Abstract
Purpose
The aim of study was to evaluate the usefulness of serum HER2 as a therapeutic response indicator in patients with HER2 positive metastatic breast cancer (MBC).
Materials and Methods
The levels of serum HER2 and CA15.3 were assayed in 148 serial serum samples from 50 HER2 positive MBC patients at both the baseline and follow-ups. The changes in the levels of serum HER2 and CA15.3 in relation to the tumor responses to the various chemotherapy regimens were monitored.
Results
The levels of serum HER2 and CA15.3 were elevated in 82% and 62% of tissue HER2 positive patients, respectively, prior to therapies, with the changes in both tumor markers showing statistical significance in relation to the tumor responses (p<0.01) in patients with elevated baseline serum markers.
Conclusion
The level of serum HER2 could be a valuable response indicator, not only for trastuzumab containing therapy, but also for other common MBC chemotherapeutic agents. Also, as it is more frequently elevated, the serum level of HER2 may also be a more useful tumor marker than CA15.3 in HER2 positive MBC.
The HER2 (c-erbB-2/neu) proto-oncogene has received much attention in recent years, especially since the availability of the anti-HER2 targeted monoclonal antibody, trastuzumab (Herceptin), for the treatment of advanced breast cancer (1,2). The HER2 gene encodes a 185-kDa glycoprotein growth factor receptor consisting of three domains, including the extracellular, transmembrane and intracellular domains (3). The extracellular ligand binding domain of HER2 is known to undergo proteolytic cleavage from the full-length protein, with its subsequent release into the circulation of patients with breast cancer (4~6). The level of serum HER2 is elevated in about 20~40% of patients with overall metastatic breast cancer, with this increased HER2 level being associated with a worse prognosis and resistance to hormone therapy or alkylating chemotherapy (7~12). Although the role of serum HER2 as a marker for the prognosis and prediction of response has been investigated in several studies, the clinical utility of serum HER2 for monitoring the response to various chemotherapeutic agents, other than trastuzumab containing therapies, requires further studies. Therefore, we selected patients with HER2 positive (immunohistochemistry (IHC) 3+ or fluorescence in situ hybridization (FISH) +) metastatic breast cancer, who had undergone chemotherapy with various agents, including trastuzumab, as well as various other chemotherapeutic agents, with the aim of evaluating the usefulness of serum HER2 for monitoring the responses to the treatment. We serially measured the level of serum HER2 at the baseline and during follow-ups, and correlated these levels with the clinical tumor responses to investigate how accurately fluctuations of the serial serum HER2 levels reflected the actual clinical response status to various therapies in HER2 positive metastatic breast cancer patients. We concurrently measured the level of serum CA15.3, a commonly used tumor marker for assessing the tumor responses in metastatic breast cancer patients in clinical practice, to compare the accuracy of the level of serum HER2 for reflecting tumor responsiveness.
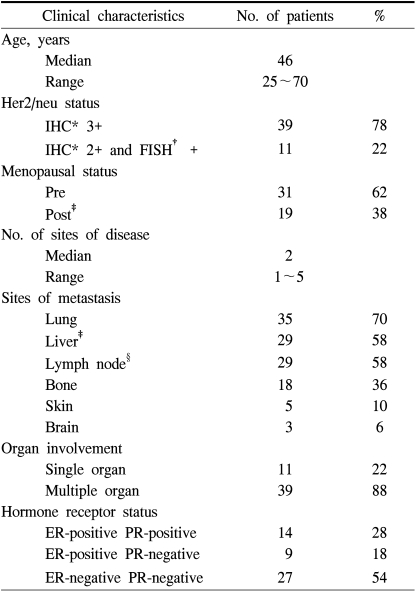
A total of 148 serial serum samples, with a median of 3 (range, 2~6) samples per patient were obtained for analysis from 50 patients prior to treatments and during follow-ups. The average period from the initial sampling to the evaluation of the first tumor response was 12 weeks (range: 5~30 weeks). All patients had IHC 3+ or FISH positive metastatic breast cancer with measurable lesions. The following clinical characteristics were evaluated in relationship with these markers: age, estrogen and progesterone receptor status, site and number of metastases, as well as therapeutic regimens consisting of trastuzumab based therapy and other forms of chemotherapy.
Blood was drawn into serum separating tubes and then centrifuged at 2,000 g for 10 minutes at the room temperature. Aliquots of serum were then placed in polypropylene tubes and stored at -20℃.
The tumor response was assessed using appropriate measurements or by radiological evaluation of the CT or MRI. Complete response (CR) required the complete disappearance of all disease for at least 4 weeks. Partial response (PR) was defined as a ≥50% decrease in the sum of the products of two diameters of all measurable lesions and stabilization of all non-measurable lesions maintained for a minimum of at least 4 weeks. Stable disease (SD) consisted of a <50% decrease in the sum of the products of two diameters of all measurable lesions. Progressive disease (PD) was defined as a >25% increase in the sum of the products of two diameters of one or more measurable tumors, or an unequivocal increase of new lesions. At the same time the tumor responsiveness to therapy was assessed, the levels of serum HER2 and CA15.3 were also measured. The median interval from the baseline to the evaluation of the first tumor response was 12 weeks (range 5~30 weeks). The tumor responsiveness to therapy and serum HER2 and CA 15-3 were simultaneously assessed and measured, respectively. The median interval from the baseline to the evaluation of tumor response was 9 weeks (range, 3~24 weeks).
