:
16921049.

17. Scher HI, Eisenberger M, D'Amico AV, Halabi S, Small EJ, Morris M, et al. Eligibility and outcomes reporting guidelines for clinical trials for patients in the state of a rising prostate-specific antigen: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol. 2004; 22:537–556. [Erratum appears in J Clin Oncol. 2004;22:3205]. PMID:
14752077.

18. Ellis WJ, Vessella RL, Noteboom JL, Lange PH, Wolfert RL, Rittenhouse HG. Early detection of recurrent prostate cancer with an ultrasensitive chemiluminescent prostate-specific antigen assay. Urology. 1997; 50:573–579. PMID:
9338734.

19. Doherty AP, Bower M, Smith GL, Miano R, Mannion EM, Mitchell H, et al. Undetectable ultrasensitive PSA after radical prostatectomy for prostate cancer predicts relapse-free survival. Br J Cancer. 2000; 83:1432–1436. PMID:
11076649.

20. Ornstein DK, Oh J, Herschman JD, Andriole GL. Evaluation and management of the man who has failed primary curative therapy for prostate cancer. Urol Clin North Am. 1998; 25:591–601. PMID:
10026768.

21. Diamandis EP, Yu H. Nonprostatic sources of prostate-specific antigen. Urol Clin North Am. 1997; 24:275–282. PMID:
9126224.

22. Karakiewicz PI, Eastham JA, Graefen M, Cagiannos I, Stricker PD, Klein E, et al. Prognostic impact of positive surgical margins in surgically treated prostate cancer: multi-institutional assessment of 5,831 patients. Urology. 2005; 66:1245–1250. PMID:
16360451.

23. Khan MA, Partin AW, Mangold LA, Epstein JI, Walsh PC. Probability of biochemical recurrence by analysis of pathologic stage, Gleason score, and margin status for localized prostate cancer. Urology. 2003; 62:866–871. PMID:
14624910.

24. Thompson IM, Tangen CM, Paradelo J, Lucia MS, Miller G, Troyer D, et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J Urol. 2009; 181:956–962. PMID:
19167731.

25. Swanson GP, Hussey MA, Tangen CM, Chin J, Messing E, Canby-Hagino E, et al. Predominant treatment failure in postprostatectomy patients is local: analysis of patterns of treatment failure in SWOG 8794. J Clin Oncol. 2007; 25:2225–2229. PMID:
17538167.

26. Bolla M, van Poppel H, Collette L, van Cangh P, Vekemans K, Da Pozzo L, et al. Postoperative radiotherapy after radical prostatectomy: a randomised controlled trial (EORTC trial 22911). Lancet. 2005; 366:572–578. PMID:
16099293.

27. Wiegel T, Bottke D, Steiner U, Siegmann A, Golz R, Storkel S, et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96-02/AUO AP 09/95. J Clin Oncol. 2009; 27:2924–2930. PMID:
19433689.
28. Cher ML, Bianco FJ Jr, Lam JS, Davis LP, Grignon DJ, Sakr WA, et al. Limited role of radionuclide bone scintigraphy in patients with prostate specific antigen elevations after radical prostatectomy. J Urol. 1998; 160:1387–1391. PMID:
9751361.

29. Dotan ZA, Bianco FJ Jr, Rabbani F, Eastham JA, Fearn P, Scher HI, et al. Pattern of prostate-specific antigen (PSA) failure dictates the probability of a positive bone scan in patients with an increasing PSA after radical prostatectomy. J Clin Oncol. 2005; 23:1962–1968. PMID:
15774789.

30. Gomez P, Manoharan M, Kim SS, Soloway MS. Radionuclide bone scintigraphy in patients with biochemical recurrence after radical prostatectomy: when is it indicated? BJU Int. 2004; 94:299–302. PMID:
15291855.

31. Okotie OT, Aronson WJ, Wieder JA, Liao Y, Dorey F, DeKernion JB, et al. Predictors of metastatic disease in men with biochemical failure following radical prostatectomy. J Urol. 2004; 171:2260–2264. PMID:
15126798.

