1. Burkitt DA. Sarcoma involving the jaws in Africa children. Br J Surg. 1958; 45:218–223. PMID:
13628987.
2. Epstein MA, Achong BG, Barr YM. Virus particles in cultured lymphoblasts from Burkitt's lymphoma. Lancet. 1964; 1:702–703. PMID:
14107961.

3. Henle G, Henle W, Diehl V. Relation of Burkitt's tumor-associated herpes-type virus to infectious mononucleosis. Proc Natl Acad Sci USA. 1968; 59:94–101. PMID:
5242134.
4. International Agency for Research on Cancer. Epstein-Barr virus and Kaposi's sarcoma Herpesvirus/Human Herpesvirus 8. 1997. vol 70. Leon: WHO.
5. Raab-Traub N, Flynn K, Pearson G. The differentiated form of nasopharyngeal carcinoma contains Epstein-Barr virus DNA. Int J Cancer. 1987; 39:25–29. PMID:
3025109.

6. Weiss LM, Strickler JG, Warnke RA, Purtilo DT, Sklar J. Epstein-Barr viral DNA in tissues of Hodgkin's disease. Am J Pathol. 1987; 192:86–91. PMID:
2821817.
7. Jones JF, Shurin S, Abramowsky C, Tubbs RR, Sciotto CG, Wahl R, et al. T-cell lymphomas containing Epstein-Barr viral DNA in patients with chronic Epstein-Barr virus infections. N Engl J Med. 1988; 318:733–741. PMID:
2831453.

8. Burke AP, Yen TSB, Shekitka KM, Sobin LH. Lymphoepithelial carcinoma of the stomach with Epstein-Barr virus demonstrated by polymerase chain reaction. Mod Pathol. 1990; 3:377–380. PMID:
2163534.
9. Bonnet M, Guinebretiere JM, Kremmer E, Grunewald V, Benhamou E, Contesso G, Joab I. Detection of Epstein-Barr virus in invasive breast cancers. J Natl Cancer Inst. 1990; 91:1376–1381. PMID:
10451442.

10. Labrecque LG, Barnes DM, Fentiman IS, Griffin BE. Epstein-Barr virus in epithelial cell tumors: a breast cancer study. Cancer Res. 1995; 55:39–45. PMID:
7805038.
11. Sugawara Y, Mizugaki Y, Uchida T, Torii T, Imai S, Makuuchi M, et al. Detection of Epstein-Barr virus (EBV) in hepatocellular carcinoma tissue: a novel EBV latency characterized by the absence of EBV-associated small RNA expression. Virology. 1999; 256:196–202. PMID:
10191184.
12. Kieff E, Rickinson AB. Fields BN, Knipe DM, Howley P, editors. Epstein-Barr virus and its replication. Fields virology. 2001. 4th ed. Philadelpia: Lippincott-Raven publishers;p. 2511–2573.
13. Ambinder RF. Gammaherpesviruses and "Hit-and-Run" oncogenesis. Am J Pathol. 2000; 156:1–3. PMID:
10623645.

14. Staratschek-Jox A, Kotkowski S, Belge G, Rudiger T, Bullerdiek J, Diehl V, Wolf J. Detection of Epstein-Barr virus in Hodgkin-Reed-Sternberg cells: no evidence for the persistence of integrated viral fragments in Latent membrane protein-1 (LMP-1)-negative classical Hodgkin's disease. Am J Pathol. 2000; 156:209–216. PMID:
10623669.
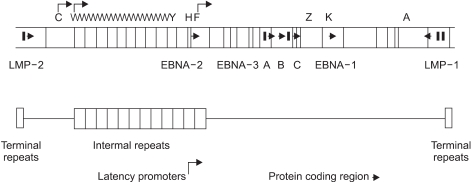
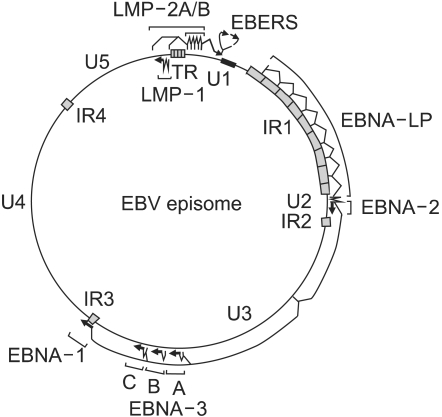
15. Baer R, Banker AT, Biggin MD. DNA sequence and expression of the B95-8 Epstein-Barr virus genome. Nature. 1984; 310:207–211. PMID:
6087149.

