Abstract
Purpose
Retinoblastoma is the most common intraocular malignancy in children. Since the 1990s, chemotherapy was indicated for intraocluar disease to reduce the frequency of enucleation and spare the complications associated with external beam radiation. In this study, we analyzed treatment results of retinoblastoma in our institute.
Materials and Methods
Datas from children diagnosed with retinoblastoma and treated at Seoul National University Children's Hospital between 1986 and 2008 were analyzed retrospectively. We utilized cyclophosphamide, vincristine, adriamycin, and methotrexate (CVAM) for OPD-based adjuvant chemotherapy. From 1990, primary chemotherapy was administered to patients with intraocular disease for eyeball-saving and patients received a combination of etoposide, vincristine, cisplatin (or ifosfamide) as a moderately intensive regimen, or a combination of cisplatin, doxorubicin, etoposide, and cycophosphamide (CDEC) as a highly intensive regimen.
Results
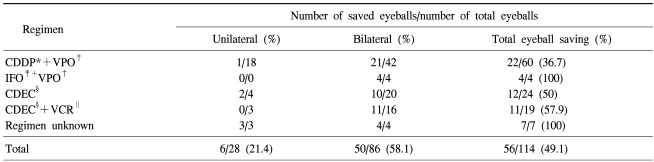
One hundred eighteen children were analyzed. There were 68 unilateral and 50 bilateral diseases. The median age at diagnosis was 1 year and Reese-Ellsworth stage V was the most common stage at the time of diagnosis. All patients were treated by chemotherapy-based multimodality methods, and primary chemotherapy was administered to 80 patients. The 10-year overall and event-free survival rate of all patients were 93.9% and 91.6%, respectively. Two patients who died were in the CDEC regimen group, but there was no significant statistical difference in survival rates by chemotherapy regimens. Fifty-six of 114 eyeballs were saved after primary chemotherapy-based treatment, and the eyeball-saving rate was 49.1%. Six patients relapsed after enucleation and 2 patients were treated successfully after autologous PBSCT. Osteosarcoma occurred in 2 patients as a secondary malignancy, and facial asymmetry after radiotherapy was the most common long-term sequelae.
Retinoblastoma is the most common tumor which occurs in the eye ball of pediatric patients, and it is known to occur at an incidence of approximately 1/15,000~30,000 in western countries (1). In the past, external beam radiotherapy or enucleation was the only treatment modality for retinoblastoma. It has been reported, however, that such complications as cataract, facial growth disturbance, optic neuropathy, facial asymmetry and secondary tumor occurred following radiotherapy (2). While the quality of life as well as a long-term survival has been considered to be crucial in patients with cancer, the methods of reducing the above complications or not performing enucleation draw the attention of physicians. In association with this, the role of chemotherapy has been gradually increasing in recent years. The primary chemotherapy has been reported to reduce the overall activity and size of tumor, thus make the local treatment possible and lower the frequency of enucleation (3,4).
Recently, the combination modality of chemotherapy with local treatments (cryotherapy, laser photocoagulation, plaque bachytherapy) or enucleation or external beam radiation has been administered to each patient according to the stage of the tumor and the response to the treatment. Also the concomitant treatment regimens have been developed, the autologous hematopoietic stem cell transplantation following a high-dose chemotherapy (5,6) has been reported to produce a long-term survival of >90% in cases of progressive disease (7,8). As a result of these changes, the number of cases in which the eyeballs are preserved is also increasing (9).
Our institution has been also making the treatment in such a manner as to enhance the eye-saving rate while improving the survival with primary chemotherapy since 1990. In 2003, our center reported that the eye-saving rate was 63% following primary chemotherapy (10). Thereafter, the primary chemotherapy combined with other treatment modalities have been performed depending on the disease stages of patients.
Through this study, we attempted to examine the treatment outcome and the results of eye-ball saving following chemotherapy based treatment at our institution in patients with retinoblastoma.
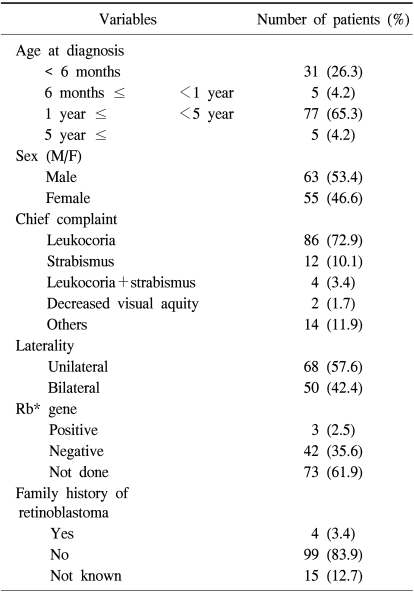
