Abstract
We have experienced three cases of extramammary Paget's disease (EMPD) of the vulva that received radiation therapy (RT). Here, we analyze the efficacy of RT and include a literature survey.
Three patients with EMPD of the vulva were treated with curative RT between 1993 and 1998. One of the patients had associated underlying adenocarcinoma of the vulva. The total doses of radiation administered were 54~78 Gy/6~8 weeks. Radiation fields encompassed 2 to 3 cm outer margins free from all visible disease including or not including the inguinal area using a 9 MeV electron or a 6 MV photon beam. Follow-up durations after radiotherapy were 0.6~11 years. Complete response was obtained in all three patients. Marginal failure occurred in one patient, and another patient with underlying adenocarcinoma treated by vulvectomy with bilateral inguinal lymph node dissection followed by external RT showed no relapse. Radiation induced side effects were transient acute confluent wet desquamation in the treated area resulting in mild late atrophic skin changes.
Although surgery is currently considered the preferred primary treatment for EMPD, it has a high relapse rate due to the multifocal nature of the disease. We conclude that RT is of benefit in some selected cases of EMPD.
Extramammary Paget's disease (EMPD) of the vulva is an uncommon malignant neoplasia with a high local recurrence rate and mainly affects aged postmenopausal women.
The standard treatment is local excision of the affected area with adequate margins; however, 40~45% of cases recur after surgery within 4 years (1). Cryosurgery, topical 5-fluorouracil (5-FU) alone and systemic chemotherapy (mitomycin C and 5-FU) have also been employed as primary treatments (2,3).
EMPD usually affects the elderly who may be medically unfit for surgery, and the treatment of genital lesions may involve mutilating surgery. However, more recently radiation therapy (RT) has been considered as an appropriate primary or adjuvant treatment with curative intent, in those who are medically unfit for surgery or in whom other modalities are inappropriate.
We retrospectively reviewed the clinical records of three patients with EMPD of the vulva that were treated by local external RT between 1993 and 1998 at our department, and undertook a review of the literature.
A 78-year-old woman with hypertension was referred because of a 5-year history of a pruritic, painful, and persistent erythematous lesion in the vulva; 16 years previously she had received a vulvectomy for EMPD. Multiple topical treatments had been attempted without improvement. On examination, the lesion was observed as poorly defined infiltrated 5×6 cm sized erythematous plaque with some ulceration on the vulva, which extended to the upper medial thigh (Fig. 1). No regional lymphadenopathies and no systemic diseases were detected.
External RT was administered using AP/PA two opposing fields of 6 MV photons at 180 cGy per day, 5 times per week, up to a total dose of 5,580 cGy. The initially treated irradiation field size was 10×11 cm and this was reduced to 8×8 cm after 5,040 cGy. The irradiation field encompassed 2 to 3 cm outer margins free from all visible disease.
Following RT, she showed an almost normal skin and mucosal appearance in the genital area, although she had experienced temporary radiation-induced skin reactions toward the end of the RT, which completely resolved within 2~3 months after RT. A two year post-RT follow-up documented local relapse at the mucocutaneous junction of the genital area, and repeated skin biopsies have revealed the same disease. However, no further treatment has been administered becaue of tolerable symptoms and signs.
A 69-year-old woman was referred for postoperative adjuvant RT. She had suffered from pruritus and pain on the left labium of the vulva for 6 years and had a slowly growing small palpable nodule in the left inguinal area of duration 2 years, which had been treated with topical treatments at another hospital without improvement. Based on biopsy results, she was diagnosed as having EMPD of the vulva with underlying adenocarcinoma in left inguinal lymph node. She underwent a wide local excision with bilateral lymph node dissection. Genitourinary and gastrointestinal neoplasms were excluded by abdominopelvic CT scan and endoscopy.
External RT was administered using AP/PA fields of 6 MV photons at 170 cGy per day, 5 times per week, up to a total dose of 5,440 cGy. RT fields included both inguinal nodes. A 1 cm bolus was applied at both inguinal areas. The initial field size of RT was 22×20 cm followed by a reduction to 16×20 cm after 5,040 cGy.
Following RT, she developed mild late atrophic skin changes. However, no local relapses developed during an 8 years follow-up period. She later developed and received an operation for a cranial meningioma after 8 years. Her general condition at present is satisfactory.
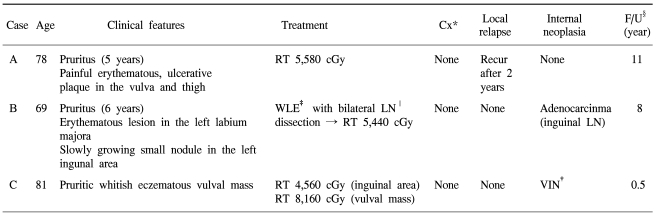
An 81-year-old woman was referred to our department because of a pruritic whitish eczematous right side vulval mass. Biopsies showed findings of invasive Paget's disease of the vulva and vaginal intraepithelial neoplasia (Fig. 2A). Pelvic CT revealed left inguinal lymphadenopathy and other unremarkable findings. No other systemic disease was detected.
