Abstract
Primary fallopian tube carcinoma (PFTC) is a rare tumor that histologically and clinically resembles epithelial ovarian cancer. PFTC has a worse prognosis than ovarian cancer as it is not routinely suspected and so treatment may be delayed. The early clinical manifestations and a prompt investigation can often lead to a correct diagnosis at an early stage. The preoperative diagnosis is usually difficult, and most patients with PFTC undergo laparotomy with the presumed diagnosis of ovarian carcinoma according to the presence of an adnexal mass. PFTC can present preoperatively as a tubo-ovarian abscess and it should be considered in the differential diagnosis of acute pelvic peritonitis. PFTC should be suspected by clinicians even if the presenting symptoms are atypical. We report here on two cases of PFTC along with a brief review of the literature.
Primary fallopian tube carcinoma (PFTC) is an uncommon tumor that accounts for approximately 0.14~1.8% of all female genital malignancies (1). Fallopian tube adenocarcinoma carries five-year survival rates of about 68~76% for Stage I disease, 27~42% for Stage II disease and 0~6% for Stage III and IV disease (2), so it is very important to diagnose these neoplasms in the early stages (3). Nulliparous women appear to be at a higher risk for developing PFTC (4). The typical presenting symptoms include abdominal pelvic pain or symptoms of pressure and vaginal bleeding (5). This bleeding is frequently associated with a watery vaginal discharge. 'Hydrops tubae profluens' is a syndrome that's chacterized by intermittent colicky lower abdominal pain and this relieved by a profuse, serous, watery, yellow discharge from the vagina. This is thought to be caused by filling and emptying of a partially blocked Fallopian tube. However, a correct diagnosis is rarely achieved preoperative, and in many cases, the diagnosis is made after incidental surgery for unrelated conditions (6). The classic syndrome of crampy lower abdominal pain followed by profuse watery discharge has been found only in 15% of the patients with PFTC (7), while the most common complaint was abnormal vaginal bleeding (4). PFTC is often mistaken for benign pelvic disease or ovarian cancer. Primary adenocarcinoma of the fallopian tube with papillary features is the most common histological type of primary tubal cancer (>90%). Especially, serous carcinoma appears to be the most common histologic type. Compared with ovarian carcinoma, PFTC more often presents at early stages, but it has a worse prognosis. PFTC is usually managed in the same manner as ovarian cancer (8). We report here on two cases of PFTC that presented as a tubo-ovarian abscess or an adnexal mass, and we briefly review the relevant literature.
A 68-year-old woman (gravida 2, para 2), who went through menopause at the age of 48, was admitted to the emergency department with complaints of severe lower abdominal pain, nausea, vomiting and constipation that had lasted for 7 days. Her symptoms were aggravated on the admission day. For her medical history, she was a hepatitis B antigen carrier and had taken antihypertension medication for the past 4 years. Her temperature was 38℃, her blood pressure was 150/100 mmHg and the pulse rate was 88 beats per minute. Bilateral lower quadrant tenderness with rebound tenderness was noticed on the physical examination. She had findings of acute panperitonitis. On the pelvic examination, she had cervical motion and adnexal tenderness. Trans-vaginal ultrasonography showed an adnexal multichamber cyst 7.6×5.1 cm in size located behind the uterus on the right side, and a moderate fluid collection in the pouch of Douglas (Fig. 1A). The computerized tomography (CT) scan revealed well-defined multilocular cystic lesions in the right adnexae (Fig. 1B). The white cell count on admission was 24.6×109/L and the C-reactive protein level was 21.58 mg/dl. The CA 125 antigen level was 45.85 U/mL and the CA 19-9 level was normal. Based on the clinical pictures and laboratory results, a right tubo-ovarian abscess was suspected and the patient was treated with intravenous antibiotics. Exploratory laparotomy was performed