In the current study, we performed a retrospective analysis of medical records of 118 patients who were diagnosed with retinoblastoma and treated at department of pediatrics of Seoul National University Children's Hospital between December of 1986 and March of 2008. A diagnosis of retinoblastoma was made based on indirect ophthalmoscope in addition to ocular ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI). In each patient, age at the time of diagnosis, sex, a chief complaint at the time of diagnosis, laterality, a family history of retinoblastoma and the presence of Rb genes were investigated. The stage of intra-ocular tumors was determined in accordance with criteria of Reese-Ellsworth (RE) classification (11). Type of treatment modalities, treatment duration, the presence and time point of enucleation, treatment outcome, survival period and the complications following the treatment were also examined.
Prior to the effect of primary chemotherapy being demonstrated, enucleations were performed for the high stage unilateral retinoblastomas and also performed for the more progressed side eyeballs in bilateral cases while the conservative treatments were performed on the contralateral sides. After the 1990s, enucleations were performed in cases in which treatment responses were small or the lesions were progressing despite the use of chemotherapy or local treatment or those in which the vitreous seedings were present. Besides, enucleations were also considered in cases in which the vitreous hemorrhage occurred or complicated cataract was formed.
The chemotherapy was primarily performed for bilateral cases and unilateral ones in which the size and scope of tumors were small in an attempt to preserve the eye ball. In cases in which the intra-cranial invasion or metastasis were present, it was also performed to reduce the range of tumors. Furthermore, it was also performed in unilateral cases in which the invasions to optic nerve were pathologically confirmed after enucleation, those in which the invasions to cerebrospinal fluid (CSF) were suspected on histopathology and in recurred cases.
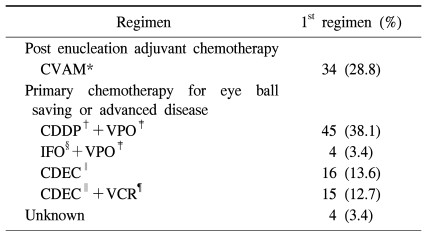
In the early stage, based on the histopathologic result and stage after enucleation, the adjuvant chemotherapy was performed using cyclophosphamide, vincristine, adriamycin and methotrexate (CVAM) in an outpatient setting. From 1990 on, for the purpose of preserving the eye balls, the primary chemotherapy was performed for the intraocular lesions based on a treatment regimen with cisplatin, etoposide and vincristine (CDDP+VPO). The chemotherapy was attempted a total of 13 times. In some patients, carboplatin was used instead of cisplatin. In cases in which the treatment responses were poor to the combination treatment using cisplatin, etoposide and vincristine or those in which the side effects such as nephrotoxicity occurred, cisplatin was replaced by ifosfamide (IFO+VPO). In cases in which no CSF invasion was identified, an intrathecal infusions of methotrexate were performed six times, and in cases in which there were CSF invasions, methotrexate, hydrocortisone, cytosine arabinoside (Ara-C) were administered via an intrathecal route. In cases of retinoblastoma in which the extraocular extensions were present, those in which the treatment responses were poor despite the alteration of treatment regimens and those in which the lesions were recurred, such drugs as cisplatin, doxorubicin, etoposide and cycophosphamide (CDEC), which had been commonly used to treat neuroblastoma, were administered as a highly-intensive regimen (12-14) (Table 1).
Radiotherapy was performed when metastases were present in the CSF or outside of the cranial cavity, and the extra-orbital metastases were confirmed on histopathology after enucleation or the recurrences were noted in areas other than the orbit. The irradiation sites included orbit, brain and spine depending on the location of lesions.
For local treatments, cryotherapy where freezing and melting were repeated three times via a sclera directly to the tumor for the purpose of necrotizing the tumor, laser therapy where a photocoagulation was performed using a diode laser to the adjacent area of the tumor for the purpose of blocking the blood supply (15) and thermotherapy (16) where the infrared ray was directly irradiated to the tumor for the purpose of inducing thermogenic shocks were administered.
In cases in which the tumor was recurred or persistently present despite a continual use of combination treatments, autologous hematopoietic stem cell transplantation following a high-dose chemotherapy was considered. In patients who are planned to undergo autologous hematopoietic stem cell transplantation, stem cells which were collected following peripheral blood stem cell mobilization (PBSCM) with the use of cyclophosphamide and etoposide were stored. Then, autologous peripheral blood stem cell transplantations (PBSCT) were performed with a conditioning regimen using carboplatin (500 mg/m2/day, d-8, -7, -6), thiotepa (300 mg/m2/day, d-5, -4, -3) and etoposide (250 mg/m2/day, d-5, -4, -3, -2).
