Abstract
Purpose
The first Korean national population-based cancer registry using nationwide hospital-based recording system and the regional cancer registries provided the source to obtain national cancer incidences for the period 1999~2001.
Materials and Methods
The incidence of cancer in Korea was calculated based on the Korea Central Cancer Registry database, data from additional medical record review survey, the Regional Cancer Registry databases, site-specific cancer registry databases, and cancer mortality data from the Korea National Statistical Office. Crude and age-standardized rates were calculated by sex for 18 age groups.
Results
The overall crude incidence rates (CR) were 247.3 and 188.3 per 100,000 for men and women and the overall age-standardized incidence rates (ASR) were 281.2 and 160.3 per 100,000, respectively. Among men, five leading primary cancer sites were stomach (CR 58.6, ASR 65.6), lung (CR 42.1, ASR 50.9), liver (CR 41.9, ASR 44.9), colon and rectum (CR 24.2, ASR 27.3) and bladder (CR 7.7, ASR 9.2). Among women, the most common cancers were stomach (CR 30.8, ASR 25.8), breast (CR 25.7, ASR 21.7), colon and rectum (CR 19.6, ASR 16.7), uterine cervix (CR 18.4, ASR 15.5), and lung cancer (CR 15.1, ASR 12.4). In 0~14 age group, leukemia was most common for both sexes. For men, stomach cancer was most common in 15~64 age group, but lung cancer was more frequent for over 65 age group. For women, thyroid cancer in 15~34 age group, breast cancer in 35~64 age group, and stomach cancer in over 65 age group were most common for each age group. The proportions of death certificate only were 7.5% for men and 7.4% for women.
In order to determine the current magnitude of the cancer burden, cancer registration is an essential component for the planning and monitoring of a national cancer control program. The Korean Ministry of Health and Welfare started a nationwide, hospital-based cancer registry (Korea Central Cancer Registry, KCCR) in 1980 (1). The KCCR database is especially useful for showing trends of cancer occurrence in Korea. Many attempts have been made to collect data on the incidences of cancer from reliable registries in Korea. Population-based cancer registries provide valid estimates on the incidences of cancer in defined populations. Population-based regional cancer registry (PB-RCR) programs have been established one by one; Seoul in 1991, Busan in 1995, Daegu and Gwangju in 1997, Incheon in 1998, Daejeon in 1999, Ulsan and Jeju Island in 2001 and Goyang in 2002. These regional registries have been collaborating with the KCCR which is providing financial and technical support. Cancer incidence rates in Korea were first estimated using the data from 4 regional cancer registries that published their data in vol. VIII of Cancer Incidence in Five Continents in 2002 (2).
Since 2002, the KCCR has constructed the Korea National Cancer Incidence Data Bases (KNCIDB) by merging the KCCR mother DB and all 9 PB-RCR databases, the site-specific cancer registry databases (breast, ovary, cervix, liver cancer etc), data from the additional medical record review survey and the cancer mortality database from the National Statistical Office (NSO) (3). The aim of this paper is to present the cancer incidences during 1999~2001 as the first result based on the KNCIDB.
The KCCR identified incident form of cancer cases in Korea through the nationwide hospital-based discharge recording system using the International Classification of Disease for Oncology (ICD-O, 3rd edition) (4,5). This hospital-based database covers all general hospitals in Korea that are equipped with a histo-pathology laboratory. The collection of information was largely passive. Cases were identified through a personal identification number and other usual identification variables such as names and addresses. The list of KCCR-registered cases and a list of cancer cases from claims made through the National Health Insurance Corporation (NHIC) for each region were sent to the regional cancer registries to find dropped cases. The data collection methods of regional cancer registries were both passive and active.
Starting in 2002, the KCCR has constructed the Korea National Cancer Incidence DataBases (KNCIDB) by merging the KCCR mother DB, all 9 PB-RCR databases, and the site-specific cancer registry databases (breast, ovary, cervix, liver cancer etc). The KNCIDB was further refined by confirming multiple primary cancers according to the rules provided by the International Agency for Research on Cancer (IARC); only one tumor per organ or pair of organs per person per lifetime is reportable (2). Other duplicated cases were removed with the help of experts from a variety of fields such as clinicians, pathologists and medical record administrators.