16. Raab-Traub N, Flynn K. The structure of the termini of the Epstein-Barr virus as a marker of clonal cellular proliferation. Cell. 1986; 47:883–889. PMID:
3022942.

17. Miller G. The Switch between latency and replication of Epstein-Barr virus. J Infec Dis. 1990; 161:833–844. PMID:
2157769.

18. Nemerow GR, Mold C, Schwend VK, Tollefson V, Cooper NR. Identification of gp350 as the viral glycoprotein mediating attachment of Epstein-Barr virus (EBV) to the EBV/C3d receptor of B cells: sequence homology of gp350 and C3 complement fragment C3d. J Virol. 1987; 61:1416–1420. PMID:
3033269.

19. Borza CM, Hutt-Fletcher LM. Alternate replication in B cells and epithelial ells switches tropism of Epstein-Barr virus. Nature Med. 2002; 8:594–599. PMID:
12042810.
20. Sixbey JW, Nedrud JG, Raab-Traub N, Hanes RA, Pagano JS. Epstein-Barr virus replication in oropharyngeal epithelial cells. N Engl J Med. 1984; 310:1225–1230. PMID:
6323983.

21. Evans As. Clinical syndromes associated with EB virus infections. Ann Intern Med. 1972; 18:77–93.
22. Tosato G, Blaese RM. Epstein-Barr virus infection and immunoregulation in man. Adv Immunol. 1985; 37:99–149. PMID:
2988307.

23. Tang H, Matthes T, Carballido-Perrig N, Zubler RH, Kindler V. Differential induction of T cell cytokine mRNA in Epstein-Barr virus-transformed B cell clones: consititutive and inducible expression of interleukin-4 mRNA. Eur J Immunol. 1993; 23:899–903. PMID:
8384561.
24. Cohen JI, Lekstrom K. Epstein-Barr virus BARF1 protein is dispensable for B-cell transformation and inhibits alpha interferon secretion from mononuclear cells. J Virol. 1999; 73:7627–7632. PMID:
10438853.

25. Levitskaya J, Shapiro A, Leonchiks A, Ciehanover A, Masucci MG. Inhibition of ubiquitin/proteosome-dependent protein degradation by the Gly-Ala repeat domain of the Epstein-Barr virus nuclear antigen 1. Proc Natl Acad Sci USA. 1997; 94:12616–12621. PMID:
9356498.
26. Masucci MG. Epstein-Barr virus oncogenesis and the ubiquitin-proteasome system. Oncogene. 2004; 23:2107–2115. PMID:
15021898.

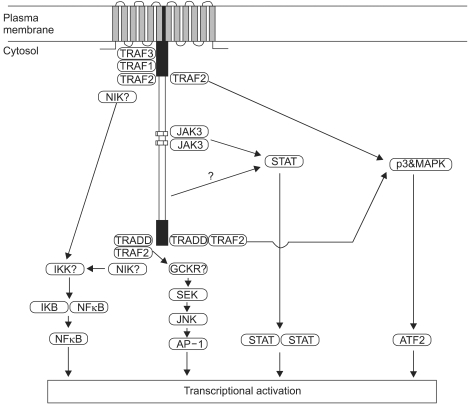
27. Wang D, Liebowitz D, Kieff E. An EBV membrane protein expressed in immortalized lymphocytes transforms established rodent cells. Cell. 1985; 43:831–840. PMID:
3000618.

28. Dawson CW, Rickinson AB, Young LS. Epstein-Barr virus latent membrane protein inhibits human epithelial cell differentiation. Nature. 1990; 344:777–780. PMID:
2158628.