For the assessment of the response to the prior chemotherapy, patients underwent fundoscopic examination under anesthesia (EUA) at a 1- to 2-month interval. During EUA, the residual tumor or novel lesions were examined, and the local treatments were initiated.
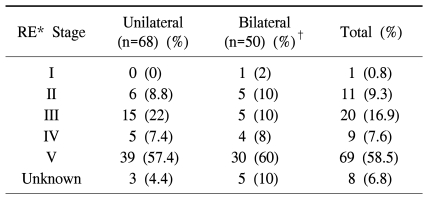
During the study period, the number of subject patients was 118 and these patients consisted of 63 men and 55 women. Median age at the time of diagnosis was 1 year (range 1 month~8 years), and median follow-up period was 63 months (range 1~236 months). Chief complaints at the time of diagnosis included 86 cases of leukocoria, 12 cases of strabismus, 4 cases of the concurrent presence of leukocoria and strabismus and 2 cases of decreased visual acuity. Our clinical series of patients included 68 unilateral cases of retinoblastoma and 50 bilateral cases. The genetic test for Rb gene was performed in the 45 patients, three had positive results. The family history of retinoblastoma was examined in 103 patients, 4 had family histories of retinoblastoma (Table 2). In accordance with Reese-Ellsworth classification at the time of diagnosis, stage IV was the most prevalent stage in both unilateral and bilateral cases (Table 3).
At the time of diagnosis, total 18 patients (15.3%) had extra-ocular invasions. Among these patients, 3 patients (2.5%) had tumor invasions in scleral emissary and two (1.7%) had tumor invasions at optic nerve resection margins. In 6 patients (5.1%), the invasions to orbit were found, and the presence of tumor cells were confirmed in the CSF in 7 patients (5.9%). There was one patient (0.8%) who had an intra-cranial metastasis on MRI scan.
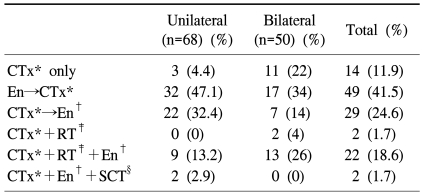
The types of treatment modalities were classified. This showed that 14 patients were given chemotherapy only and 49 were additionally given it after enucleation. Twenty nine patients underwent enucleation following the primary chemotherapy, 2 underwent the combination treatment of chemotherapy with radiotherapy. In 22 patients, chemotherapy, radiotherapy and enucleation were all performed, and 2 patients underwent hematopoietic stem cell transplantation following enucleation and chemotherapy (Table 4).
By the treatment regimens, 34 patients received CVAM, 45 did CDDP+VPO and four did IFO+VPO regimen. CDEC regimen was applied in 16 patients, and vincristine was added to CDEC regimen in 15 patients. In 6 patients, CDDP+VPO was converted to IFO+VPO because of the elevation of serum BUN and creatinine during chemotherapy. In 2 patients in whom IFO+VPO was performed, the treatment regimen was converted to CDDP+VPO because of suspected renal tubulopathy. There were 22 patients in whom second line chemotherapy regimens were alternatively performed due to the poor treatment responses or the development of novel lesions after first line chemotherapy (Table 5).
Radiotherapy was performed in 23 patients (19.5%), in whom a median value of irradiated dose was 4,500 cGy (range 3,750~11,200 cGy). Nine patients including one who got irradiation after the recurrence in the orbit received the irradiation in the orbit. Eye was the second common irradiation field in 7 patients, and 2 patients who had intra-thecal metastases and the progressive diasease got radiations in the craniospinal axis. In addition, there was one patient with a unilateral retinioblastoma who received radiation in the brain because new mass was found in the brain despite of enucleation and chemotherapy combination. The recurrence after radiotherapy was found in one patient in the orbit, and this patient started to get chemotherapy based on drugs such as intrathecal methotrexate, Ara-C and hydrocortisone. Due to the occurrence of osteosarcoma as the secondary cancer, however, this patient died during chemotherapy.
Of total patients, the datas about local treatment were available in 52 patients. This showed that 21 patients (17.8%) received cryotherapy, 12 patients (10.1%) received laser therapy and 19 patients (16.1%) received thermotherapy.