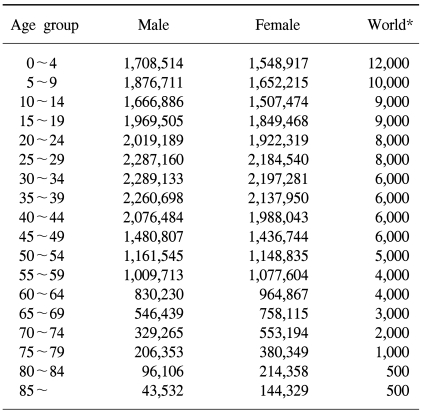
From 2002 to 2004, we compared the KNCIDB data with the list of claimed cancer cases from the NHIC; the list of cancer patients who were newly diagnosed during 1999~2002, and did not visit the clinics for cancer during the past three years were identified. We reviewed the case reported in 2002 to include cases, which were diagnosed during 1999~2001, but their reports were delayed. A total of 740 hospitals including 166 KCCR-registered hospitals provided the data and 66,704 cases from the NHIC DB during 1999~2002 that were not included in the KNCIDB were investigated by active review of medical records to confirm the cause of death, the available details of the cancer (morphology, topography, etc), and the date of onset with the help of regional cancer registries and medical record administrators. A total of 29,794 cases were confirmed as malignant cases and added to the KNCIDB. Death certificates were also reviewed as an alternative source of information. The cases whose cause of death was cancer during 1999~2002 were matched to cases registered in the KNCIDB and 23,192 cases were added to the dataset. In total, 310,715 cases of cancer were included in the final dataset. The crude incidence rates (CR) per 100,000 by sex were calculated for 18 age groups (0~4, 5~9, 10~14, every five year, 85 years and over) and standardized to the World Standard Population of the World Health Organization (WHO) (6).
The population used as the denominator to calculate cancer incidences is a mid-year population (the population on the 1st of July). However, in this report, the modified resident registration population data that is released annually from the NSO was used (3).
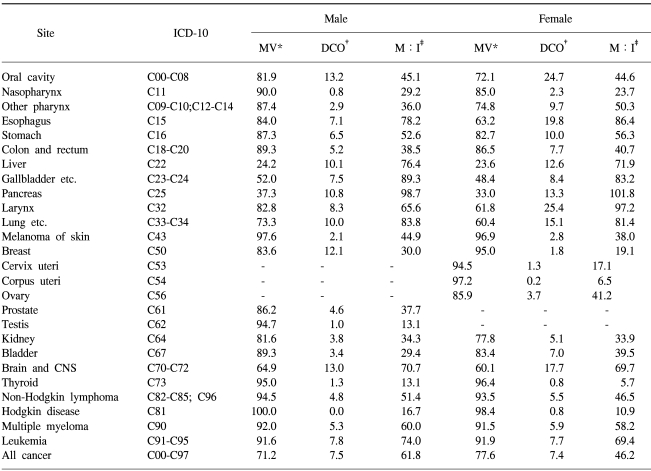
We calculated several indices of quality (7). For mortality: incidence ratio (M : I), an indicator of data completeness, the mortality data on cancer by sex, age group and site for the same period as the registered cases from the NSO were compared to the incidence data from the registry which was presented in percent. The microscopic verification % (MV%), an indicator of the validity of the diagnostic information, is the percentage of cases for which the diagnosis was based on morphological verification of a tissue specimen. The Death Certificate Only % (DCO%), percentage of cases that are registered on the basis of death certificates only is one of the indices of validity of diagnosis. Primary site unknown (PSU%) and Age unknown (Age UNK%) are the percentages of cases registered with unknown primary sites or unknown age, respectively.