To determine the normal cutoff values of the level of serum HER2 in Korean women, samples were collected from 93 healthy volunteers. The informed consent was obtained from all those participating in the present study. The levels of serum HER2 and CA15.3 were measured using the ADVIA Centaur immunoassay system (Bayer Diagnostics, Tarrytown, NY). This assay employs sandwich immunoassay technology, with direct chemiluminescence for optimal assay performance. All samples were analyzed without knowledge of the clinical outcome of an individual patient.
The SPSS software was used for all statistical analyses. To evaluate an association of clinical variables with the baseline levels of serum HER2 and CA15.3, we performed χ2 testing. The association between serum HER2 and CA15.3, estimated using a correlation analysis, and the difference of tumor response rate according to pretreatment serum HER2 or CA15.3 levels were evaluated using the Pearson χ2 test.
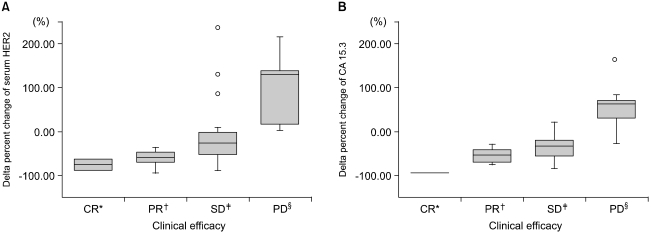
To confirm differences between the pretreatment and follow-up tumor marker levels for each therapeutic response, the Wilcoxon signed rank test was used. For patients having elevated baseline levels of serum HER2 or CA15.3, we simultaneously calculated the delta percent change {(Level of follow-up-Level of baseline)/Level of baseline} for evaluation of the usefulness of serum tumor markers with respect to the therapeutic response and the clinical efficacy. The difference in the delta percent change between subgroups with a different tumor response was evaluated using the Kruskal- Wallis test.
The median age of the patients was 46 years (range: 25~70). The clinical characteristics of the patients are described in Table 1. The median age of the healthy volunteers used to determine the serum HER2 cutoff levels was 34 years (range: 21~66). While the data derived from the 93 volunteers showed a mean +2SD of 10.2µg/L for serum HER2, the manufacturer's recommendation for the cutoff level for serum HER2, 15µg/L, was used. The serum CA15.3 cutoff level was 38 kilo units/L (kU/L).
The baseline levels of serum HER2 prior to therapy ranged from 8.8 to 2589.6µg/L (median, 38.0µg/L), with 41 HER2 positive metastatic breast cancer patients (82%) having elevated serum HER2 levels in their tissues. The CA15.3 levels were elevated in 31 patients (62%), ranging from 3.5 to 2817.4 kU/L (median, 54.9 kU/L). Twenty-six patients (52%) showed elevation of both markers, and 4 (8%) had no elevation of either tumor marker.
There was no significant association between the level of serum HER2 and the clinical variables, with the exception of lymph node metastasis. The levels of serum HER2 (mean±SD; 115±41) of those patients with lymph node metastasis was significantly lower than for those without (mean±SD; 399±142) (p<0.05). The CA15.3 levels showed positive correlations with estrogen receptor positivity and liver metastasis (p<0.05). A weak correlation was also observed between the serum HER2 and CA15.3 concentrations (correlation coefficient 0.29, p<0.05).
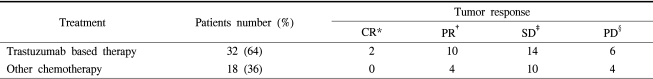
The treatment regimens used were trastuzumab (18%), trastuzumab/taxane (28%), trastuzumab/vinorelbine (18%), anthracycline-containing regimen (14%), capecitabine (16%), gemcitabine (4%) and letrozole (2%). The tumor responses according to the therapeutic regimens are shown in Table 2. The pretreatment levels of serum HER2 and CA15.3 had no influence on the clinical response to the therapeutic regimen, and there was a statistically significant correlation between the pretreatment and follow-up levels of serum HER2 in patients with a tumor response (CR and PR) or PD (p<0.05). However, the CA15.3 level only showed a statistically significant change in patients with PD (p<0.05). The delta percent change was estimated at the time the tumor response was evaluated (Fig. 1). The delta percent changes in the levels of serum HER2 and CA15.3 in patients with either CR or PR were greater than -37 and -31%, respectively. In patients with PD, increases were observed in both tumor markers, with the exception of one patient who showed a decreased CA15.3 level; the mean delta percent changes were +94 and +56% for the levels of serum HER2 and CA15.3, respectively. However, the range of the delta percent changes in the levels of either the serum HER2 or CA15.3 in patients with PD did not discriminate between SD and PD due to the wide and overlapping ranges for PD, from 3 to 216% for serum HER2, and from -29 to 164% for CA15.3; for SD the ranges were from -90 to 238% and from -87 to 21% for serum HER2 and CA15.3 levels, respectively. However, a statistically significant differences were observed between the delta percent changes of levels of serum HER2 or CA15.3 and the responses (p<0.01), which were consistent irrespective of the therapeutic regimen.
Monitoring of the therapeutic response in patients with metastatic breast cancer is often difficult due to the lack of measurable lesions, such as in cases with bone metastasis or isolated pleural-based disease. Therefore, a reliable serum tumor marker able to reflect the clinical response of patients with metastatic breast cancer would be beneficial and useful. In previous studies, elevation of the CA15.3 level ranged from 50 to 90% in metastatic breast cancer, which was dependent on the anatomical sites of metastases, with the role of the CA15.3 level emphasized for monitoring the treatment of metastatic breast cancer. However, the positive rate of the level of serum HER2 elevation in patients with metastatic breast cancer has generally been lower than that of CA15.3, which has been reported in about 20~40% of cases (13,14). The baseline level of serum HER2 was elevated