The recurrences were seen in 6 patients (5.1%). One had a recurrence in brain and CSF, one had a recurrence in bone marrow, CSF and scalp; 3 had a recurrence in orbit; and the remaining one had a recurrence in orbit and bone marrow after enucleation. Treatments after recurrences were all made based on the chemotherapy. The radiotherapy was added in one patient who had a recurrence in the orbit, and hematopoietic stem cell transplantation was performed in 2 patients. Of the 2 patients who underwent hematopoietic stem cell transplantation, one patient was a boy who was diagnosed with retinoblastoma in the right eye at the age of three years. This patient completed the treatment after the enucleation of right eye, two months later, however, multiple bone metastases were found. The patient got six cycles of chemotherapy with a CDEC regimen, thereafter he underwent autologous PBSCT with a conditioning regimen of carboplatin, thiotepa and etoposide. The total amount of hematopoietic stem cells which were administered to this patient was 5.3×106 CD34+ cells/kg. The neutrophil engraftment (absolute neutrophil count ≥0.5×109/L for 3 consecutive days) was done on day 12, and the platelet engraftment (platelet count ≥20×109/L for 7 consecutive days without transfusion) was confirmed on day 18 after the transplantation. The patient was given a 3-week course of interleukin-11 (75 µg/kg/day) from day 1. Until now, for 94 months, the patient is alive without any evidence demonstrating the tumor. The another patient was a girl who was diagnosed with retinoblastoma in the left eye, in whom the treatment was completed after the enucleation. Six months later, however, the recurrence was confirmed in the bone marrow and the orbit which was located posterior to the artificial eye on the left side. She received CDEC regimen seven times thereafter, and she received autologous PBSCT. The total amount of hematopoietic stem cells which were administered to this patient was 17.42×106 CD34+ cells/kg, the neutrophil engraftment and platelet engraftment day were day 9 and day 13, respectively. In this case, she is also still alive without disease for 4 months. In both patients, subcutaneous injections of interleukin-2 were performed at a dose of 3×106 IU/m2 from day 28, 5 times per a week at a 2-week interval during 3 months, and 13-cis retinoic acids were also administered at a dose of 100 mg/m2/day for two weeks.
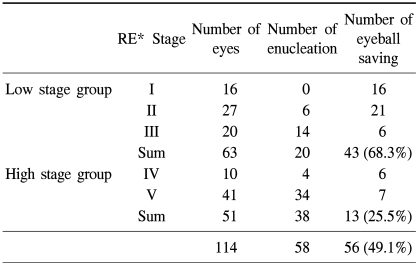
As a results of treatment, 105 of 118 patients survived during the study period; 6 were transferred to other hospitals (2 patients were hopelessly discharged); and 5 did not complete follow-up observations. The number of patients who died was 2, both of whom had bilateral presence of the lesions. In a total of 118 patients, overall survival and EFS rates were 93.9% and 91.6%, respectively (Fig. 1). According to the classification of the primary chemotherapy regimens of the survived patients, the patients of the CVAM treatment group and those of the CDDP+VPO regimen group and the IFO+VPO regimen group all survived. All death cases proved to have received CDEC regimen, in which a 10-year overall survival rate was 95.5%. As a result of primary chemotherapy for the purpose of preserving the eye ball, of a total of 114 eye balls, 56 eye balls (49.1%) were preserved. Of 71 patients, 31 (43.7%) could preserve their eye balls (Table 6). By laterality, of 68 patients with a unilateral lesion, 43 primarily received enucleation and the remaining 25 received the primary chemotherapy. Of these 25 patients, 3 were ultimately able to preserve their eye balls and their eye saving rate was 4.4%. Except for one patient who was hopelessly discharged during the treatment of a progressive disease, no patient was noted to die until the final follow-up was completed. Of 50 patients with a bilateral lesion, 23 primarily received chemotherapy. In the remaining 27 patients, the eye balls with more advanced stages of the two were enucleated priorly. Of 23 patients who underwent primary chemotherapy, 13 ultimately preserved both eye balls, 10 patients had one eye ball enucleated. Of these 10 patients, two had persistent lesions despite of the chemotherapy and radiotherapy and the remaining eyes were also enucleated. On the other hand, in 27 patients in whom the eye balls with more advanced stages of the two eye balls were priorly enucleated, the chemotherapy and radiotherapy were also performed. In six patients, however, the remaining eye balls were also enucleated, so the number of patients in whom one eye ball could be preserved was 21. In death cases, one patient died of infections with cytomegalovirus or P. jiroveci pneumonia during the anti-cancer treatment with both eye balls preserved, and the other patient died of sepsis during chemotherapy for osteosarcoma as the secondary cancer after bilateral enucleation. Except for these two patients, all the patients survived. As a result, the number of patients in whom both eyes were enucleated during the follow-up period was 8. Except for one death case, at least one eye ball was preserved in 41 of 50 bilateral cases, so the eye-saving rate was 82% (Fig. 2). In patients who primarily underwent chemotherapy, the enucleation free survival rate was 26.3%, and there was no statistically significant difference in enucleation-free survival rate between the treatment regimens (Fig. 3).
