Abstract
Purpose
Peritoneal metastasis is a crucial factor for the prognosis in gastric cancer, but its diagnosis is difficult before laparotomy. This study analyzed the usefulness of diagnostic imaging and various tumor markers in the detection of peritoneal metastasis in gastric cancer.
Materials and Methods
The sera from 768 patients with gastric cancer were measured for CEA, CA19-9 and CA125 levels using a commercial immunoradiometric assay. All the patients underwent diagnostic imaging with computed tomography (CT) and ultrasound (US) before laparotomy.
Results
Preoperative levels of CEA, CA19-9 and CA125 were above the cut-off levels in 15.4%, 8.7% and 5.7% of all cases, respectively. Eighty-eight patients were diagnosed with peritoneal metastasis by laparotomy. CT and US revealed peritoneal dissemination in 15 of 88 patients (17%). Among the three tumor markers, CA19-9 and CA125 showed similar detection rates of peritoneal metastasis (37.5% and 38.6%, respectively). In particular, the serum CA125 levels showed the best sensitivity (38.6%), specificity (98.4%), and diagnostic accuracy (91.5%), and the highest odd ratio (24.46, 95% CI: 11.17~53.57) for predicting peritoneal metastasis among the markers tested. CEA did not add significant predictive information (p=0.471).
The prognosis for gastric cancer with peritoneal metastasis is very dismal, and the quality of life quickly deteriorates because of symptoms such as massive ascites, ileus, and cachexia. Since any delay in diagnosis is detrimental for patients with peritoneal metastasis, it is important to diagnose the degree and extent of peritoneal metastasis, and to make prompt decisions about applicable treatments. Unfortunately, however, the currently used diagnostic imaging techniques such as computed tomography (CT), and ultrasonography (US) often fail to provide an accurate prediction of peritoneal metastasis.
Many papers have been published on the relationship between peritoneal metastasis and different markers such as cytology findings (1), tumor markers (2,3), and molecular markers (4). Although there are no specific tumor-associated antigens in gastric cancers, carcinoembryonic antigen (CEA) and carbohydrate antigens of the sialyl-Lewis A group, such as CA19-9, are known to be elevated in the serum of patients with advanced gastric cancer (5~7). Besides, another carbohydrate antigen, CA125, was also mentioned in the literature. CA125 represents a protein normally expressed by cells lining the fallopian tubes, endometrium, endocervix, peritoneum, pleura and pericardium (8). Serum CA125 is a tumor marker extensively used in patients with ovarian cancer (9).
In this prospective study, we measured preoperative serum CEA, CA19-9, and CA125 levels in patients with gastric cancer and then evaluated the predictive values of these tumor markers for peritoneal metastasis from gastric cancer.
Seven hundred and sixty-eight patients with histologically proven gastric carcinoma who underwent surgery between July 1999 and December 2003 were enrolled in this study. There were 534 males and 234 females. The mean age±standard deviation was 57.3±11.9 years (range 20~83 years). Of these 768 patients, total gastrectomy was performed in 128 patients (16.7%), subtotal gastrectomy in 538 patients (70.0%), proximal gastrectomy in 37 patients (4.8%), and explo-laparotomy or by-pass procedures in 65 patients (8.5%). According to the Union Internationale Contra le Cancer (UICC) TNM classification (10), 351 patients had Stage I disease, 111 had Stage II disease, 154 had Stage III disease, and 152 had Stage IV disease.
All the patients underwent diagnostic imaging by CT and US before laparotomy. Ascites, Krukenberg tumor, and/or omental cake were regarded as peritoneal metastasis. The degree of peritoneal metastasis was defined according to the criteria of the Japanese Research Society for Gastric Cancer (11): P1, metastases to the adjacent peritoneum but not distant peritoneum; P2, a few metastases to the distant peritoneum; P3, numerous metastases to the distant peritoneum.