29. Fahraeus R, Rymo L, Rhim JS, Klein G. Morphological transformation of human keratinocytes expressing the LMP gene of Epstein-Barr virus. Nature. 1990; 345:447–449. PMID:
1692971.
30. Kulwichit W, Edwards RH, Davenport EM, Baskar JF, Godfrey V, Raab-Traub N. Expression of the Epstein-Barr virus latent membrane protein 1 induces B cell lymphoma in transgenic mice. Proc Natl Acad Sci U S A. 1998; 95:11963–11968. PMID:
9751773.

31. Curran JA, Laverty FS, Campbell D, Macdiarmid J, Wilson JB. Epstein-Barr virus encoded latent membrane protein-1 induces epithelial cell proliferation and sensitizes transgenic mice to chemical carcinogenesis. Cancer Res. 2001; 61:6730–6738. PMID:
11559544.
32. Baumforth KR, Young LS, Flavell KJ, Constandinou C, Murray PG. The Epstein-Barr virus and its association with human cancers. Mol Pathol. 1999; 52:307–322. PMID:
10748864.

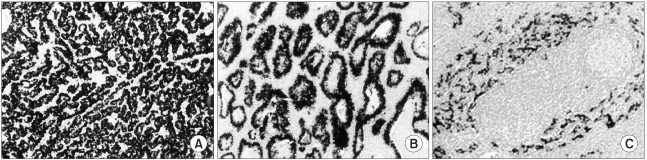
33. Cho YS, Chang MS, Park SH, Kim HS, Kim WH. In situ hybridization of Epstein-Barr virus in tumor cells and tumor-infiltrating lymphocytes of the gastrointestinal tract. Human Pathology. 2001; 32:297–301. PMID:
11274639.

34. Chang MS, Kim WH, Kim CW, Kim YI. Epstein-Barr virus in gastric carcinomas with lymphoid stroma. Histopathology. 2000; 37:309–315. PMID:
11012737.

35. Wu TC, Mann RB, Charache P, Hayward SD, Staal S, Lambe BC, et al. Detection of EBV gene expression in Reed-Sternberyg cells of Hodgkin's disease. Int J Cancer. 1990; 46:801–804. PMID:
2172169.
36. Barletta JM, Kingma DW, Charache P, Mann RB, Ambinder RF. Rapid in situ hybridization for the diagnosis of latent Epstein-Barr virus infection. Mol Cell Probes. 1993; 7:105–109. PMID:
8391639.

37. Chang MS, Lee JH, Kim JP, Kim HS, Lee HS, Kim CW. Microsatellite instability and Epstein-Barr virus infection in gastric remnant cancers. Pathol Int. 2000; 50:486–492. PMID:
10886725.

38. Chang MS, Lee HS, Kim HS, Kim YI, Kim WH. Clinicopathologic characteristics of Epstein-Barr virus-incorporated gastric cancers in Korea. Pathol Res Pract. 2001; 197:395–400. PMID:
11432666.

39. Chang MS, Kim HS, Kim CW, Kim YI, Lee BL, Kim WH. Epstein-Barr virus, p53 protein and microsatellite instability in adenoma-carcinoma sequence of the stomach. Hum Pathol. 2002; 33:415–420. PMID:
12055676.
40. Chang MS, Lee HS, Kim HS, Kim SH, Choi SI, Lee BL, et al. Epstein-Barr virus and microsatellite instability in gastric carcinogenesis. J Pathol. 2003; 199:447–452. PMID:
12635135.

41. Chang MS, Lee HS, Jung EJ, Kim CW, Lee BL, Kim WH. Cell cycle regulators, bcl-2 and NF-kB in Epstein-Barr virus-associated gastric carcinomas. Int J Oncol. (In print).

42. Murray PG, Niedobitek G, Kremmer E, Grasser F, Reynolds GM, Cruchiley A, et al. In situ detection of the Epstein-Barr virus-encoded nuclear antigen 1 in oral hairy leukoplakia and virus-associated carcinomas. J Pathol. 1996; 178:44–47. PMID:
8778314.