External RT was applied using 6 MV photons at 170~180 cGy per day, 5 times per week, up to a total dose of 4,560 cGy to the whole pelvis including both inguinal areas. The initial field size was 26×22 cm and this was later reduced to 16×21 cm after 3,000 cGy. Another 3,600 cGy was added using 9 MeV electrons with a 10 cm cone to the vulvar mass area. During RT transient wet desquamation around the perineal region developed but spontaneously healed.
This patient showed clinically complete remission at her 6 month follow-up (Fig. 2B).
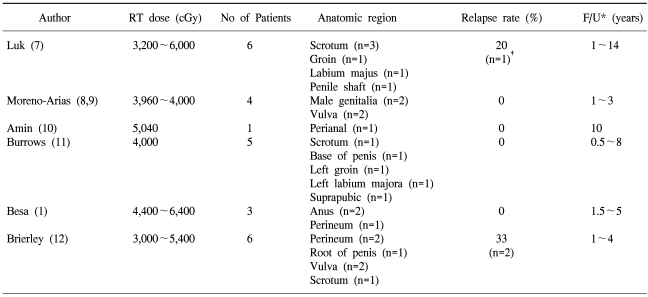
All treated 3 cases are summarized in Table 1.
Tissue diagnosis was made in all three cases by skin biopsy. Specimens were embedded in paraffin and histologic specimens were prepared for H&E, periodic acid Schiff (PAS), S-100 protein, carcinoembryonic antigen (CEA), cytokeratins, vimentin, and alcian blue staining (Fig. 3).
James Paget first described mammary Paget's disease in 1874, and EMPD was first described by Crocker in 1888 (4). EMPD is a rare disorder that frequently affects the anogenital area in the elderly. The most frequent site is the vulva followed by the perianal region, pelvis, scrotum, penis, and groin (5).
EMPD is a rare disorder which occurs more commonly in women than in men, and more frequently between the ages of 50 and 80 years. Paget's disease of the nipple is always associated with a subjacent breast adenocarcinoma, but this relation is less frequent in EMPD. In a review of 196 cases of EMPD between 1962 and 1982, 24% of the patients had an associated adnexal carcinoma, but only 12% had a concomitant internal malignancy (5).
Histopathologically Pagetoid cells, which have large round nuclei and abundant pale-staining cytoplasm, are located in the basal epidermis and rarely protrude into the dermis. However, in some cases cells do invade the dermis, a condition which could be defined as invasive Paget's disease, which has a poor prognosis (2).
The clinical features of Paget's disease include erythematous, scaly, pruritic, ulcerative areas, and local pain. Lesions vary in color from an erythematous to a whitish gray. These features are similar to those of Paget's disease of the nipple, and may resemble atopic eczema or contact dermatitis. Consequently skin biopsy is important diagnostic tool. Moreover, symptom durations in our three cases were protracted, and all had a history of multiple topical medications without improvement, which is typical in elderly women.
Local surgical excision with wide margins is considered the treatment of choice by many. Moreover, excision of the rectum or abdominoperineal resection may be required in patients with invasive disease or associated adenocarcinoma.
In 36~66% of cases, resection margins were reported to be positive after surgical resection alone with a local recurrence rate of up to 40~45% within 4 years (1). To reduce the risk of local recurrence, intraoperative margin checks using frozen sections or Moh's chemosurgery have been used (6).
However, because of the multifocal nature of EMPD, surgery is limited from the prognostic point of view, and is sometimes associated with severe morbidity and functional impairment. Thus, RT has been used in certain conditions, such as, in aged patients that are medically unfit for surgery, or as an alternative therapy for those with recurrence after repeated operations and for those who refuse surgery. Complete regression has been achieved after local RT, and recent reports indicate that more than 80% of cases show no recurrence after long-term follow-up (Table 2).
In our series, one patient diagnosed as having EMPD of the vulva with underlying adenocarcinoma in the inguinal area, received wide local excision followed by postoperative RT some 8 years ago and remains disease free.
In terms of RT, photon or electron beams can be used. Appropriate electron beam energies can spare deeper structures, but when the disease is associated with an adjacent adenocarcinoma the use of a photon beam is recommended. Though, optimal radiation doses have not been definitively determined, many authors recommend 40~50 Gy in intraepithelial Paget's disease and 55~65 Gy in invasive Paget's disease or EMPD with associated adenocarcinoma. The morbidity associated with radiotherapy is minimal. In our cases, no specific chronic complication occurred, only acute transient radiation-induced skin reactions. Moreover, at the time of RT planning, the use of topical 5-FU was found to be useful in terms of defining disease extent (3).
Because Paget's disease is rare, no randomized trials have been performed, and thus it is difficult to compare the efficacies of surgical resection and RT. To determine the efficacy of RT long-term follow-up and randomized study is mandatory. However, primary or postoperative adjuvant RT in selected patients with EMPD should be viewed as highly effective treatment modalities.
References
1. Besa P, Rich TA, Delclos L, Edwards CL, Ota DM, Wharton JT. Extramammary Paget's disease of the perineal skin: role of radiotherapy. Int J Radiat Oncol Biol Phys. 1992; 24:73–78. PMID: 1324902.