32. Kane CJ, Amling CL, Johnstone PA, Pak N, Lance RS, Thrasher JB, et al. Limited value of bone scintigraphy and computed tomography in assessing biochemical failure after radical prostatectomy. Urology. 2003; 61:607–611. PMID:
12639656.

33. Saleem MD, Sanders H, Abu El Naser M, El-Galley R. Factors predicting cancer detection in biopsy of the prostatic fossa after radical prostatectomy. Urology. 1998; 51:283–286. PMID:
9495712.

34. Connolly JA, Shinohara K, Presti JC Jr, Carroll PR. Local recurrence after radical prostatectomy: characteristics in size, location, and relationship to prostate-specific antigen and surgical margins. Urology. 1996; 47:225–231. PMID:
8607239.

35. Shekarriz B, Upadhyay J, Wood DP Jr, Hinman J, Raasch J, Cummings GD, et al. Vesicourethral anastomosis biopsy after radical prostatectomy: predictive value of prostate-specific antigen and pathologic stage. Urology. 1999; 54:1044–1048. PMID:
10604706.

36. Scattoni V, Montorsi F, Picchio M, Roscigno M, Salonia A, Rigatti P, et al. Diagnosis of local recurrence after radical prostatectomy. BJU Int. 2004; 93:680–688. PMID:
15009088.

37. Naya Y, Okihara K, Evans RB, Babaian RJ. Efficacy of prostatic fossa biopsy in detecting local recurrence after radical prostatectomy. Urology. 2005; 66:350–355. PMID:
16040095.

38. Deliveliotis C, Manousakas T, Chrisofos M, Skolarikos A, Delis A, Dimopoulos C. Diagnostic efficacy of transrectal ultrasound-guided biopsy of the prostatic fossa in patients with rising PSA following radical prostatectomy. World J Urol. 2007; 25:309–313. PMID:
17440730.

39. Koppie TM, Grossfeld GD, Nudell DM, Weinberg VK, Carroll PR. Is anastomotic biopsy necessary before radiotherapy after radical prostatectomy? J Urol. 2001; 166:111–115. PMID:
11435834.

40. Sella T, Schwartz LH, Swindle PW, Onyebuchi CN, Scardino PT, Scher HI, et al. Suspected local recurrence after radical prostatectomy: endorectal coil MR imaging. Radiology. 2004; 231:379–385. PMID:
15064390.

41. Miralbell R, Vees H, Lozano J, Khan H, Molla M, Hidalgo A, et al. Endorectal MRI assessment of local relapse after surgery for prostate cancer: a model to define treatment field guidelines for adjuvant radiotherapy in patients at high risk for local failure. Int J Radiat Oncol Biol Phys. 2007; 67:356–361. PMID:
17236961.

42. Sciarra A, Panebianco V, Salciccia S, Osimani M, Lisi D, Ciccariello M, et al. Role of dynamic contrast-enhanced magnetic resonance (MR) imaging and proton MR spectroscopic imaging in the detection of local recurrence after radical prostatectomy for prostate cancer. Eur Urol. 2008; 54:589–600. PMID:
18226441.

43. Hinkle GH, Burgers JK, Neal CE, Texter JH, Kahn D, Williams RD, et al. Multicenter radioimmunoscintigraphic evaluation of patients with prostate carcinoma using indium-111 capromab pendetide. Cancer. 1998; 83:739–747. PMID:
9708939.

44. Raj GV, Partin AW, Polascik TJ. Clinical utility of indium 111-capromab pendetide immunoscintigraphy in the detection of early, recurrent prostate carcinoma after radical prostatectomy. Cancer. 2002; 94:987–996. PMID:
11920467.

45. Petronis JD, Regan F, Lin K. Indium-111 capromab pendetide (ProstaScint) imaging to detect recurrent and metastatic prostate cancer. Clin Nucl Med. 1998; 23:672–677. PMID:
9790041.