Peripheral blood samples were obtained from each patient within 1 week before surgery. The commercial immunoradiometric assay was used for measurement of CEA (CIS bio international, Yvette, France), CA19-9 (Immunotech, Marseille, France), and CA125 (Fujirebio Diagnostics, PA, USA).
The cutoff values for serum CEA, CA19-9, and CA125 were 5 ng/ml, 37 U/ml, and 35 U/ml, respectively, according to the manufacturer's instructions.
The nonparametric Mann-Whitney U test was used for comparison of the two independent groups. The predictive value of each tumor marker was assessed by a logistic regression model. A p value less than 0.05 was considered to be statistically significant. All statistical analyses were carried out with the Statistical Package for the Social Science (SPSS, Chicago, IL) program.
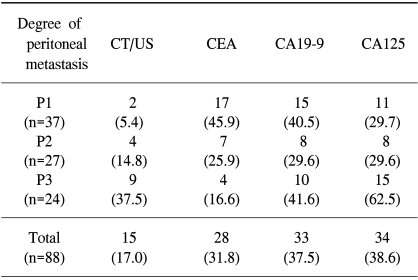
Preoperative levels of CEA, CA19-9 and CA125 were above the cut-off levels in 15.4%, 8.7% and 5.7% of all cases, respectively. Eighty-eight patients were diagnosed with peritoneal metastasis by laparotomy. The diagnostic abilities of various examinations for peritoneal metastasis are summarized in Table 1. Diagnostic imaging (CT and US) revealed peritoneal dissemination in 15 of 88 patients (17%) and showed the lowest sensitivity among these examinations. Among the three tumor markers, CA19-9 and CA125 showed similar detection rates of peritoneal metastasis (37.5% and 38.6%, respectively). As the degree of peritoneal dissemination increased, the positive rate of CA125 increased, whereas the positive rate of CEA decreased accordingly.
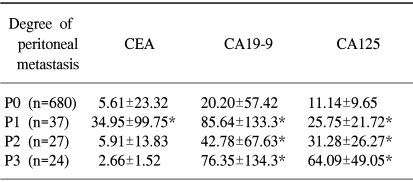
As shown in Table 2, almost the same trend was observed for the correlations between the mean±SD values of serum CEA, CA19-9, and CA125 and the degree of peritoneal dissemination. The serum CA125 levels were significantly higher in P1 through P3 than in P0. However, P1 tumor showed a higher CEA level than did P2 through P3 tumors.
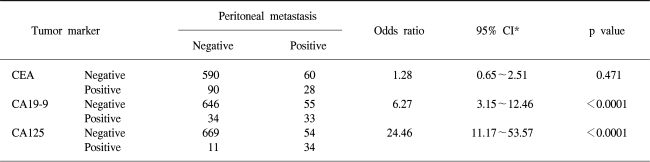
Fig. 1 shows a comparison of various tumor markers for peritoneal metastasis. For CEA, CA19-9 and CA125, each cut-off value was used as a reference value for peritoneal metastasis. CA125 had the best sensitivity (38.6%), specificity (98.4%), and accuracy (91.5%). CA19-9 had the second best sensitivity (37.5%), specificity (95%), and accuracy (88.4%). In contrast, CEA had the worst sensitivity (31.8%), specificity (86.7%), and accuracy (80.4%) among these tumor markers.
The multivariate analysis indicated that patients with preoperative serum CA125 above 35 U/ml had the highest odd ratio (24.46, 95% CI: 11.17~53.57) for predicting peritoneal metastasis among the markers tested. CEA did not add significant predictive information (p=0.471) (Table 3).
Peritoneal metastasis is one of the most difficult problems in patients with gastric carcinoma in terms of diagnosis and treatment. Diagnosis for the peritoneal metastasis involves recognition of ascites on physical examination, recognition of induration of the pouch of Douglas by digital examination, or the use of diagnostic imaging techniques such as CT, US, or magnetic resonance imaging (MRI). However, none of these methods has demonstrated a high predictive value. Therefore, until now, laparotomy plays an important role in the diagnosis of peritoneal metastasis by the direct observation of peritoneal cavity and the estimation of resectability.