2. Parker LP, Parker JR, Bodurka-Bevers D, Deavers M, Bevers MW, Shen-Gunther J, et al. Paget's disease of the vulva: pathology, pattern of involvement, and prognosis. Gynecol Oncol. 2000; 77:183–189. PMID: 10739709.

3. Eliezri YD, Silvers DN, Horan DB. Role of preoperative topical 5-fluorouracil in preparation for Mohs micrographic surgery of extramammary Paget's disease. J Am Acad Dermatol. 1987; 17:497–505. PMID: 2821087.

4. Crocker HR. Paget's disease affecting the scrotum and penis. Trans Pathol Soc London. 1889; 40:187–191.
5. Chanda JJ. Extramammary Paget's disease: prognosis and relationship to internal malignancy. J Am Acad Dermatol. 1985; 13:1009–1014. PMID: 3001158.

6. Coldiron BM, Goldsmith BA, Robinson JK. Surgical treatment of extramammary Paget's disease. A report of six cases and a reexamination of Mohs micrographic surgery compared with conventional surgical excision. Cancer. 1991; 67:933–938. PMID: 1846769.

7. Luk NM, Yu KH, Yeung WK, Choi CL, Teo ML. Extramammary Paget's disease: outcome of radiotherapy with curative intent. Clin Exp Dermatol. 2003; 28:360–363. PMID: 12823291.

8. Moreno-Arias GA, Conill C, Sola-Casas MA, Mascaro-Galy JM, Grimalt R. Radiotherapy for in situ extramammary Paget disease of the vulva. J Dermatolog Treat. 2003; 14:119–123. PMID: 12775320.

9. Moreno-Arias GA, Conill C, Castells-Mas A, Arenas M, Grimalt R. Radiotherapy for genital extramammary Paget's disease in situ. Dermatol Surg. 2001; 27:587–590. PMID: 11442599.

11. Burrows NP, Jones DH, Hudson PM, Pye RJ. Treatment of extramammary Paget's disease by radiotherapy. Br J Dermatol. 1995; 132:970–972. PMID: 7662577.

Fig. 1
Case A. A 78-year-old woman was referred because of a 5-year history of a pruritic, painful, and persistent erythematous lesion in the vulva; 16 years previously she had undertaken a vulvectomy for the same disease. It shows poorly defined infiltrated 5×6 cm sized erythematous plaque with some ulceration on the vulva which extended to the upper medial thigh.

Fig. 2
Case C. (A) A 81-year-old woman was referred because of pruritic whitish eczematous vulva lesions with palpable mass. Biopsies showed findings of invasive Paget's disease of the vulva and vaginal intraepithelial neoplasia. (B) After radiation therapy, she showed clinically complete remission.
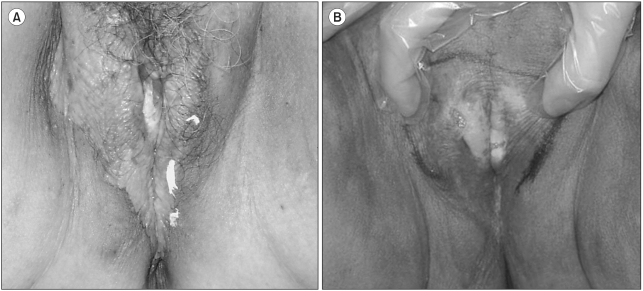
Fig. 3
(A) Microscpic findings of the biopsy from the vulva show that large, pale and vacuolated cells are clustered just above the basal layer (H/E, ×100), (B) They show that pargetoid cells (⇩) are single, or arranged in rows or nests. They show abundant cytoplasm, round nuclei and prominent nucleoli, occasionally with mitosis (H/E, ×400).





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download