One of the death cases was undergoing chemotherapy after diagnosis of a RE stage IV bilateral retinoblastoma. Due to the suspected cytomegalovirus or P. jeroveci pneumonia and acute respiratory distress syndrome, however, the patient died one year after the treatment. Another patient was diagnosed with bilateral retinoblastoma at other institution, where the patient underwent enucleation and radiotherapy. Then, the patient was referred to our center and then received chemotherapy. Although the patient completed the treatment, the new lesions recurred. While receiving the treatment again, the patient was diagnosed with osteosarcoma in the mandible and died of sepsis during the chemotherapy.
The secondary malignancy was developed in two patients, all of which were osteosarcoma. One of them was a 10-year-old boy who was diagnosed with osteosacoma in the left mandible after the consummation of the treatment of his bilateral retinoblastoma, died during the treatment for osteosarcoma. The other patient was a 7-year-old girl who had a bilateral presence of retinoblastoma, for which the patient underwent enucleation of both eye balls and chemotherapy, then the patient completed the treatment. Five years later, however, the patient was diagnosed with osteosarcoma in the femur and lung. At the present, the patient is receiving chemotherapy for a secondary malignancy.
After the treatment, the complications were reported in 14 patients (11.9%), of which the facial asymmetry was the most prevalent one (five patients [4.2%]). All of these patients underwent radiotherapy. There were four patients with growth disturbances and one with with neurocognitive disorder, one with endocrine disorder, one with infertility, one with cerebral infarction, and one with seizure and cataract, respectively.
With the increased interest in the complications of the classical treatment modalities and in the importance of quality of life, the crucial role of chemotherapy in the treatment of retinoblastoma has been gradually increasing. With chemotherapy, the size of intraocular tumor can be decreased and thereby the local treatments can be done. A repeated use of chemotherapy and local treatments can eradicate the residual tumor and it can also avoid the use of radiotherapy causing the complications in many cases (16). In the chemotherapy for retinoblastoma, various drugs have been combined since Campinchi et al. (13) first introduced the concept of "chemoreduction" where the size of tumor was reduced with the use of such drugs as cyclophosphamide and vincristine prior to enucleation or radiotherapy in 1976. Currently in most cases, including platinum drugs like carboplatin, such drugs as etoposide or vincristine are effectively used. At the present, the effectiveness of regimens containing doxorubicin which is used to treat neuroblastoma has been demonstrated in extraocular tumors or in recurred cases (12-14). Still, however, controversial opinions exist as to the optimal combinations of drugs for the effectiveness and the optimal frequency of cycle in chemotherapy. Adverse effects occurring as a result of chemotherapy must also be considered. Such adverse effects as bone marrow suppression, fever, infection, renal dysfunction and the neurotoxicity of vincristine may occur. It must be noted that these adverse effects may lead to the death.
