1. Zou Z, Anisowicz A, Hendrix MJ, Thor A, Neveu M, Sheng S, et al. Maspin, a serpin with tumor-suppressing activity in human mammary epithelial cells. Science. 1994; 263:526–529. PMID:
8290962.

2. Schneider SS, Schick C, Fish KE, Miller E, Pena JC, Treter SD, et al. A serine proteinase inhibitor locus at 18q21.3 contains a tandem duplication of the human squamous cell carcinoma antigen gene. Proc Natl Acad Sci USA. 1995; 92:3147–3151. PMID:
7724531.

3. Zhang M, Maass N, Magit D, Sager R. Transactivation through Ets and Ap1 transcription sites determines the expression of the tumor-suppressing gene maspin. Cell Growth Differ. 1997; 8:179–186. PMID:
9040939.
4. Sheng S, Carey J, Seftor EA, Dias L, Hendrix MJ, Sager R. Maspin acts at the cell membrane to inhibit invasion and motility of mammary and prostatic cancer cells. Proc Natl Acad Sci USA. 1996; 93:11669–11674. PMID:
8876194.

5. Sheng S, Pemberton PA, Sager R. Production, purification, and characterization of recombinant maspin proteins. J Biol Chem. 1994; 269:30988–30993. PMID:
7983035.

6. Sheng S, Truong B, Fredrickson D, Wu R, Pardee AB, Sager R. Tissue-type plasminogen activator is a target of the tumor suppressor gene maspin. Proc Natl Acad Sci USA. 1998; 95:499–504. PMID:
9435220.

7. Maass N, Hojo T, Ueding M, Luttges J, Kloppel G, Jonat W, et al. Expression of the tumor suppressor gene Maspin in human pancreatic cancers. Clin Cancer Res. 2001; 7:812–817. PMID:
11309327.
8. Lim YJ, Lee JK, Jang WY, Song SY, Lee KT, Paik SW, et al. Prognostic significance of maspin in pancreatic ductal adeno carcinoma. Korean J Intern Med. 2004; 19:15–18. PMID:
15053038.
9. Sood AK, Fletcher MS, Gruman LM, Coffin JE, Jabbari S, Khalkhali-Ellis Z, et al. The paradoxical expression of maspin in ovarian carcinoma. Clin Cancer Res. 2002; 8:2924–2932. PMID:
12231537.
10. Ogasawara S, Maesawa C, Yamamoto M, Akiyama Y, Wada K, Fujisawa K, et al. Disruption of cell-type-specific methylation at the Maspin gene promoter is frequently involved in undifferentiated thyroid cancers. Oncogene. 2004; 23:1117–1124. PMID:
14743202.

11. Umekita Y, Ohi Y, Sagara Y, Yoshida H. Expression of maspin predicts poor prognosis in breast-cancer patients. Int J Cancer. 2002; 100:452–455. PMID:
12115529.

12. Wada K, Maesawa C, Akasaka T, Masuda T. Aberrant expression of the maspin gene associated with epigenetic modification in melanoma cells. J Invest Dermatol. 2004; 122:805–811. PMID:
15086568.

13. Umekita Y, Yoshida H. Expression of maspin is up-regulated during the progression of mammary ductal carcinoma. Histopathology. 2003; 42:541–545. PMID:
12786889.

14. Futscher BW, Oshiro MM, Wozniak RJ, Holtan N, Hanigan CL, Duan H, et al. Role for DNA methylation in the control of cell type specific maspin expression. Nat Genet. 2002; 31:175–179. PMID:
12021783.
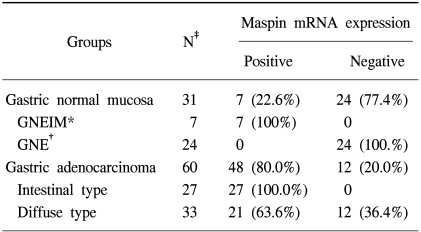
15. Akiyama Y, Maesawa C, Ogasawara S, Terashima M, Masuda T. Cell-type-specific repression of the maspin gene is disrupted frequently by demethylation at the promoter region in gastric intestinal metaplasia and cancer cells. Am J Pathol. 2003; 163:1911–1919. PMID:
14578190.

16. Son HJ, Sohn TS, Song SY, Lee JH, Rhee JC. Maspin expression in human gastric adenocarcinoma. Pathol Int. 2002; 52:508–513. PMID:
12366809.

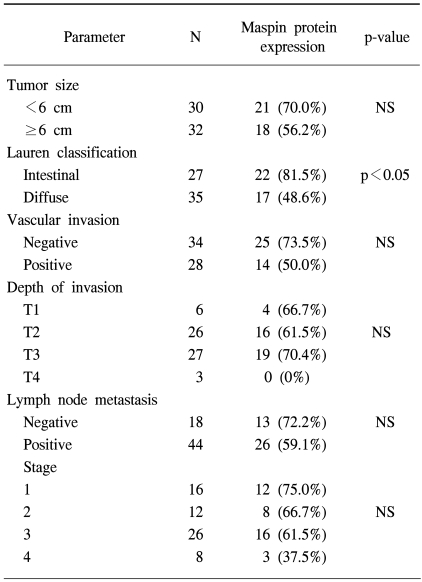
17. Terashima M, Maesawa C, Oyama K, Ohtani S, Akiyama Y, Ogasawara S, et al. Gene expression profiles in human gastric cancer: expression of maspin correlates with lymph node metastasis. Br J Cancer. 2005; 92:1130–1136. PMID:
15770218.

18. Wang MC, Yang YM, Li XH, Dong F, Li Y. Maspin expression and its clinicopathological significance in tumorigenesis and progression of gastric cancer. World J Gastroenterol. 2004; 10:634–637. PMID:
14991928.

19. Fleming I, Cooper J, Henson D. Stomach. AJCC cancer staging manual. 1997. 5th ed. Philadelphia: Lippincott-Raven;p. 71–76.
20. Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965; 64:31–49. PMID:
14320675.
21. Song SY, Lee SK, Kim DH, Son HJ, Kim HJ, Lim YJ, et al. Expression of maspin in colon cancers: its relationship with p53 expression and microvessel density. Dig Dis Sci. 2002; 47:1831–1835. PMID:
12184537.
22. Yin T, Ji XL, Shen MS. Relationship between lymph node sinuses with blood and lymphatic metastasis of gastric cancer. World J Gastroenterol. 2003; 9:40–43. PMID:
12508348.

23. Xin Y, Li XL, Wang YP, Zhang SM, Zheng HC, Wu DY, et al. Relationship between phenotypes of cell-function differentiation and pathobiological behavior of gastric carcinomas. World J Gastroenterol. 2001; 7:53–59. PMID:
11819733.

24. Correa P. Human gastic carcinogenesis: a multistep and multifactorial process. First American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res. 1992; 52:6735–6740. PMID:
1458460.
25. Mutoh H, Sakurai S, Satoh K, Tamada K, Kita H, Osawa H, et al. Development of gastric carcinoma from intestinal metaplasia in Cdx2-transgenic mice. Cancer Res. 2004; 64:7740–7747. PMID:
15520178.






 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download