Cumulative risk is the proportion of initially susceptible individuals in a population who become incident cases during a specified time period, in the absence of other competing causes of death. Cumulative risk could be derived from the cumulative rate, which is the summation of each age-specific rates over each year of age from birth to a defined upper age limit. In this report, we used 74 years old as an upper age limit.
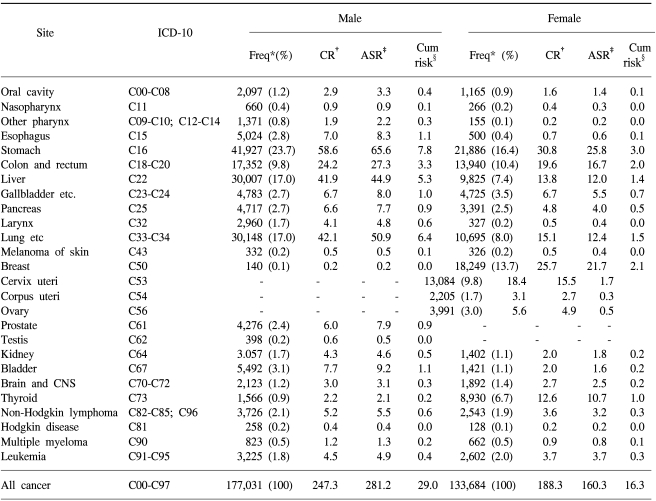
The overall CRs were 247.3 and 188.3 per 100,000 for men and women and the overall ASRs were 281.2 and 160.3 per 100,000, respectively. The overall cumulative risks for developing a cancer before the age of 74 were 29.0% for men and 16.3% for women (Table 1). In men, the five leading primary cancer sites were stomach (CR 58.6, ASR 65.6), lung (CR 42.1, ASR 50.9), liver (CR 41.9, ASR 44.9), colon and rectum (CR 24.2, ASR 27.3) and bladder (CR 7.7, ASR 9.2). In women, the most common cancer sites were stomach (CR 30.8, ASR 25.8), followed by breast (CR 25.7, ASR 21.7), colon and rectum (CR 19.6, ASR 16.7), uterine cervix (CR 18.4, ASR 15.5), and lung (CR 15.1, ASR 12.4).
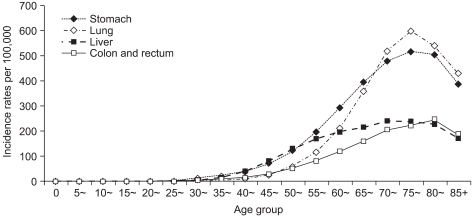
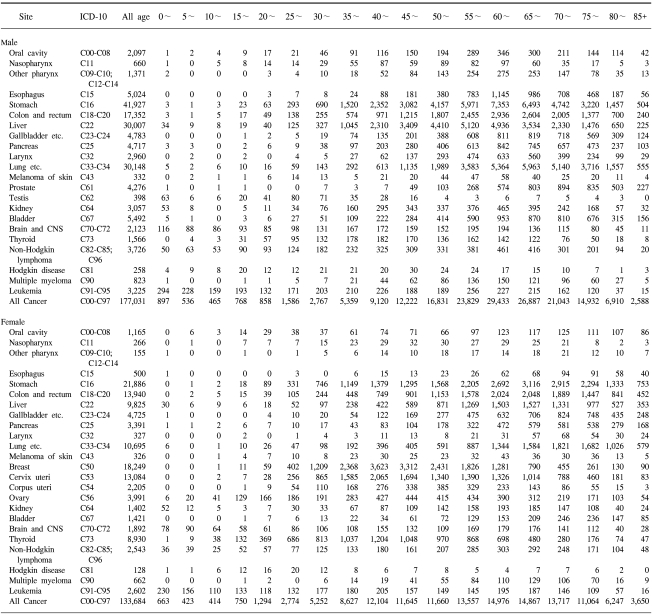
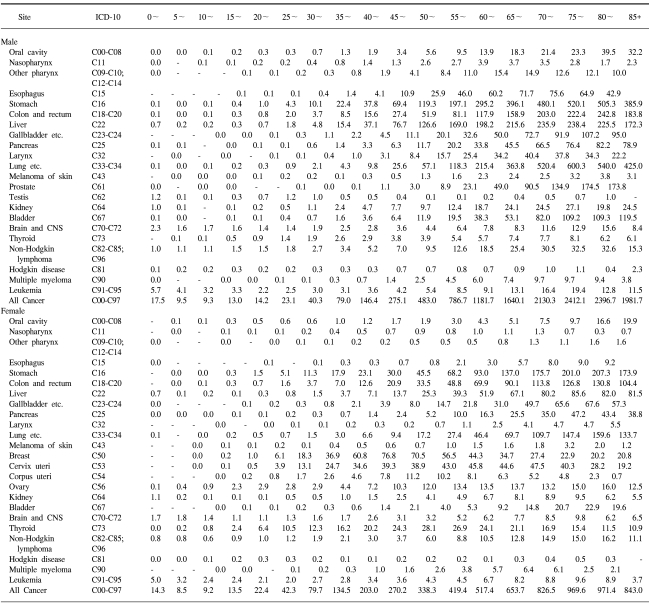
In the 0~14 age group, leukemia was most common in both sexes. For males, stomach cancer was most common in the 15~64 age group, but lung cancer was more frequent for the over 65 age group. For females, thyroid cancer for the 15~34 age group, breast cancer for the 35~64 group, and stomach cancer among the over 65 group were the most common forms of cancer for each age group (Table 2 and 3). Fig. 1 shows the age-specific incidence graph of the 4 major cancers in men. Fig. 2 shows an age-specific incidence graph of the 6 major cancers in women. The data shows that cancer incidence gradually increased with age, but there was some decline after 75 in men and 80 in women.