and bilateral hydrosalpinges were found. The right tubo-ovarian abscess was already ruptured with peritoneal pus, and there was severe adhesion between the intestine, both adnexae, the uterus and the omentum. The patient underwent total abdominal hysterectomy, bilateral salpingo-oophorectomy, partial omentectomy with adhesiolysis and appendectomy. The section of the right tube in the operation room revealed a dilated tube containing mostly pus-like fluid without a solid component. The histopathologic examination revealed poorly differentiated adenocarcinoma of the right fallopian tube with lamina propria involvement and no lympho-vascular invasion (Fig. 1C). The other specimen was free of tumor. A staging workup was performed and all the findings were non-specific. The patient received three cycles of postoperative adjuvant therapy with carboplatine and taxol, after which complete surgical staging was planned. Yet the patient refused our recommendations to receive further adjuvant therapy. Six months after the last chemotherapy session, the serum CA-125 level was normal and the PET-CT and pelvic MRI were normal. The patient is still alive two years after the surgery for PFTC. A recent MRI was negative for local recurrences of the disease. The serial serum CA 125 measurements have been normal since surgery.
A 60-year-old woman (gravida 0, para 0), who went through menopause at the age of 40 and with a past history of infertility, visited our outpatient clinic for her intermittent vaginal bleeding that had occurred for the previous 4 months. The vaginal bleeding was scant. The physical examination showed non-specific findings. Transvaginal sonography revealed a homogenous longitudinal mass in the right adnexa and the mass measured 4.8×2.0×2.2 cm (Fig. 2A). The pelvic CT scans revealed a solid tubular mass in the right adnexae (Fig. 2B). The CA 125, CA 19-9 and CEA levels were normal. The Pap smear was within normal limits. A diagnostic D&C was performed, which showed an inactive postmenopausal endometrium. Laparoscopy was undertaken, which revealed a normal looking uterus, left fallopian tube, both ovaries and intestinal tract; there was a solid mass seen at the ampulla portion of the right fallopian tube and the mass measured 5×2×2 cm (Fig. 2C). As the frozen sections of the right salpingectomy specimen showed malignancy, we performed exploratory laparotomy, peritoneal washing, total hysterectomy, left salpingectomy, bilateral oophorectomy, partial omentectomy and pelvic and paraaortic lymph node dissection. Histologic examination revealed papillary serous carcinoma of the right fallopian tube with serosa invasion (Fig. 2D). The uterus, both ovaries, the left fallopian tube, omentum, lymph nodes and the peritoneal washing fluid were free of tumor. The patient was diagnosed with PFTC Stage IC. She was given six courses of systemic combination chemotherapy with carboplatine and taxol, at 3-week intervals. After the second look operation, which revealed no residual tumor, she was given three additional cycles of carboplatine and taxol. The patient is still under follow-up after 16 months at the outpatient department and she is asymptomatic. Her CA 125 level and vaginal cytology are normal and CT screening has shown no abnormality.
PFTC is the least common of all gynecologic malignancies and the annual incidence about 3.6 per million women per year (9). PFTC accounts for approximately 0.14~1.8% of all female genital malignancies (1). The incidence of PFTC among all the gynecologic malignancies for the recent 5 years at our hospital was 1.09%. The peak incidence is between the ages of 60 and 64 years, with the mean age of incidence being 55 years (age range: 17~88 years) (9). In a retrospective study of 151 patients, it was noted that the patients usually present with abnormal vaginal bleeding (47.5%), lower abdominal pain (39%), abnormal watery vaginal discharge (20%) and a palpable pelvic/abdominal mass (61%) (10).