43. Cancer Registry system in Korea. Headquarters of Korea Central Cancer Registry. Available from: URL:
http://ncc.re.kr.
44. Fukayama M, Hayashi Y, Iwasaki Y, Chong J, Ooba T, Takizawa T, et al. Epstein-Barr virus-associated gastric carcinoma and Epstein-Barr virus infection of the stomach. Lab Invest. 1994; 71:73–81. PMID:
8041121.
45. Yanai H, Takada K, Shimizu N, Mizugaki Y, Tada M, Okita K. Epstein-Barr virus infection in non-carcinomatous gastric epithelium. J Pathol. 1997; 183:293–298. PMID:
9422984.

46. Gulley ML, Pulitzer DR, Eagan PA, Schneider BG. Epstein-Barr virus infection is an early event in gastric carcinogenesis and is independent of bcl-2 expression and p53 accumulation. Hum Pathol. 1996; 27:20–27. PMID:
8543306.

47. Imai S, Koizumi S, Sugiura M, Tokunaga M, Uemura Y, Yamamoto N, et al. Gstric carcinoma: Monoclonal epithelial malignant cells expressing Epstein-Barr virus latent infection protein. Proc Natl Acad Sci USA. 1994; 91:9131–9135. PMID:
8090780.
48. Levine PH, Stemmermann G, Lennette ET, Hildesheim A, Shibata D, Nomura A. Elevated antibody titers to Epstein-Barr virus prior to the diagnosis of Epstenin-Barr virus-associated gastric adenocarcinoma. Int J Cancer. 1995; 60:642–644. PMID:
7860138.
49. Osato T, Imai S. Epstein-Barr virus and gastric carcinoma. Semin Cancer Biol. 1996; 7:175–182. PMID:
8946601.

50. Shibata D, Weiss LM. Epstein-Barr virus-associated gastric adenocarcinoma. Am J Pathol. 1992; 140:769–774. PMID:
1314023.
51. Rawlands DC, Ito M, Mangham DC, Reynolds G, Hallissey MT, Fielding JW, et al. Epstein-Barr virus and carcinomas: rare association of the virus with gastric adenocarcinomas. Br J Cancer. 1993; 68:1014–1019. PMID:
8217590.

52. Tokunaga M, Land CE, Uemura Y, Tokudome T, Tanaka S, Sato E. Epstein-Barr virus in gastric carcinoma. Am J Pathol. 1993; 143:1250–1254. PMID:
8238241.
53. Shin WS, Kang MW, Kang JH, Choi MK, Ahn BM, Kim JK, et al. Epstein-Barr virus-associated gastric adenocarcinomas among Koreans. Am J Clin Pathol. 1996; 105:174–181. PMID:
8607441.

54. Nakamura S, Ueki T, Yao T, Ueyama T, Tsuneyoshi M. Epstein-Barr virus in gastric carcinoma with lymphoid stroma. Special Reference to its detection by the polymerase chain reaction and in situ hybridization in 99 tumors, including a morphological analysis. Cancer. 1994; 73:2239–2249. PMID:
8168030.
55. Mastsunou H, Konishi F, Hori H, Ikeda T, Sasaki K, Hirose Y, Yamamichi N. Characteristics of Epstein-Barr virus-associated gastric carcinoma with lymphoid stroma in Japan. Cancer. 1996; 77:1998–2004. PMID:
8640662.

56. Watanabe H, Enjoji M, Imai T. Gastric carcinoma with lymphoid stroma. Its morphologic characteristics and prognostic correlations. Cancer. 1976; 38:232–243. PMID:
947518.
57. Oda K, Tamaru J, Takenouchi T, Mikata A, Nunomura M, Saitoh N, et al. Association of Epstein-Barr virus with gastric carcinoma with lymphoid stroma. Am J Pathol. 1993; 143:1063–1071. PMID:
8214002.
58. Yamamoto N, Tokunaga M, Uemura Y, Tanaka S, Shirahama H, Nakamura T, et al. Epstein-Barr virus and gastric remnant cancer. Cancer. 1994; 74:805–809. PMID:
8039108.