46. Elgamal AA, Troychak MJ, Murphy GP. ProstaScint scan may enhance identification of prostate cancer recurrences after prostatectomy, radiation, or hormone therapy: analysis of 136 scans of 100 patients. Prostate. 1998; 37:261–269. PMID:
9831223.

47. Nagda SN, Mohideen N, Lo SS, Khan U, Dillehay G, Wagner R, et al. Long-term follow-up of 111In-capromab pendetide (ProstaScint) scan as pretreatment assessment in patients who undergo salvage radiotherapy for rising prostate-specific antigen after radical prostatectomy for prostate cancer. Int J Radiat Oncol Biol Phys. 2007; 67:834–840. PMID:
17293236.

48. Koontz BF, Mouraviev V, Johnson JL, Mayes J, Chen SH, Wong TZ, et al. Use of local (111)in-capromab pendetide scan results to predict outcome after salvage radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2008; 71:358–361. PMID:
18164863.

49. Thomas CT, Bradshaw PT, Pollock BH, Montie JE, Taylor JMG, Thames HD, et al. Indium-111-capromab pendetide radioimmunoscintigraphy and prognosis for durable biochemical response to salvage radiation therapy in men after failed prostatectomy. J Clin Oncol. 2003; 21:1715–1721. PMID:
12721246.

50. Rinnab L, Simon J, Hautmann RE, Cronauer MV, Hohl K, Buck AK, et al. [(11)C]choline PET/CT in prostate cancer patients with biochemical recurrence after radical prostatectomy. World J Urol. 2009; 27:619–625. PMID:
19234708.

51. Castellucci P, Fuccio C, Nanni C, Santi I, Rizzello A, Lodi F, et al. Influence of trigger PSA and PSA kinetics on 11C-Choline PET/CT detection rate in patients with biochemical relapse after radical prostatectomy. J Nucl Med. 2009; 50:1394–1400. [Erratum appears in J Nucl Med. 2009; 50:1578]. PMID:
19690023.

52. Scattoni V, Picchio M, Suardi N, Messa C, Freschi M, Roscigno M, et al. Detection of lymph-node metastases with integrated [11C]choline PET/CT in patients with PSA failure after radical retropubic prostatectomy: results confirmed by open pelvicretroperitoneal lymphadenectomy. Eur Urol. 2007; 52:423–429. PMID:
17397992.

53. Schilling D, Schlemmer HP, Wagner PH, Bottcher P, Merseburger AS, Aschoff P, et al. Histological verification of 11C-choline-positron emission/computed tomography-positive lymph nodes in patients with biochemical failure after treatment for localized prostate cancer. BJU Int. 2008; 102:446–451. PMID:
18410442.
54. Vees H, Buchegger F, Albrecht S, Khan H, Husarik D, Zaidi H, et al. 18F-choline and/or 11C-acetate positron emission tomography: detection of residual or progressive subclinical disease at very low prostate-specific antigen values (<1 ng/mL) after radical prostatectomy. BJU Int. 2007; 99:1415–1420. PMID:
17428249.
55. Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005; 294:433–439. PMID:
16046649.

56. Moul JW, Wu H, Sun L, McLeod DG, Amling C, Donahue T, et al. Early versus delayed hormonal therapy for prostate specific antigen only recurrence of prostate cancer after radical prostatectomy. J Urol. 2004; 171:1141–1147. [Reprint in J Urol. 2008;179(5 Suppl):S53-9; PMID: 18405753]. PMID:
14767288.

57. Shipley WU, Desilvio M, Pilepich MV, Roach M 3rd, Wolkov HB, Sause WT, et al. Early initiation of salvage hormone therapy influences survival in patients who failed initial radiation for locally advanced prostate cancer: A secondary analysis of RTOG protocol 86-10. Int J Radiat Oncol Biol Phys. 2006; 64:1162. 1167. [Erratum appears in Int J Radiat Oncol Biol Phys. 2006;65:313]. PMID:
16427211.