In the current study, we attempted to assess the treatment outcome obtained in patients with retinoblastoma who had been diagnosed and treated at our institution during a 20-year period. Particularly, the primary chemotherapy was persistently performed since the 1990s in our institution, we attempted to evaluate the treatment outcome and the results of eye-ball saving based on the chemotherapy in patients with retinoblastoma. Our results showed that the overall survival and EFS were superior to other reports (7,8). In unilateral cases, the proportion of patients who preserved the eye ball was lower, but these patients had a survival rate of 100%. In bilateral cases, 82% of patients preserved more than one eye ball. These results indicate that both unilateral and bilateral cases consorted to the treatment goals in patients with retinoblastoma. As compared with other reports, however, the proportion of eye-ball saving relative to the overall eye balls was similar or relatively lower (17-19). In particular, the enucleation free survival rate was lower in patients treated with CDEC regimen known as a highly-intensive chemotherapy as the primary chemotherapy. Presumably, these results might be due to the earlier decision on enucleation in the CDEC regimen group than the low-risk group because the CDEC regimen was performed in higher stages and in more prevalent extra-ocular invasions at the time of diagnosis. As a matter of fact, as shown in Table 6, the eye-ball saving rate was approximately 50% in the CDEC group and this was higher than that of the CDDP+VPO group (36.7%). Besides, there was no significant difference in the survival between the two groups. An enucleation free survival, which was calculated using Kaplan-Meier method, must reflect the period elapsed until enucleation was performed as well as whether the eye ball was preserved. Accordingly in interpreting these results, the stage and individual situation of each patient at the time of diagnosis must also be considered.
Given this background, whether the eye ball was preserved depending on RE stage at the time of diagnosis was summarized (Table 7). This showed a poorer treatment outcome compared to that of 2003. Although unclear, it can be inferred that the effectiveness of concomitant treatment with the primary chemotherapy had an effect on the our findings. Presumably, it would be the causes lowering the eye-ball saving rate in our series that a small number of patients (n=22) were enrolled in the study conducted in 2003 and the number of stage V eye balls was markedly greater than that of stage IV among the high-stage group in current study than in study of 2003.
In the current study, although the overall eye-saving rate was lower than the previous reports, similarly to the results of 2003's study, the eye-ball saving rate after chemotherapy in the low-stage group was markedly higher than the high-stage group. These results might support the previous reports that the primary chemotherapy could contribute to improving the treatment outcome in patients with lower stages of retinoblastoma.
To date, various treatment modalities have been combined to treat patients with retinoblastoma. Even in recent years, various new attempts have been made in a different manner from the conventional treatment modalities. In recurred cases or advanced ones, hematopoietic stem cell transplantation following a high-dose chemotherapy has been reported to produce a good treatment outcome (5). Also at our institution, two patients were given hematopoietic stem cell transplantations. In cases of advanced disease of RE stage V, Phase I and II studies have demonstrated the effectiveness of "Direct Intraarterial Chemotherapy" where anti-cancer drugs were directly administered via an ophthalmic artery to the eye ball with the use of microcatheter, ongoing studies are conducted to make this method commercially available thereafter (20). From the aspect of anti-cancer chemotherapy, other studies are currently being conducted to identify the optimal treatment regimens which are the most effective and safe (21).
In the treatment of retinoblastoma, chemotherapy has become recently popular in that it can reduce the complications and raise the eye-ball saving rate, and its effectiveness has been demonstrated throughout many studies. To date, however, no definite treatment guidelines have been established in patients with retinoblastoma. Therefore, with the development of chemotherapy regimens which are more effective and less toxic, ultimately combining the currently-available various treatment regimens with the future ones and applying a team-based approach which is customizable to each patient, continual studies are warranted to minimize the morbidity and maximize the eye-ball saving rate.
References
1. Ellsworth RM. The practical management of retinoblastoma. Trans Am Ophthalmol Soc. 1969; 67:462–534. PMID: 5381307.
2. Phillips C, Sexton M, Wheeler G, McKenzie J. Retinoblastoma: review of 30 years' experience with external beam radiotherapy. Australas Radiol. 2003; 47:226–230. PMID: 12890239.
3. Gombos DS, Chevez-Barrios AP. Current treatment and management of retinoblastoma. Curr Oncol Rep. 2007; 9:453–458. PMID: 17991352.