Our data indicated a poor sensitivity of CT/US for detecting the peritoneal metastasis. Even for patients with numerous metastases to the distant peritoneum (P3), the diagnostic ability of these examinations was only 37.5%, and these results are comparable to those of other studies (2,12). Recently, laparoscopic examination has been reported to be useful in the detection of peritoneal metastasis (12,13). It allows the direct inspection of the peritoneal cavity, biopsy of suspect nodules, and cytological investigation of washings. It also affords an opportunity to identify small omental and peritoneal implants which may not be detected by imaging modalities. However, its use is not yet prevalent in clinical practice. Surgeons might hesitate to perform laparoscopy before surgical treatment because it is still invasive, although less so than open laparotomy, and is time-consuming and costly.
Many tumor markers, such as CEA, CA19-9, CA72-4, CA125, and CA50, have been studied in the monitoring of gastric cancer, but the sensitivity of any one of them is not sufficient (14~16). CEA and CA19-9 are probably the most well-investigated of all markers to date, and serial examinations have been found useful in postoperative follow-up and detection of recurrence in patients with gastric cancer. CA125 is a sensitive, but not specific, tumor marker that is especially used in the diagnosis and follow-up of ovarian cancer. Lung, liver, biliary tract, stomach, colorectal, and pancreatic malignant tumors are all associated with an increase of serum CA125 levels. This marker is also increased in patients with heart failure, benign pleuropulmonary diseases, peritoneal tuberculosis, and liver cirrhosis. The probable etiology of this marker increment is a diffuse insult to the mesothelial cells. When mesothelial cells of the pleura, peritoneum, pericardium, or fallopian tube are abnormally stimulated, they can increase their normal production of CA125, and its serum level increases (17,18). Only few studies have addressed the possible value of these tumor markers as a preoperative monitor of peritoneal dissemination (2,12).
Our study showed that preoperative positivities for CEA, CA19-9 and CA125 were 15.4%, 8.7% and 5.7%, respectively, in all 768 patients with gastric cancer. However, the sensitivities for peritoneal metastasis were 31.8%, 37.5%, and 38.6%, respectively, in 88 patients with peritoneal metastasis. These significant increases in sensitivity suggested that the serum levels of CA25 and CA19-9 would be highly suitable for monitoring for peritoneal metastasis. Moreover, patients with high CA125 and CA19-9 showed 24.26-fold and 6.27-fold risk of peritoneal metastasis as compared to those with low levels, respectively, at the multivariate analysis (p<0.001). Our study also disclosed that serum CA125 levels were significantly higher in P1 through P3 than in P0; this may reflect the peritoneal dissemination may cause inflammation of peritoneum. On the contrary, we found that P1 tumor showed a higher CEA level than did P2 through P3 tumors. This finding suggested a strong correlation between the serum CEA level and other organ involvement of tumor, such as lymph node or liver, rather than peritoneal involvement.
However, the positivity rate of CA125 in our patients with gastric cancer was quite low (5.7%). We do not propose CA125 as a convenient marker for gastric cancer; it may be useful in patients with highly suspicious peritoneal metastasis prior to surgery or chemotherapy.
Preoperative serum CA19-9 and CA125 levels may provide a predictable value in determining peritoneal metastasis in patients with gastric cancer. In particular, the serum CA125 levels have the best sensitivity, specificity, and diagnostic accuracy, and the highest odd ratio for predicting peritoneal metastasis among the various examinations. Therefore, surgeons can be better prepared for alternative therapy, such as diagnostic laparoscopy or intraperitoneal chemotherapy.
References
1. Bando E, Yonemura Y, Takeshita Y, Taniguchi K, Yasui T, Yoshimitsu Y, Fushida S, Fujimura T, Nishimura G, Miwa K. Intraoperative lavage for cytological examination in 1297 patients with gastric carcinoma. Am J Surg. 1999; 178:256–262. PMID: 10527450.