58. Trock BJ, Han M, Freedland SJ, Humphreys EB, DeWeese TL, Partin AW, et al. Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA. 2008; 299:2760–2769. PMID:
18560003.

59. Boorjian SA, Karnes RJ, Crispen PL, Rangel LJ, Bergstralh EJ, Blute ML. Radiation therapy after radical prostatectomy: impact on metastasis and survival. J Urol. 2009; 182:2708–2714. PMID:
19836762.

60. Choo R, Hruby G, Hong J, Bahk E, Hong E, Danjoux C, et al. (IN)-efficacy of salvage radiotherapy for rising PSA or clinically isolated local recurrence after radical prostatectomy. Int J Radiat Oncol Biol Phys. 2002; 53:269–276. PMID:
12023129.

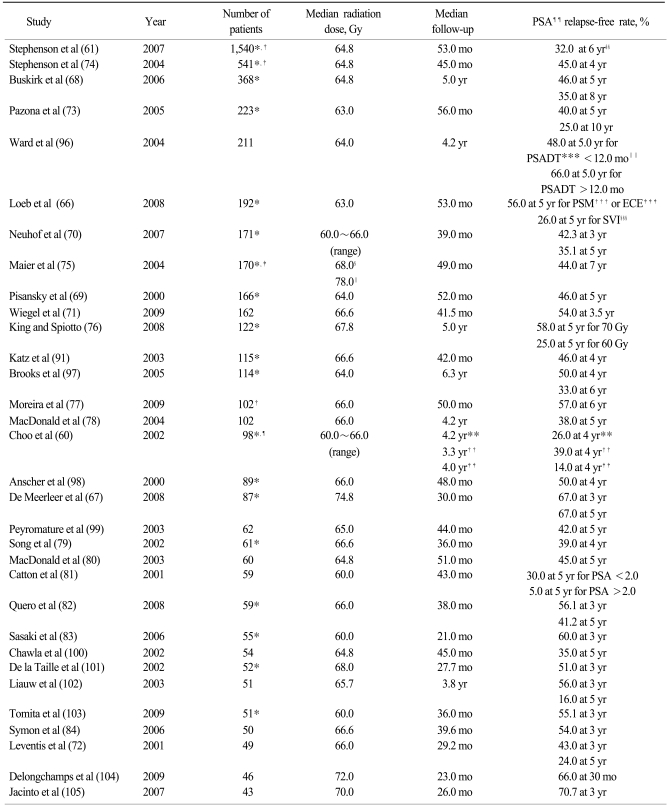
61. Stephenson AJ, Scardino PT, Kattan MW, Pisansky TM, Slawin KM, Klein EA, et al. Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol. 2007; 25:2035–2041. [Erratum appears in J Clin Oncol. 2007;25:4153]. PMID:
17513807.

62. Choo R, Morton G, Danjoux C, Hong E, Szumacher E, DeBoer G. Limited efficacy of salvage radiotherapy for biopsy confirmed or clinically palpable local recurrence of prostate carcinoma after surgery. Radiother Oncol. 2005; 74:163–167. PMID:
15734204.

63. Macdonald OK, Schild SE, Vora SA, Andrews PE, Ferrigni RG, Novicki DE, et al. Salvage radiotherapy for palpable, locally recurrent prostate cancer after radical prostatectomy. Int J Radiat Oncol Biol Phys. 2004; 58:1530–1535. PMID:
15050333.

64. Ray GR, Bagshaw MA, Freiha F. External beam radiation salvage for residual or recurrent local tumor following radical prostatectomy. J Urol. 1984; 132:926–930. PMID:
6436511.

65. Rosen EM, Cassady JR, Connolly J, Chaffey JT. Radiotherapy for localized prostate carcinoma. Int J Radiat Oncol Biol Phys. 1984; 10:2201–2210. PMID:
6439698.