4. De Potter P. Current treatment of retinoblastoma. Curr Opin Ophthalmol. 2002; 13:331–336. PMID: 12218465.

5. Lee SH, Yoo KH, Sung KW, Kim JY, Cho EJ, Koo HH, et al. Tandem high-dose chemotherapy and autologous stem cell rescue in children with bilateral advanced retinoblastoma. Bone Marrow Transplant. 2008; 42:385–391. PMID: 18574441.

6. Matsubara H, Makimoto A, Higa T, Kawamoto H, Sakiyama S, Hosono A, et al. A multidisciplinary treatment strategy that includes high-dose chemotherapy for metastatic retinoblastoma without CNS involvement. Bone Marrow Transplant. 2005; 35:763–766. PMID: 15750608.

7. Yang MH, Eun SH, Park CS, Son JA, Kim JY, Ko JW, et al. A study of the Survival Rate of Childhood Cancer in Korea. Cancer Res Treat. 2001; 33:191–198.

8. Shields CL, Shields JA, De Potter P. New treatment modalities for retinoblastoma. Curr Opin Ophthalmol. 1996; 7:20–26. PMID: 10163455.

9. Abramson DH, Niksarli K, Ellsworth RM, Servodidio CA. Changing trends in the management of retinoblastoma: 1951-1965 vs 1966-1980. J Pediatr Ophthalmol Strabismus. 1994; 31:32–37. PMID: 8195960.

10. Kim JH, Yu YS, Khwarg SI, Choi HS, Shin HY, Ahn HS. Clinical result of prolonged primary chemotherapy in retinoblastoma patients. Korean J Ophthalmol. 2003; 17:35–43. PMID: 12882506.

11. Reese AB, Ellsworth RM. The evaluation and current concept of retinoblastoma therapy. Trans Am Acad Ophthalmol Otolaryngol. 1963; 67:164–172. PMID: 13973597.
12. Akiyama K, Iwasaki M, Amemiya T, Yanai M. Chemotherapy for retinoblastoma. Ophthalmic Paediatr Genet. 1989; 10:111–116. PMID: 2779981.

13. Campinchi R, Lemerle J, Bloch-Michel E, Pinget T, Schweisguth O, Luker P, et al. Does chemotherapy have a role in the treatment of retinoblastomas? BullSoc Ophtalmol Fr. 1976; 76:17–22.
14. Matthay KK, O'Leary MC, Ramsay NK, Villablanca J, Reynolds CP, Atkinson JB, et al. Role of myeloablative therapy in improved outcome for high risk neuroblastoma: review of recent Children's Cancer Group results. Eur J Cancer. 1995; 31A(4):572–575. PMID: 7576971.

15. Han SB, Kim JH, Choung HK, Kim SJ, Khwarg SI, Yu YS. The clinical courses of retinoblastoma patients who underwent bilateral enucleation. J Korean Ophthalmol Soc. 2007; 48:1234–1241.

16. Chintagumpala M, Chevez-Barrios P, Paysse EA, Plon SE, Hurwitz R. Retinoblastoma: review of current management. Oncologist. 2007; 12:1237–1246. PMID: 17962617.

17. Lee V, Hungerford JL, Bunce C, Ahmed F, Kingston JE, Plowman PN. Globe conserving treatment of the only eye in bilateral retinoblastoma. Br J Ophthalmol. 2003; 87:1374–1380. PMID: 14609838.

18. Migdal C. Bilateral retinoblastoma: the prognosis for vision. Br J Ophthalmol. 1983; 67:592–595. PMID: 6882716.

19. Sanders BM, Draper GJ, Kingston JE. Retinoblastoma in Great Britain 1969-80: incidence, treatment, and survival. Br J Ophthalmol. 1988; 72:576–583. PMID: 3415951.