59. Arikawa J, Tokunaga M, Satoh E, Tanakia S, Land CE. Morphological characterics of Epstein-Barr virus-related early gastric carcinoma: A case control study. Pathol Int. 1997; 47:360–367. PMID:
9211523.
60. Lee HS, Chang MS, Yang H-K, Lee BL, Kim WH. Epstein-barr virus-positive gastric carcinoma has a distinct protein expression profile in comparison to epstein-barr virus-negative carcinoma. Clin Cancer Res. 2004; 10:1698–1705. PMID:
15014022.
61. Hoshikawa Y, Satoh Y, Murakami M, Maeta M, Kaibara N, Ito H, et al. Evidence of lytic infection of Epstein-Barr virus (EBV) in EBV-positive gastric carcinoma. J Med Virol. 2002; 66:351–359. PMID:
11793387.

62. Luo B, Wang Y, Wang XF, Liang H, Yan LP, Huang BH, Zhao P. Expression of Epstein-Barr virus genes in EBV-associated gastric carcinomas. World J Gastroenterol. 2005; 11:629–633. PMID:
15655811.

63. Wei MX, Ooka T. A transforming function of the BARF1 gene encoded by Epstein-Barr virus. EMBO J. 1989; 8:2897–2903. PMID:
2555151.

64. Sheng W, Decaussin G, Sumner S, Ooka T. N-terminal domain of BARF1 gene encoded by Epstein-Barr virus is essential for malignant transformation of rodent fibroblasts and activation of Bcl-2. Oncogene. 2001; 20:1176–1185. PMID:
11313861.

65. Sheng W, Decaussin G, Ligout A, Takada K, Ooka T. Malignant transformation of Epstein-Barr virus-negative Akata cells by introduction of the BARF1 gene carried by Epstein-Barr virus. J Virol. 2003; 76:3859–3865. PMID:
12610162.

66. Zur Hausen A, Brink AA, Craanen ME, Middeldorp JM, Meijer CJ, van den Brule AJ. Unique transcription pattern of Epstein-Barr virus (EBV) in EBV-carrying gastric adenocarcinomas: expression of the transforming BARF1 gene. Cancer Res. 2000; 60:2745–2748. PMID:
10825150.
67. Fingeroth JD, Weiss JJ, Tedder TF, Strominger JL, Biro PA, Fearon DT. Epstein-Barr virus receptor of human B lymphocytes is the C3d receptor CR2. Proc Natl Acad Sci USA. 1984; 81:4510–4514. PMID:
6087328.

68. Sixbey JW, Yao QY. Immunoglobulin A-induced shift of Epstein-Barr virus tissue tropism. Science. 1992; 255:1578–1580. PMID:
1312750.

69. Bayliss GJ, Wolf H. Epstein-Barr virus-induced cell fusion. Nature. 1980; 287:164–165. PMID:
6253791.

70. Schneider BG, Gulley ML, Eagan P, Bravo JC, Mera R, Geradts J. Loss of p16/CDKN2A tumor suppressor protein in gastric adenocarcinoma is associated with Epstein-Barr virus and anatomic location in the body of the stomach. Hum Pathol. 2000; 31:45–50. PMID:
10665912.

71. Kang GH, Lee S, Kim WH, Lee HW, Kim JC, Rhyu MG, et al. Epstein-barr virus-positive gastric carcinoma demonstrates frequent aberrant methylation of multiple genes and constitutes CpG island methylator phenotype-positive gastric carcino. Am J Pathol. 2002; 160:787–794. PMID:
11891177.
72. Chong J-M, Fukayama M, Hayashi Y, Takizawa T, Koike M, Konishi M, et al. Microsatellite instability in the progression of gastric carcinoma. Cancer Res. 1994; 54:4595–4597. PMID:
8062248.
73. Leung SY, Yuen ST, Chung LP, Chu KM, Wong Mp, Rbanicki FJ, et al. Microsatellite instability, Epstein-Barr virus, mutation of type II transforming growth factor beta receptor and BAX in gastric carcinomas in Hong Kong Chinese. Br J Cancer. 1999; 79:582–588. PMID:
10027334.
74. Wu M-S, Shun C-T, Wu C-C, Hsu TY, Lin MT, Chang MC, et al. Epstein-Barr virus-associated gastric carcinomas: Relation to H. pylori infection and genetic alterations. Gastroenterology. 2000; 118:1031–1038. PMID:
10833477.