A correct diagnosis of PFTC was made preoperatively in only 4.6% of cases in the series of Alvarado-Cabrero et al. (11). There are no known predisposing factors, but it has been found to be associated with nulliparity and infertility, as well as with pelvic inflammatory disease (1). The pathogenesis is obscure. Because of its rarity, the correct preoperative diagnosis is rarely made and it is usually misdiagnosed as ovarian carcinoma. PFTC should be included in the differential diagnosis and especially if the patient has clinical symptoms such as vaginal discharge or abnormal genital bleeding with negative diagnostic curettage. Making the preoperative diagnosis of PFTC could be assisted by measurement of the serum levels of CA 125, which is elevated in 65% of PFTC patients (12). The CA 125 antigen is expressed in fallopian tube carcinoma. Therefore, CA 125 should be used in the diagnosis and follow-up. The echographic appearance of the fallopian tubes is non-specific and it mimics other pelvic diseases such as tubo-ovarian abscess, ovarian tumor and ectopic pregnancy. The echogram may show a cystic mass with spaces and mural nodules, a sausage-shaped mass or a multilobular mass with a cog-and-wheel appearance (13). Some tumors are completely solid and others are predominantly cystic and the latter contain papillary projections or solid regions. Although rare, PFTC must be considered in the differential diagnosis of adnexal masses, and particularly in the presence of incomplete septations and a highly vascular, solid component. The lesion can have the appearance of a small, solid, lobulated mass on a CT scan or MRI. On a CT scan, the lesion has attenuation equal to that of other soft tissue masses and it enhances less than the myometrium. PFTC spreads by local invasion, transluminal migration and via the lympatics and the bloodstream (1). Patients with PFTC have a higher rate of retroperitoneal and distant metastases than those patients with epitherial ovarian cancer (1). Metastases to the para-aortic lymph nodes have been documented in 33% of the patients with all stages of disease. The stage of disease at the time of diagnosis is the most important factor affecting the prognosis, and the 5-year survival rate for all the patients with fallopian tube carcinoma has been reported to range from 30% to 50% (14). The other clinicopathologic prognostic factors include residual disease after cytoreduction, the presence of ascites and the histologic grade. Surgery is the treatment of choice for PFTC, and the surgical principles are the same as those used for ovarian cancer. The procedure of choice is abdominal total hysterectomy, bilateral salpingo-oophorectomy, omentectomy, selective pelvic and para-aortic lymphadenectomy for any stage for fallopian tube carcinoma. Postoperative adjuvant chemotherapy that's similar to that used for ovarian carcinoma is employed with intravenous taxol and cisplatin being today's drug combination of choice. The role of postoperative radiotherapy is even less clear (14). Patients with Stage I disease and a higher risk of recurrence such as tumors infiltrating the serosa or tumors that have ruptured preoperatively or intraoperatively probably should be offered the same treatment as higher stage patients (12). The diagnosis of PFTC is rarely considered preoperatively and it is usually first appreciated at the time of operation or after operation by the pathologist. One of the reasons for the poor survival of patients with PFTC is that the symptoms are uncharacteristic and an ordinary gynecological examination is unreliable for detecting small, soft masses in the lower pelvis. One of our cases underwent laparoscopy for the differential diagnosis of suspicious adnexal masses before exploratory laparotomy. The other case was diagnosed by the pathologist after the operation for presumed acute panperitonitis due to tubo-ovarian abscess. PFTC should be taken into account for making the differential diagnosis of a suspicious adnexal mass or a presumptive tubo-ovarian abscess in all post-menopausal women and also in the pre-menopausal women who fail to respond to antibiotic therapy and drainage.
References
1. Riska A, Leminen A, Pukkala E. Sociodemographic determinants of incidence of primary fallopian tube carcinoma, Finland 1953-97. Int J Cancer. 2003; 104:643–645. PMID: 12594821.