20. Suzuki S, Kaneko A. Management of intraocular retinoblastoma and ocular prognosis. Int J Clin Oncol. 2004; 9:1–6. PMID: 15162819.

21. Zage PE, Reitman AJ, Seshadri R, Weinstein JL, Mets MB, Zeid JL, et al. Outcomes of a two-drug chemotherapy regimen for intraocular retinoblastoma. Pediatr Blood Cancer. 2008; 50:567–572. PMID: 17729249.

Fig. 1
Kaplan-Meier analysis of total patients. (A) Ten-year overall survival rate; (B) Ten-year event-free survival rate of total patients.
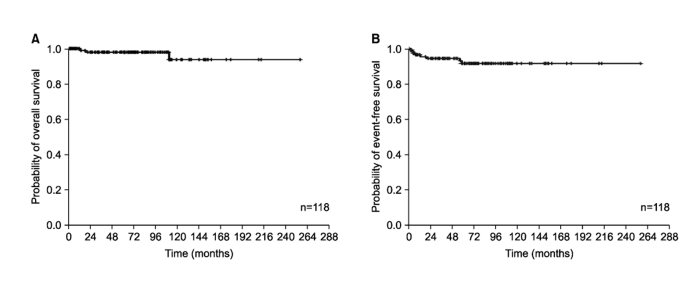
Fig. 2
Treatment flow by laterality and the numbers of patients whose eyes saved. CTx: chemotherapy, En: enucleation, *One of them died due to cytomegalovirus or P.jirovceci pneumonia. †One of them died due to septic shock during chemotherapy to secondary malignancy.
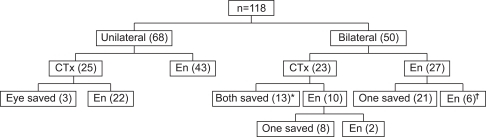
Fig. 3
Kaplan-Meier analysis of enucleation free survival rate in total patients with primary chemotherapy.
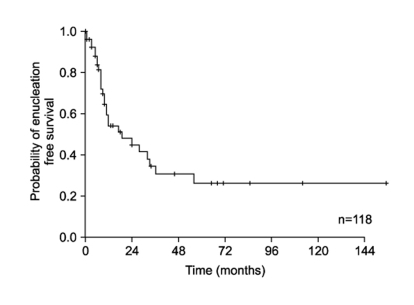
Table 1
Chemotherapy regimens
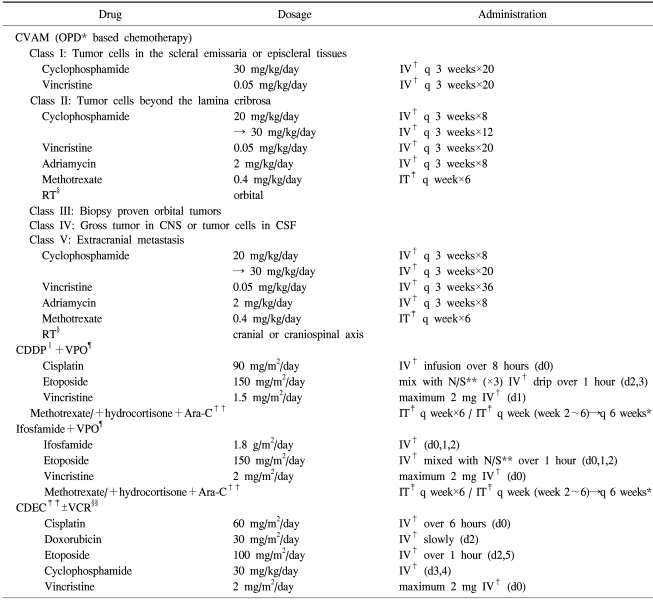
*outpatient department, †intravenous, ‡intrathecal, §radiotherapy, ∥cisplatin, ¶etoposide+vincristine, **normal saline, ††cytosine arabinoside, ‡‡cisplatin+doxorubicin+etoposide+cyclophosphamide, §vincristine.
If initial CSF cytospin was positive, intrathecal triple therapy were applied weekly during first 5 weeks, and every 6 weeks afterward.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download