in 82% of the cases with HER2 positive metastatic breast cancer in this study, as the level of serum HER2 has a significant correlation with the expression of HER2 in tumor tissue (9,15). In a previous study, the utility of serum and tissue HER2 for the early diagnosis of recurrence was assessed in only a few breast cancer patients, but the serum HER2 sensitivity was reported to be significantly higher in patients overexpressing HER2 in their tissues (8/10, 80%) than in those without overexpression (1/30, 3.3%) (p=0.0001), which was comparable to the 82% (41/50) positivity found in our study (16). Fifteen patients (30%) in our study had elevated serum HER2 levels, but without serum CA15.3 elevation at the baseline. This particular group may derive the most benefit from serial HER2 level monitoring for tumor responses, especially in cases without measurable lesions, such as for either bone or pleural fluid only diseases. Moreover, the longitudinal variations of the levels of serum HER2 were concordant with the clinical tumor responses to the anticancer therapy, regardless of the regimen. Cheung et al studied 30 metastatic breast cancer patients, who received docetaxel-based and anthracycline therapy, and observed sequential changes in the level of serum HER2 completely paralleled the initial response in less than 9 patients with positive tissue staining, as in our study (17). This study encompassed commonly used chemotherapeutic drugs used in the treatment of breast cancer, such as anthracycline containing regimens, capecitabine and gemcitabine, while most of the serum HER2 studies in the literature focused on the use of trastuzumab containing therapies.
No common guidelines on to how to assess the curves of variations in serum tumor markers have been found with respect to the clinical response. When tumor markers are applied, with the only the criterion of either an elevation or non-elevation during the follow-up, as executed by some investigators, the changing trends in the tumor marker may not be quantitatively reflected (18~20). Hence, we used the delta percent change to evaluate the quantitative correlation of either the level of serum HER2 or CA15.3 with the tumor response during follow-up. While a 10% change in the level of the tumor marker from that of the baseline has been regarded as a significant elevation or decline in a previous study (21), those patients with a SD in the present study often had a change of greater than 10% in their level of serum HER2 or CA15.3. While all responders showed normalization or undetectable serum HER2 levels in a previous study (18), in our study not all the responders achieved serum HER2 normalization, but had decreases in the levels of serum HER2 and CA15.3 greater than 37 and 31%, respectively. Therefore, a sufficient decrease in the level of a tumor marker may implicate a tumor response, even when the level does not decrease below the cutoff levels on follow-up. Likewise, a sufficient rise in the level of a of tumor marker from the nadir or plateau level on follow-up may be indicative of tumor progression, even if this rise is still below the baseline level of the tumor marker, as is often seen with conventional tumor markers.
The correlation of several clinical parameters, including visceral metastases, such as lung and liver metastasis, with an increased level of serum HER2, has been reported (22,23). However, our data showed no such correlation, with the exception of lymph node metastasis. In patients with lymph node metastasis, the level of serum HER2 showed a significantly lower level than in patients without lymph node involvement (p<0.05), which was most likely attributable to the low tumor volumes in those patients with positive lymph nodes.
It has been suggested that patients with a high pretreatment level of serum HER2 show significantly lower response rates to certain chemotherapy or hormone therapy than those without increased marker concentrations. Whether an increased baseline level of serum HER2 is predictive of a response to trastuzumab-based therapy remains controversial (1,9,10,25). In our study, the pretreatment baseline level of serum HER2 did not appear predictive of clinical responses to any particular therapeutic regimen, as the low baseline level may merely reflect a low tumor volume in the tissue of our HER2 positive population.
The level of serum HER2 appears to be a useful tumor marker for monitoring HER2 positive metastatic breast cancer, irrespective of the therapeutic regimen, with respect to the high rate of serum HER2 level elevation as well as the good concordance rate of tumor responses in HER2 positive metastatic breast cancer tissue. Moreover, the level of serum HER2 appears to be a better tumor marker than that of the serum CA15.3 level for HER2 positive metastatic breast cancer, mainly due to its level of elevation in these patients. A close follow-up on the serial level of serum HER2, especially in cases without a measurable disease, may prevent the prolonged administration of ineffective therapies, which would consequently help initiate successive lines of therapy in HER2 positive metastatic breast cancer.
References
1. Cobleigh MA, Vogel CL, Tripathy D, Robert NJ, Scholl S, Fehrenbacher L, et al. Multinational study of the efficacy and safety of humanized anti-HER2 monoclonal antibody in women who have HER2-overexpressing metastatic breast cancer that has progressed after chemotherapy for metastatic disease. J Clin Oncol. 1999; 17:2639–2648. PMID: 10561337.

2. Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001; 344:783–792. PMID: 11248153.

3. Maguire HC Jr, Greene MI. The neu (c-erbB-2) oncogene. Semin Oncol. 1989; 16:148–155. PMID: 2565604.
4. Lin YZ, Clinton GM. A soluble protein related to the HER-2 proto-oncogene product is released from human breast carcinoma cells. Oncogene. 1991; 6:639–643. PMID: 1674366.
5. Zabrecky JR, Lam T, McKenzie SJ, Carney W. The extracellular domain of p185/neu is released from the surface of human breast carcinoma cells, SK-BR-3. J Biol Chem. 1991; 266:1716–1720. PMID: 1671042.

6. Leitzel K, Teramoto Y, Sampson E, Mauceri J, Langton BC, Demers L, et al. Elevated soluble c-erbB-2 antigen levels in the serum and effusions of a proportion of breast cancer patients. J Clin Oncol. 1992; 10:1436–1443. PMID: 1355522.

7. Fehm T, Maimonis P, Weitz S, Teramoto Y, Katalinic A, Jager W. Influence of circulating c-erbB-2 serum protein on response to adjuvant chemotherapy in node-positive breast cancer patients. Breast Cancer Res Treat. 1997; 43:87–95. PMID: 9065602.

8. Mehta RR, McDermott JH, Hieken TJ, Marler KC, Patel MK, Wild LD, et al. Plasma c-erbB-2 levels in breast cancer patients: prognostic significance in predicting response to chemotherapy. J Clin Oncol. 1998; 16:2409–2416. PMID: 9667258.

9. Colomer R, Montero S, Lluch A, Ojeda B, Barnadas A, Casado A, et al. Circulating HER2 extracellular domain and resistance to chemotherapy in advanced breast cancer. Clin Cancer Res. 2000; 6:2356–2362. PMID: 10873087.
10. Hayes DF, Yamauchi H, Broadwater G, Cirrincione CT, Rodrigue SP, Berry DA, et al. Circulating HER-2/erbB-2/c-neu (HER-2) extracellular domain as a prognostic factor in patients with metastatic breast cancer: Cancer and Leukemia Group B Study 8662. Clin Cancer Res. 2001; 7:2703–2711. PMID: 11555582.
11. Lipton A, Ali SM, Leitzel K, Demers L, Chinchilli V, Engle L, et al. Elevated serum Her-2/neu level predicts decreased response to hormone therapy in metastatic breast cancer. J Clin Oncol. 2002; 20:1467–1472. PMID: 11896093.