2. Nakata B, Hirakawa K, Kato Y, Yamashita Y, Maeda K, Onoda N, Sawada T, Sowa M. Serum CA125 level as a predictor of peritoneal dissemination in patients with gastric carcinoma. Cancer. 1998; 83:2488–2500. PMID: 9874453.
3. Nishiyama M, Takashima I, Tanaka T, Yoshida K, Toge T, Nagata N, Iwamori S, Tamura Y. Carcinoembryonic antigen levels in the peritoneal cavity: useful guide to peritoneal recurrence and prognosis for gastric cancer. World J Surg. 1995; 19:133–137. PMID: 7740800.

4. Fujimura T, Ohta T, Kitagawa H, Fushida S, Nishimura GI, Yonemura Y, Elnemr A, Miwa K, Nakamura Y. Trypsinogen expression and early detection for peritoneal dissemination in gastric cancer. J Surg Oncol. 1998; 69:71–75. PMID: 9808508.

5. Kodera Y, Yamamura Y, Torii A, Uesaka K, Hirai T, Yasui K, Morimoto T, Kato T, Kito T. The prognostic value of preoperative serum levels of CEA and CA19-9 in patients with gastric cancer. Am J Gastroenterol. 1996; 91:49–53. PMID: 8561143.
6. Yook JH, Kim BS, Kim YH, Suh BS, Kim WS, Oh ST, Park KC. Diagnostic value of tumor markers in stomach cancer. J Korean Cancer Assoc. 1999; 31:1094–1100.
7. Baek SW, Cho DH, Yoo CH, Han WK. Prognostic value of preoperative serum CEA and CA19-9 levels in gastric cancer patients. J Korean Surg Soc. 2004; 66:27–32.
8. Kabawat SE, Bast RC, Bhan AK, Welch WR, Knapp RC, Colvin RB. Tissue distribution of a coelomic-epithelium-related antigen recognized by the monoclonal antibody OC125. Int J Gynecol Pathol. 1983; 2:275–285. PMID: 6196309.
9. Canney PA, Moore M, Wilkinson PM, James RD. Ovarian cancer antigen CA125: a prospective clinical assessment of its role as a tumor marker. Br J Cancer. 1984; 50:765–769. PMID: 6208925.
10. Sobin LH, Wittekind C. TNM Classification of Malignant Tumors. 1997. 5th ed. New York: Wiley-Liss.
11. Japanese Research Society for Gastric Cancer. Japanese classification of gastric carcinoma. 1998. 2nd English ed. Tokyo: Kanehara.
12. Fujimura T, Kinami S, Ninomiya I, Kitagawa H, Fushida S, Nishimura G, Kayahara M, Shimizu K, Ohta T, Miwa K. Diagnostic laparoscopy, serum CA125, and peritoneal metastasis in gastric cancer. Endoscopy. 2002; 34:569–574. PMID: 12170412.

13. D'Ugo DM, Persiani R, Caracciolo F. Selection of locally advanced gastric carcinoma by preoperative staging laparoscopy. Surg Endosc. 1997; 11:1159–1162. PMID: 9373285.
14. Takahashi Y, Takeuchi T, Sakamoto J, Touge T, Mai M, Ohkura H, Kodaira S, Okajima K, Nakazoto H. The usefulness of CEA and/or Ca19-9 in monitoring for recurrence in gastric cancer patients: a prospective clinical study. Gastric Cancer. 2003; 6:142–145. PMID: 14520526.

15. Lai IR, Lee WJ, Huang MT, Lin HH. Comparison of serum CA72-4, CEA, TPA, CA19-9 and CA125 levels in gastric cancer patients and correlation with recurrence. Hepatogastroenterol. 2002; 49:1157–1160.
16. Gaspar MJ, Arribas I, Coca MC, Alonso MD. Prognostic value of carcinoembryonic antigen, CA19-9 and CA72-4 in gastric carcinoma. Tumor Biol. 2001; 22:318–322.
17. Miralles C, Orea M, Espana P, Provencio M, Sanchez A, Cantos B, Cubedo R, Carcereny E, Bonilia F, Gea T. Cancer antigen 125 associated with multiple benign and malignant pathologies. Ann Surg Oncol. 2003; 10:150–154. PMID: 12620910.

18. Sevinc A, Camci C, Turk HM, Buyukberber S. How to interpret serum CA125 levels in patients with serosal involvement? A clinical dilemma. Oncology. 2003; 65:1–6. PMID: 12837976.
Fig. 1
Comparison of diagnostic ability of peritoneal metastasis by each tumor marker. Solid bar: sensitivity; open bar: specificity; shaded bar: diagnostic accuracy. Sensitivity=(patients with peritoneal metastasis with positive tests/all patients with peritoneal metastasis tested) ×100; Specificity=(patients without peritoneal metastasis with negative tests/all patients without peritoneal metastasis tested) ×100; Diagnostic accuracy=(patients with peritoneal metastasis with positive tests+patients without peritoneal metastasis with negative tests)/(all patients tested) ×100.

Table 1
Comparison of diagnostic abilities of imaging studies (CT and US) and tumor markers for peritoneal metastasis from gastric cancer




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download