2. Semrad N, Watring W, Fu YS, Hallatt J, Ryoo M, Lagasse L. Fallopian tube adenocarcinoma: common extraperitoneal recurrence. Gynecol Oncol. 1986; 24:230–235. PMID: 3710267.

3. Vaughan MM, Evans BD, Baranyai J, Weitzer MJ. Survival of patients with primary fallopian tube carcinoma. Int J Gynecol Cancer. 1998; 8:16–22. PMID: 11576282.

4. King A, Seraj IM, Thrasher T, Slater J, Wagner RJ. Fallopian tube carcinoma: a clinicopathological study of 17 cases. Gynecol Oncol. 1989; 33:351–355. PMID: 2722062.

5. Slanetz PJ, Whitman GJ, Halpern EF, Hall DA, McCarthy KA, Simeone JF. Imaging of fallopian tube tumors. AJR Am J Roentgenol. 1997; 169:1321–1324. PMID: 9353450.

6. Piura B, Rabinovich A. Primary carcinoma of the fallopian tube: study of 11 cases. Eur J Obstet Gynecol Reprod Biol. 2000; 91:169–175. PMID: 10869791.

7. Benedet JL, White GW. Coppleson M, editor. Malignant tumors of fallopian tube. Gynecologic oncology. 1981. London: Churchill Livingstone;p. 621–629.
8. Kosary C, Trimble EL. Treatment and survival for women with fallopian tube carcinoma: a population-based study. Gynecol Oncol. 2002; 86:190–191. PMID: 12144827.

9. Cohen CJ, Thoas GM, Hagopian GS, Kufe DW, Pollock RE, Holland JF, et al. Neoplasms of the fallopian tube cancer medicine. 2000. 5th ed. Canada, B.C: Decker Inc;p. 1683.
10. Baekelandt M, Jorunn Nesbakken A, Kristensen GB, Trope CG, Abeler VM. Carcinoma of the fallopian tube. Cancer. 2000; 89:2076–2084. PMID: 11066048.

11. Alvarado-Cabrero I, Young RH, Vamvakas EC, Scully RE. Carcinoma of the fallopian tube: a clinicopathological study of 105 cases with observations on staging and prognostic factors. Gynecol Oncol. 1999; 72:367–379. PMID: 10053109.

12. Baekelandt M, Kockx M, Wesling F, Gerris J. Primary adenocarcinoma of the fallopian tube: review of the literature. Int J Gynecol Cancer. 1993; 3:65–71. PMID: 11578324.

13. Kol S, Gal D, Friedman M, Paldi E. Preoperative diagnosis of fallopian tube carcinoma by transvaginal sonography and CA-125. Gynecol Oncol. 1990; 37:129–131. PMID: 2182403.

14. Rosen A, Klein M, Lahousen M, Graf AH, Rainer A, Vavra N. Austrian cooperative study group for fallopian tube carcinoma. Primary carcinoma of the fallopian tube-a retrospective analysis of 115 patients. Austrian cooperative study group for fallopian tube carcinoma. Br J Cancer. 1993; 68:605–609. PMID: 8353051.
Fig. 1
(A) Transvaginal ultrasonography showing a multilocular cyst with incomplete septation. (B) Computed tomographic scan showing the tubo-ovarian abscess-like appearance of PFTC. (C) Histologic presentation of poorly differentiated adenocarcinoma (H & E, ×200).

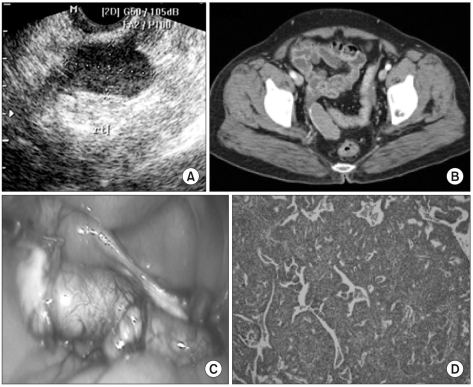
Fig. 2
(A) Transvaginal ultrasonography showing a solid mass in the right adnexae. (B) Computed tomographic (CT) scan showing a solid tubular mass of the right adnexa, and the mass is weekly enhanced. (C) Laparoscopy shows the tumor distending the right fallopian tube. Note the papillary projections out of the tube. (D) Serous carcinoma showing slit-like glandular spaces admixed with complex papillae and pasmmoma bodies (H & E, ×100).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download