66. Loeb S, Roehl KA, Viprakasit DP, Catalona WJ. Long-term rates of undetectable PSA with initial observation and delayed salvage radiotherapy after radical prostatectomy. Eur Urol. 2008; 54:88–94. PMID:
18400368.

67. De Meerleer G, Fonteyne V, Meersschout S, Van den Broecke C, Villeirs G, Lumen N, et al. Salvage intensity-modulated radiotherapy for rising PSA after radical prostatectomy. Radiother Oncol. 2008; 89:205–213. PMID:
18771809.

68. Buskirk SJ, Pisansky TM, Schild SE, Macdonald OK, Wehle MJ, Kozelsky TF, et al. Salvage radiotherapy for isolated prostate specific antigen increase after radical prostatectomy: evaluation of prognostic factors and creation of a prognostic scoring system. J Urol. 2006; 176:985–990. PMID:
16890677.

69. Pisansky TM, Kozelsky TF, Myers RP, Hillman DW, Blute ML, Buskirk SJ, et al. Radiotherapy for isolated serum prostate specific antigen elevation after prostatectomy for prostate cancer. J Urol. 2000; 163:845–850. PMID:
10687990.

70. Neuhof D, Hentschel T, Bischof M, Sroka-Perez G, Hohenfellner M, Debus J. Long-term results and predictive factors of three-dimensional conformal salvage radiotherapy for biochemical relapse after prostatectomy. Int J Radiat Oncol Biol Phys. 2007; 67:1411–1417. PMID:
17275204.

71. Wiegel T, Lohm G, Bottke D, Hocht S, Miller K, Siegmann A, et al. Achieving an undetectable PSA after radiotherapy for biochemical progression after radical prostatectomy is an independent predictor of biochemical outcome--results of a retrospective study. Int J Radiat Oncol Biol Phys. 2009; 73:1009–1016. PMID:
18963539.

72. Leventis AK, Shariat SF, Kattan MW, Butler EB, Wheeler TM, Slawin KM. Prediction of response to salvage radiation therapy in patients with prostate cancer recurrence after radical prostatectomy. J Clin Oncol. 2001; 19:1030–1039. [Erratum appears in J Clin Oncol. 2001;19:2109]. PMID:
11181666.

73. Pazona JF, Han M, Hawkins SA, Roehl KA, Catalona WJ. Salvage radiation therapy for prostate specific antigen progression following radical prostatectomy: 10-year outcome estimates. J Urol. 2005; 174:1282–1286. PMID:
16145393.

74. Stephenson AJ, Shariat SF, Zelefsky MJ, Kattan MW, Butler EB, Teh BS, et al. Salvage radiotherapy for recurrent prostate cancer after radical prostatectomy. JAMA. 2004; 291:1325–1332. PMID:
15026399.

75. Maier J, Forman J, Tekyi-Mensah S, Bolton S, Patel R, Pontes JE. Salvage radiation for a rising PSA following radical prostatectomy. Urologic Oncology. 2004; 22:50–56. PMID:
14969805.

76. King CR, Spiotto MT. Improved outcomes with higher doses for salvage radiotherapy after prostatectomy. Int J Radiat Oncol Biol Phys. 2008; 71:23–27. PMID:
18207668.

77. Moreira DM, Jayachandran J, Presti JC Jr, Aronson WJ, Terris MK, Kane CJ, et al. Validation of a nomogram to predict disease progression following salvage radiotherapy after radical prostatectomy: results from the SEARCH database. BJU Int. 2009; 104:1452–1456. PMID:
19466946.

78. MacDonald OK, Schild SE, Vora S, Andrews PE, Ferrigni RG, Novicki DE, et al. Salvage radiotherapy for men with isolated rising PSA or locally palpable recurrence after radical prostatectomy: do outcomes differ? Urology. 2004; 64:760–764. PMID:
15491716.