12. Cheung KL, Graves CR, Robertson JF. Tumour marker measurements in the diagnosis and monitoring of breast cancer. Cancer Treat Rev. 2000; 26:91–102. PMID: 10772967.

13. Seregni E, Coli A, Mazzucca N. Circulating tumour markers in breast cancer. Eur J Nucl Med Mol Imaging. 2004; 31(Suppl 1):S15–S22. PMID: 15127239.

14. Baselga J. Is circulating HER-2 more than just a tumor marker? Clin Cancer Res. 2001; 7:2605–2607. PMID: 11555569.
15. Sugano K, Ushiama M, Fukutomi T, Tsuda H, Kitoh T, Ohkura H. Combined measurement of the c-erbB-2 protein in breast carcinoma tissues and sera is useful as a sensitive tumor marker for monitoring tumor relapse. Int J Cancer. 2000; 89:329–336. PMID: 10956406.

16. Burstein HJ, Harris LN, Marcom PK, Lambert-Falls R, Havlin K, Overmoyer B, et al. Trastuzumab and vinorelbine as first-line therapy for HER2-overexpressing metastatic breast cancer: multicenter phase II trial with clinical outcomes, analysis of serum tumor markers as predictive factors, and cardiac surveillance algorithm. J Clin Oncol. 2003; 21:2889–2895. PMID: 12885806.

17. Cook GB, Neaman IE, Goldblatt JL, Cambetas DR, Hussain M, Luftner D, et al. Clinical utility of serum HER-2/neu testing on the Bayer Immuno 1 automated system in breast cancer. Anticancer Res. 2001; 21:1465–1470. PMID: 11396233.
18. Fehm T, Gebauer G, Jager W. Clinical utility of serial serum c-erbB-2 determinations in the follow-up of breast cancer patients. Breast Cancer Res Treat. 2002; 75:97–106. PMID: 12243512.

19. Robertson JF, Jaeger W, Syzmendera JJ, Selby C, Coleman R, Howell A, et al. European Group for Serum Tumour Markers in Breast Cancer. The objective measurement of remission and progression in metastatic breast cancer by use of serum tumour markers. Eur J Cancer. 1999; 35:47–53. PMID: 10211087.

20. Ali SM, Leitzel K, Chinchilli VM, Engle L, Demers L, Harvey HA, et al. Relationship of serum HER-2/neu and serum CA 15-3 in patients with metastatic breast cancer. Clin Chem. 2002; 48:1314–1320. PMID: 12142389.

21. Jensen BV, Johansen JS, Price PA. High levels of serum HER-2/neu and YKL-40 independently reflect aggressiveness of metastatic breast cancer. Clin Cancer Res. 2003; 9:4423–4434. PMID: 14555515.
22. Colomer R, Llombart-Cussac A, Lluch A, Barnadas A, Ojeda B, Caranana V, et al. Biweekly paclitaxel plus gemcitabine in advanced breast cancer: phase II trial and predictive value of HER2 extracellular domain. Ann Oncol. 2004; 15:201–206. PMID: 14760109.

23. Pegram MD, Lipton A, Hayes DF, Weber BL, Baselga JM, Tripathy D, et al. Phase II study of receptor-enhanced chemosensitivity using recombinant humanized anti-p185HER2/neu monoclonal antibody plus cisplatin in patients with HER2/neu-overexpressing metastatic breast cancer refractory to chemotherapy treatment. J Clin Oncol. 1998; 16:2659–2671. PMID: 9704716.

24. Esteva FJ, Valero V, Booser D, Guerra LT, Murray JL, Pusztai L, et al. Phase II study of weekly docetaxel and trastuzumab for patients with HER-2-overexpressing metastatic breast cancer. J Clin Oncol. 2002; 20:1800–1808. PMID: 11919237.

25. Kostler WJ, Schwab B, Singer CF, Neumann R, Rucklinger E, Brodowicz T, et al. Monitoring of serum Her-2/neu predicts response and progression-free survival to trastuzumab-based treatment in patients with metastatic breast cancer. Clin Cancer Res. 2004; 10:1618–1624. PMID: 15014012.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download