75. Boutell C, Everett R. The herpes simplex virus type 1 (HSV-1) regulatory protein ICP0 interacts with and Ubiquitinates p53. J Biol Chem. 2003; 278:36596–36602. PMID:
12855695.

76. Holowaty MN, Sheng Y, Nguyen T, Arrowsmith C, Frappier L. Protein interaction domains of the ubiquitin-specific protease, USP7/HAUSP. J Biol Chem. 2003; 278:47753–47761. PMID:
14506283.

77. Putnam DA. Antisense strategies and therapeutic applications. Am J Health Syst Pharm. 1996; 53:151–160. quiz 182-3. PMID:
8653480.
78. Coburn GA, Cullen BR. Potent and specific inhibition of human immunodeficiency virus type 1 replication by RNA interference. J Virol. 2002; 76:9225–9231. PMID:
12186906.

79. Jiang M, Milner J. Selective silencing of viral gene expression in HPV-positive human cervical carcinoma cells treated with siRNA, a primer of RNA interference. Oncogene. 2002; 21:6041–6048. PMID:
12203116.

80. Cahir-McFarland ED, Davidson DM, Schauer SL, Duong J, Kieff E. NFkB inhibition causes spontaneous apoptosis in Epstein-Barr virus-transformed lymphoblastoid cells. Proc Natl Acad Sci USA. 2000; 97:6055–6060. PMID:
10811897.
81. Farrell CJ, Lee JM, Shin EC, Cebrat M, Cole PA, Hayward SD. Inhibition of Epstein-Barr virus-induced growth proliferation by a nuclear antigen EBNA2-TAT peptide. Proc Natl Acad Sci USA. 2004; 101:4625–4630. PMID:
15070768.

82. Chodosh J, Holder VP, Gan YJ, Belgaumi A, Sample J, Sixbey JW. Eradication of latent Epstein-Barr virus by hydroxyurea alters the growth-transformed cell phenotype. J Infect Dis. 1998; 177:1194–1201. PMID:
9593003.

83. Dhar SK, Yoshida K, Machida Y, Khaira P, Chaudhuri B, Wohlschlegel JA, et al. Replication from oriP of Epstein-Barr virus requires human ORC and is inhibited by geminin. Cell. 2001; 106:287–296. PMID:
11509178.

84. Inman GJ, Bienne UK, Parker GA, Farrell PJ, Allday MJ. Activators of the Epstein-Barr virus lytic program concomitantly induce apoptosis, but lytic gene expression protects from cell death. J Virol. 2001; 75:2400–2410. PMID:
11160743.

85. Westphal EM, Blackstock W, Feng WH, Israel BF, Kenney SC. Activation of lytic Epstein-Barr virus (EBV) infection by radiation and sodium butyrate in vitro and in vivo: a potential method for treating EBV-positive malignancies. Cancer Res. 2000; 60:5781–5788. PMID:
11059774.
86. Aghi M, Kramm CM, Chou TC, Breakefield XO, Chiocca EA. Synergistic anticancer effects of ganciclovir/thymidine kinase and 5-fluorocytosine/cytosine deaminase gene therapies. J Natl Cancer Inst. 1998; 90:370–380. PMID:
9498487.