79. Song DY, Thompson TL, Ramakrishnan V, Harrison R, Bhavsar N, Onaodowan O, et al. Salvage radiotherapy for rising or persistent PSA after radical prostatectomy. Urology. 2002; 60:281–287. PMID:
12137827.

80. Macdonald OK, Schild SE, Vora SA, Andrews PE, Ferrigni RG, Novicki DE, et al. Radiotherapy for men with isolated increase in serum prostate specific antigen after radical prostatectomy. J Urol. 2003; 170:1833–1837. PMID:
14532786.

81. Catton C, Gospodarowicz M, Warde P, Panzarella T, Catton P, McLean M, et al. Adjuvant and salvage radiation therapy after radical prostatectomy for adenocarcinoma of the prostate. Radiother Oncol. 2001; 59:51–60. PMID:
11295206.

82. Quero L, Mongiat-Artus P, Ravery V, Maylin C, Desgrandchamps F, Hennequin C. Salvage radiotherapy for patients with PSA relapse after radical prostatectomy: a single institution experience. BMC Cancer. 2008; 8:26. PMID:
18230130.

83. Sasaki T, Nakamura K, Shioyama Y, Ohga S, Toba T, Urashima Y, et al. Low preradiotherapy prostate-specific antigen level is a significant predictor of treatment success for postoperative radiotherapy in patients with prostate cancer. Anticancer Res. 2006; 26:2367–2374. PMID:
16821618.
84. Symon Z, Kundel Y, Sadetzki S, Oberman B, Ramon J, Laufer M, et al. Radiation rescue for biochemical failure after surgery for prostate cancer: predictive parameters and an assessment of contemporary predictive models. Am J Clin Oncol. 2006; 29:446–450. PMID:
17023777.
85. King CR, Kapp DS. Radiotherapy after prostatectomy: is the evidence for dose escalation out there? Int J Radiat Oncol Biol Phys. 2008; 71:346–350. PMID:
18234451.

86. Bernard JR Jr, Buskirk SJ, Heckman MG, Diehl NN, Ko SJ, Macdonald OK, et al. Salvage Radiotherapy for Rising Prostate-Specific Antigen Levels After Radical Prostatectomy for Prostate Cancer: Dose-Response Analysis. Int J Radiat Oncol Biol Phys. 2010; 76:735–740. PMID:
19464818.

87. Feng M, Hanlon AL, Pisansky TM, Kuban D, Catton CN, Michalski JM, et al. Predictive factors for late genitourinary and gastrointestinal toxicity in patients with prostate cancer treated with adjuvant or salvage radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 68:1417–1423. PMID:
17418972.

88. Peterson JL, Buskirk SJ, Heckman MG, Crook JE, Ko SJ, Wehle MJ, et al. Late toxicity after postprostatectomy salvage radiation therapy. Radiother Oncol. 2009; 93:203–206. PMID:
19766337.

89. Pearse M, Choo R, Danjoux C, Gardner S, Morton G, Szumacher E, et al. Prospective assessment of gastrointestinal and genitourinary toxicity of salvage radiotherapy for patients with prostate-specific antigen relapse or local recurrence after radical prostatectomy. Int J Radiat Oncol Biol Phys. 2008; 72:792–798. PMID:
18707818.

90. Choo R, Danjoux C, Gardner S, Morton G, Szumacher E, Loblaw DA, et al. Efficacy of salvage radiotherapy plus 2-year androgen suppression for postradical prostatectomy patients with PSA relapse. Int J Radiat Oncol Biol Phys. 2009; 75:983–989. PMID:
19409726.

91. Katz MS, Zelefsky MJ, Venkatraman ES, Fuks Z, Hummer A, Leibel SA. Predictors of biochemical outcome with salvage conformal radiotherapy after radical prostatectomy for prostate cancer. J Clin Oncol. 2003; 21:483–489. PMID:
12560439.

