A 43-year-old man presented with a painless testicular mass (
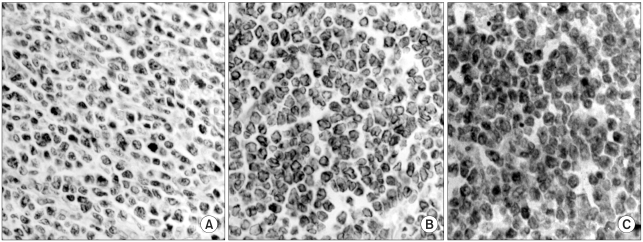
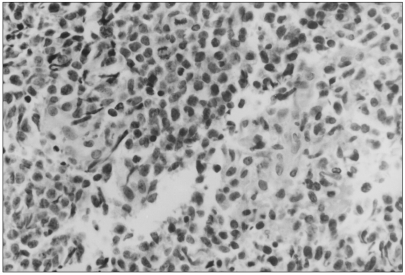
Fig. 1). The pathologic diagnosis of the radical orchiectomy specimen revealed PTCL-u (
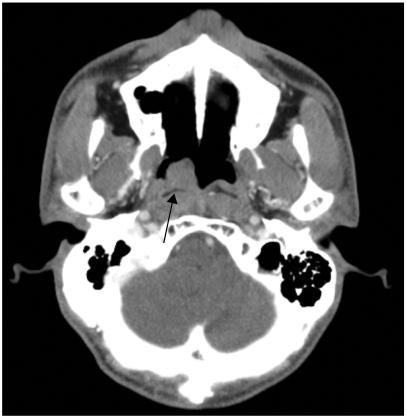
Fig. 2), and further staging evaluation (bone marrow biopsy, computerized scan of the abdomen, pelvis and nasopharynx, and cytology of the cerebrospinal fluid) showed a right nasopharyngeal mass (
Fig. 3). which was also confirmed as PTCL-u (
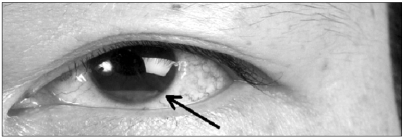
Fig. 4). Immunohistochemical staining showed CD3(+), CD4(-), CD20(-), CD56(+), CD68(-), granzyme(-) and Epstein-Barr virus(-). His clinical stage was III according to the Ann Arbor staging system. He received the first-line chemotherapy with four courses of CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) regimen followed by involved-field radiotherapy (4400 cGy) to the testis and nasopharynx, and he subsequently achieved complete remission according to the International Working Group criteria. Two months after achieving complete response, the patient complained of progressively worsening vision in his left eye. The external eye examination was normal except for a pseudohypopyon in his left eye (
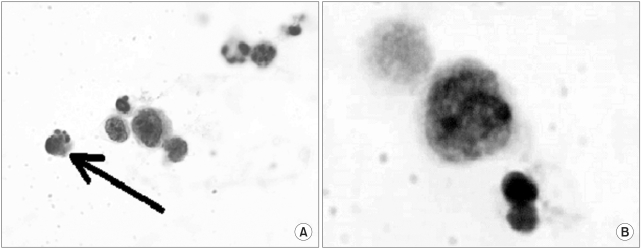
Fig. 5). The vitreous and posterior segments were normal as were the conjunctiva, lens and sclera of the left eye. The intraocular pressures were 12 mmHg in the right eye and 15 mmHg in the left eye. The ultrasound biomicroscopic imaging of his left eye revealed a mass-like lesion in the left ciliary body, so anterior chamber aspiration was performed. The cells obtained in the aqueous aspirate were described morphologically as atypical lymphocytes with mercury drop-like apoptotic bodies (
Fig. 6), which were characteristic of lymphoma. The CSF examination, brain imaging and the abdomen and pelvis computerized scanning showed no evidence of disease recurrence. A week after initiation of chemotherapy with high dose cyclophosphamide, the follow-up ultrasound biomicroscopic imaging showed complete disappearance of the infiltration and the anterior chamber aspirate was cleared. Following autologous peripheral stem cell transplantation, he achieved a second complete remission (International Working Group criteria). Yet three months after the patient achieved his secondary complete remission, the patient developed dysphagia. Esophagogastroduodenoscopy and computerized scanning of the pharynx could not reveal the cause of the dysphagia. A modified barium swallowing test showed ataxia of the pharyngeal wall motion. Magnetic resonance imaging of the brain demonstrated parenchymal enhancement of the cerebellum, linear enhancement at the anterior aspect of both cerebral peduncles and tiny enhancing foci of the left parietal cortex (
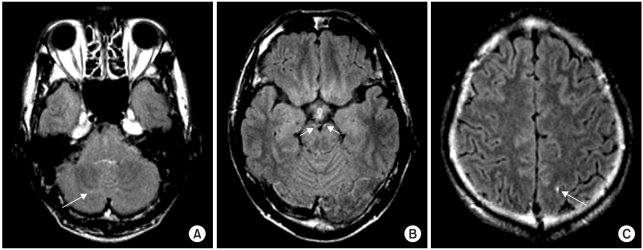
Fig. 7). Leptomeningeal seeding was confirmed by cytologic examination of the cerebrospinal fluid. Treating him with intrathecal methotrexate was unsuccessful; the patient succumbed to the disease 11 months after the initial diagnosis.