87. Gutierrez MI, Judde J, Magrath IT, Bhatia KG. Switching viral latency to viral lysis: A novel therapeutic approach for Epstein-Barr virus-associated neoplasia. Cancer Res. 1996; 56:969–972. PMID:
8640787.
88. Falk KI, Ernberg I. Demethylation of the Epstein-Barr virus origin of lytic replication and of the immediate early gene BZLF1 is DNA replication independent. Brief report. Arch Virol. 1999; 144:2219–2227. PMID:
10603176.
89. Gruffat H, Manet E, Sergeant A. MEF2-mediated recruitment of class II HDAC at the EBV immediate early gene BZLF1 links latency and chromatin remodeling. EMBO Rep. 2002; 3:141–146. PMID:
11818339.
90. Ben-Sasson SA, Klein G. Activation of the Epstein-Barr virus genome by 5-aza-cytidine in latently infected human lymphoid lines. Int J Cancer. 1981; 28:131–135. PMID:
6172387.
91. Rooney CM, Smith CA, Ng CY, Loftin SK, Sixbey JW, Gan Y, et al. Infusion of cytotoxic T cells for the prevention and treatment of Epstein-Barr virus-induced lymphoma in allogeneic transplant recipients. Blood. 1998; 92:1549–1555. PMID:
9716582.

92. Paludan C, Bickham K, Nikiforow S, Tsang ML, Goodman K, Hanekom WA, et al. Epstein-Barr nuclear antigen 1-specific CD4(+) Th1 cells kill Burkitt's lymphoma cells. J Immunol. 2002; 169:1593–1603. PMID:
12133989.
93. Rooney CM, Smith CA, Ng CY, Loftin S, Li C, Krance RA, et al. Use of gene-modified virus-specific T lymphocytes to control Epstein-Barr-virus-related lymphoproliferation. Lancet. 1995; 345:9–13. PMID:
7799740.

94. Murray RJ, Kurilla MG, Brooks JM, Thomas WA, Rowe M, Kieff E, et al. Identification of target antigens for the human cytotoxic T cell response to Epstein-Barr virus (EBV): impli cations for the immune control of EBV-positive malignancies. J Exp Med. 1992; 176:157–168. PMID:
1319456.
95. Chua D, Huang J, Zheng B, Lau SY, Luk W, Kwong DL, et al. Adoptive transfer of autologous Epstein-Barr virus-specific cytotoxic T cells for nasopharyngeal carcinoma. Int J Cancer. 2001; 94:73–80. PMID:
11668481.

96. Wagner HJ, Sili U, Gahn B, Vigouroux S, Huls MH, Xie W, et al. Expansion of EBV latent membrane protein 2a specific cytotoxic T cells for the adoptive immunotherapy of EBV latency type 2 malignancies: influence of recombinant IL12 and IL15. Cytotherapy. 2003; 5:231–240. PMID:
12850791.

97. Taylor GS, Haigh TA, Gudgeon NH, Phelps RJ, Lee SP, Steven NM, et al. Dual stimulation of Epstein-Barr virus (EBV)-specific CD4+/- and CD8+/- T cell responses by a chimeric antigen construct: Potential therapeutic vaccine for EBV-positive nasopharyngeal carcinoma. J Virol. 2004; 78:768–778. PMID:
14694109.
98. Bollard CM, Rossig C, Calonge MJ, Huls MH, Wagner HJ, Massague J, et al. Adapting a transforming growth factor beta-related tumor protection strategy to enhance antitumor immunity. Blood. 2002; 99:3179–3187. PMID:
11964281.
100. Ulaeto D, Wallace L, Morgan A, Morein B, Rickinson AB. In vitro T cell responses to a candidate Epstein-Barr virus vaccine: human CD4+ T cell clones specific for the major envelope glycoprotein gp340. Eur J Immunol. 1998; 18:1689–1697. PMID:
2904885.

101. Jung S, Chung YK, Chang SH, Kim J, Kim HR, Jang HS, et al. DNA-mediated immunization of glycoprotein 350 of Epstein-Barr virus induces the effective humoral and cellular immune responses against the antigen. Mol Cells. 2001; 12:41–49. PMID:
11561729.
102. Khanna R, Sherritt M, Burrows SR. EBV structural antigens, gp350 and gp85, as targets for ex vivo virus-specific CTL during acute infectious mononucleosis: potential use of gp350/gp85 CTL epitopes for vaccine design. J Immunol. 1999; 162:3063–3069. PMID:
10072559.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download