92. Tiguert R, Rigaud J, Lacombe L, Laverdiere J, Fradet Y. Neoadjuvant hormone therapy before salvage radiotherapy for an increasing post-radical prostatectomy serum prostate specific antigen level. J Urol. 2003; 170:447–450. PMID:
12853796.

93. King CR, Presti JC Jr, Gill H, Brooks J, Hancock SL. Radiotherapy after radical prostatectomy: does transient androgen suppression improve outcomes? Int J Radiat Oncol Biol Phys. 2004; 59:341–347. PMID:
15145146.

94. Taylor N, Kelly JF, Kuban DA, Babaian RJ, Pisters LL, Pollack A. Adjuvant and salvage radiotherapy after radical prostatectomy for prostate cancer. Int J Radiat Oncol Biol Phys. 2003; 56:755–763. PMID:
12788182.

95. Yokomizo A, Kawamoto H, Nihei K, Ishizuka N, Kakehi Y, Tobisu KI, et al. Randomized controlled trial to evaluate radiotherapy +/- endocrine therapy versus endocrine therapy alone for PSA failure after radical prostatectomy: Japan Clinical Oncology Group Study JCOG 0401. Jpn J Clin Oncol. 2005; 35:34–36. PMID:
15681602.

96. Ward JF, Zincke H, Bergstralh EJ, Slezak JM, Blute ML. Prostate specific antigen doubling time subsequent to radical prostatectomy as a prognosticator of outcome following salvage radiotherapy. J Urol. 2004; 172:2244–2248. PMID:
15538240.

97. Brooks JP, Albert PS, Wilder RB, Gant DA, McLeod DG, Poggi MM. Long-term salvage radiotherapy outcome after radical prostatectomy and relapse predictors. J Urol. 2005; 174:2204–2208. PMID:
16280764.

98. Anscher MS, Clough R, Dodge R. Radiotherapy for a rising prostate-specific antigen after radical prostatectomy: the first 10 years. Int J Radiat Oncol Biol Phys. 2000; 48:369–375. PMID:
10974449.

99. Peyromaure M, Allouch M, Eschwege F, Verpillat P, Debre B, Zerbib M. Salvage radiotherapy for biochemical recurrence after radical prostatectomy: a study of 62 patients. Urology. 2003; 62:503–507. PMID:
12946755.

100. Chawla AK, Thakral HK, Zietman AL, Shipley WU. Salvage radiotherapy after radical prostatectomy for prostate adenocarcinoma: analysis of efficacy and prognostic factors. Urology. 2002; 59:726–731. PMID:
11992848.

101. De la Taille A, Flam TA, Thiounn N, Pontvert D, Saighi D, Zerbib M, et al. Predictive factors of radiation therapy for patients with prostate specific antigen recurrence after radical prostatectomy. BJU Int. 2002; 90:887–892. PMID:
12460351.

102. Liauw SL, Webster WS, Pistenmaa DA, Roehrborn CG. Salvage radiotherapy for biochemical failure of radical prostatectomy: a single-institution experience. Urology. 2003; 61:1204–1210. PMID:
12809898.

103. Tomita N, Kodaira T, Furutani K, Tachibana H, Nakahara R, Mizoguchi N, et al. Early salvage radiotherapy for patients with PSA relapse after radical prostatectomy. J Cancer Res Clin Oncol. 2009; 135:1561–1567. PMID:
19479278.

104. Delongchamps NB, Zerbib M, Mejean A, Rouach Y, Debre B, Peyromaure M. Conformal radiotherapy for detectable PSA following radical prostatectomy: efficacy and predictive factors of recurrence. Can J Urol. 2009; 16:4813–4819. PMID:
19796456.
105. Jacinto AA, Fede AB, Fagundes LA, Salvajoli JV, Castilho MS, Viani GA, et al. Salvage radiotherapy for biochemical relapse after complete PSA response following radical prostatectomy: outcome and prognostic factors for patients who have never received hormonal therapy. Radiat Oncol. 2007; 2:8. PMID:
17316430.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download