 | Fig. 1CT scan of the pelvis showed the heterogeneously enhancing mass that originated from the left testicle. 
|
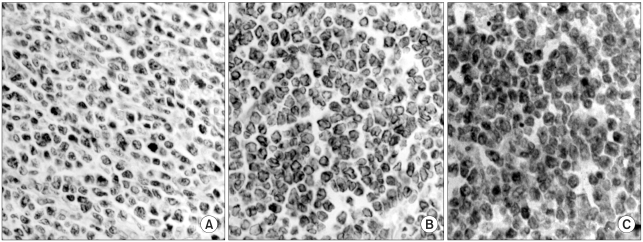 | Fig. 2Orchiectomy specimen of the left testis showed malignant lymphoma with focal angioinvasion, and this was consistant with peripheral T cell lymphoma (A: H&E, ×400), and the positive immunohistochemical staining with CD3 (B: ×400), and CD56 (C: ×400). 
|
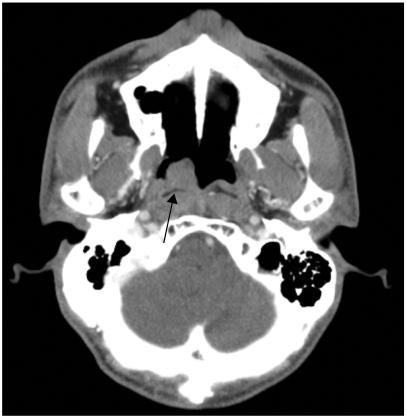 | Fig. 3Nasopharynx CT displayed polyphoid lesion of the right nasopharynx. 
|
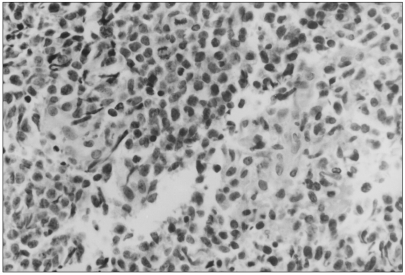 | Fig. 4Nasopharynx biopsy revealed the involvement of peripheral T cell lymphoma (H&E, ×400). 
|
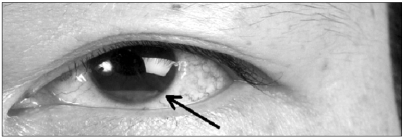 | Fig. 5Pseudohypopyon of the left eye. 
|
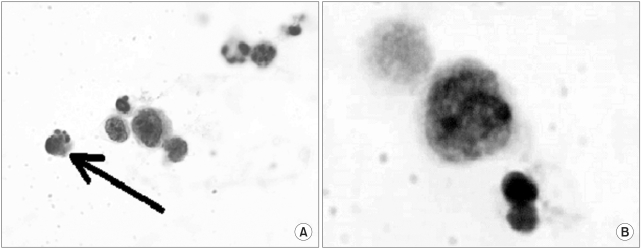 | Fig. 6Aspiration of the anterior chamber showed atypical lymphocytes with mercury drop-like apoptotic bodies, suggestive of lymphomatous cells (H&E, A: ×40, B: ×200). 
|
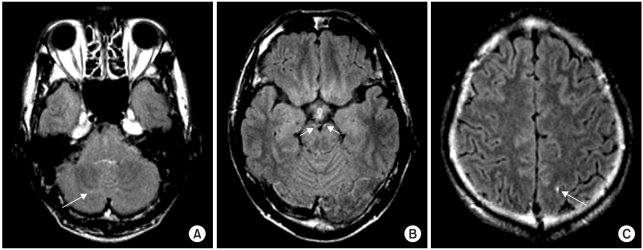 | Fig. 7Brain MRI demonstrated parenchimal enhancement of the cerebellum (A), linear enhancement at the anterior aspect of both cerebral peduncles (B) and tiny enhancing foci of the left parietal cortex (C). 
|





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download