To assess the quality of the data in terms of completeness and validity, we examined several indices of quality (Table 4). The M : I ratios were 61.8% and 46.2% for men and women. We also evaluated the validity of the KNCIDB data using indices such as MV%, DCO%, PSU% and Age UNK%. The MV%s of the diagnosis were 71.2% and 77.6% for men and women. The DCO%s were 7.5% and 7.4% for men and women, respectively. The PSU%s were 2.2% and 2.5% for men and women. The Age UNK%s were 0% for both men and women.
The significance of this report lies in the fact that a nationwide cancer incidence report derived from 47 million people is unprecedented in the world.
Stomach, lung, liver, and colorectal cancer represent the four most common primary sites of cancer in Korea, accounting for two-thirds of the cancer burden in Korean men. Stomach, breast, colorectal, cervix, lung, and liver cancer account for two-thirds of cancer burden in Korean women.
Compared to the cancer incidence reported in the Globocan 2002 (8), the overall ASR in Korean men is higher than the world average (281.2 vs. 209.6 per 100,000 males) and is similar to that reported for northern Europe (283.1). By contrast, Korean women have an overall ASR similar to the world average (160.3 vs. 161.5 per 100,000 females) and lower than those reported for Europe. In addition, it is similar to that of Japan (167.4), eastern Africa (156.7), Caribbean (164.9) and Melanesia (165.0). In both sexes, ASRs of stomach, colon and rectum, liver, lung and thyroid cancer are higher than the world average ASR.
For most cancers, incidence increases with age. This increase begins after the age of 15. However, there is some decline after the age of 75 in men and 80 in women. This trend has been observed in the oldest age group in other cancer registries. It is partly due to less efficient case ascertainment, some of which is a consequence of competing causes of mortality in the elderly, and is partly because of a decrease in the proportion of the population predisposed to cancer (9).
To evaluate the validity of the results presented in this report, we compared the current findings with results from our previous report where we estimated cancer incidence in Korea. We used the estimated number of new cases in 1998~2000 based on the accumulated cancer registry data from Kanghwa, Seoul, Busan, and Daegu (2). The estimated overall ASR during 1998~2000 were 287.0 per 100,000 males and 163.1 per 100,000 females (10). These incidences were slightly different from those calculated (247.3 vs. 281.2 for males and 188.3 vs.160.3 for females) in this report. Compared to the rates from this report, the estimated ASRs for cancers that are decreasing, for example, stomach, liver and uterine cervix cancer, seemed to be over-estimated, while those with an increasing trend such as colo-rectum, lung and female breast cancers, tended to be under-estimated. This may suggest that the estimation of national incidence based on the regional cancer registry data does not reflect the rapidly changing trends or the effect of the cancer control programs during a specific period of time or in a specific geographical region.
It is essential to assess the quality of data for completeness and validity. We evaluated the completeness and the validity of the KNCIDB using the indices such as DCO%, M : I ratio, MV%, PSU% and Age UNK%. All the values for these indices were within the expected ranges based on the regional standard in the Cancer Incidence in Five Continents, Volume VIII. The standards for DCO% from the North American Association of Central Cancer Registries (11) is less than 5% for silver standard and that of the Canadian Cancer Registry (12) is less than 5% for acceptable. And DCO% higher than 15% was considered to be due to probable under-reporting (7). Conversely, a very low DCO% (under 1%) might mean that not all of the death certificates with diagnosis of cancer have reached the registry. According to these rules, DCO% in this report (7.5% for men, 7.4% for women) is quite acceptable. PSU% of the KNCIDB (2.2% for men and 2.5% for women) is acceptable by the standards of Canadian Cancer Registry (0~8%) and relatively low compared to those of most countries (2,12). For the Age UNK%, which rarely exceeds 1% in developed countries, there was no case with unknown age in our data.
Considering the magnitude of the incident cancer cases during 1999~2001 (annually 100,236 cases) and cancer mortality (3), cancer is currently the most important public health problem in Korea, and the ageing of the Korean population will cause these numbers to continue to increase even if age-specific rates remain constant.
The cancer incidences presented in this report can be used as reference information to evaluate the effect of various cancer control interventions. And the publication of this report will prompt more research that will help identify risk factors associated with the observed increases in Korean population.
ACKNOWLEDGEMENT
The authors owed a debt of gratitude to KCCR-affiliated Hospitals, and non KCCR-affiliated Hospitals and staff members for Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, Ulsan, and Jeju-do Cancer Registry.
References
1. Cancer registry system in Korea. Korea Central Cancer Registry. Available from:
http://www.ncc.re.kr.
2. Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB, editors. Cancer Incidence in Five Continents. 2002. Vol. VIII. Lyon: IARC Press;IARC Scientific Publications No. 155.
3. Korean Statistical Information System. National Statistical Office, Korea. Available from:
http://kosis.nso.go.kr.
4. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, editors. International Classification of Disease for Oncology. 2000. 3rd ed. Geneva: World Health Organization.
5. Korea Central Cancer Registry International Classification of Diseases for Oncology. 2003. 3rd ed. Goyang: National Cancer Center;(Korean version).
6. Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: New WHO standard. 2000. Geneva: World Health Organization;GPE Discussion paper series No.31.
7. Jensen OM, Parkin DM, Maclennan R, Muir CS, Skeet RG, editors. Cancer Registration Principles and methods. 1991. Lyon: IARC;IARC Scientific Publication No 95.
8. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108. PMID: 15761078.

9. Parkin DM, Chen VW, Ferlay J, Galceran J, Storm HH, Whelan SL. Comparability and quality control in cancer registration. 1994. International Agency for Research on Cancer;IARC technical report No.19.
10. Shin HR, Ahn YO, Bae JM, Shin MH, Lee DH, Lee CW, et al. Cancer incidence in Korea. Cancer Res Treat. 2002; 34:405–408.

11. Havener LA, editor. Standards for Cancer Registries Volume III: Standards for Completeness, Quality, Analysis, and Management of data. 2004. North American Association of Central Cancer Registries, Inc.
12. Cormier M. User guide to data quality reports for provincial/Territorial Cancer Registries. 2005.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download