Abstract
Purpose
The combination of cisplatin, epirubicin, leucovorin and 5-fluorouracil (PELF) administration, as adjuvant chemotherapy after curative resection for gastirc cancer, was compared with 5-fluorouracil (5-FU) administration alone. This paper reports the results of a prospective randomized comparison of the two regimens, PELF and 5-FU.
Methods
From August 1996 to July 1999, 54 patients were selected subsequent to being diagnosed with stage III cancer after a curative resection for gastric cancer. The patients were stratified according to stage IIIA/IIIB and subtotal/total gastrectomy, and then they were randomized into each treatment group, i.e. the PELF or 5-FU alone groups.
Results
54 assessable patients were enrolled in this study: 28 received PELF and 26 received 5-FU alone. 12 patients relapsed in each group and the median follow-up duration was 42 months (range: 10~77 months). The overall survival rate and disease-free survival rate (DFS) were not significantly different between two groups, (5-year survival of PELF vs. 5-FU: 57% vs. 64%, 5-year DFS: 54% vs. 51%). The PELF combination was more toxic in terms of anemia, anorexia, nausea and diarrhea than the 5-FU.
The incidence and mortality of gastric cancer are high in Oriental countries, and it ranked as the number one cause of cancer incidence and the 2nd most common cause of cancer deaths among Koreans in 2001 (1). In Western countries, although the overall incidence of gastric cancer has decreased, the incidence of proximal gastric cancer has increased, however, the prognosis of this disease remains poor. The only curative treatment is surgical resection of all gross and microscopic diseases, and the disease recurs in locoregional, peritoneal and distant sites in 40% or more of cases, even after curative gastrectomy (2). The overall 5-year survival rate ranges from 10 to 40% (3).
Preoperative and postoperative therapies have been tried to improve the poor outcomes. For 3 meta-analyses, the odds ratio for death after adjuvant chemotherapy ranges from 0.72 to 0.88, and a slight survival benefit was observed (4~6). However, the survival rate of the widely used FAM (5-fluorouracil, adriamycin and mitomycin) regimen was not different from that of an operation alone (7).
Recently, an Italian group reported a response rate of 43% with the PELF (cisplatin, epirubicin, leucovorin and 5-fluorouracil) regimen for advanced gastric cancer (AGC) (8), and our previous phase II study showed the response rate of 47.4% (9). However, the toxicities of both studies were severe. Neri et al reported that the survival rate with the ELF (epirubicin, leucovorin and 5-fluorouracil) regimen as an adjuvant treatment was significantly higher than that of an operation (3-years survival rate: 25 vs. 13%) (10).
5-Fluorouracil (5-FU) showed a response rate of 20% in AGC (11). As an adjuvant therapy, Chou reported the survival rate of 5-FU alone was not different from that of an operation alone (12).
This study was planned to compare the efficacy of the PELF combination chemotherapy with that of 5-FU alone, as an adjuvant chemotherapy after the curative resection for stage III gastric cancer.
The eligible patients were required to have stage III gastric cancer after curative resection, an ECOG performance status (PS) of 0 to 1 with an age from 18 to 65 years old. The patients had adequate bone marrow (WBC ≥4,000/mm3, hemoglobin ≥10.0 g/dL and platelet count of ≥100×109 cells/L), hepatic (serum transaminase ≤2.0 times the upper normal limit) and renal function (serum creatinine level ≤1.2 mg/dL or creatinine clearance ≥60 mL/min). No prior chemotherapy should have been given. The exclusion criteria included: a prior history of malignancies, with the exception of a basal cell carcinoma of the skin or a carcinoma in situ of the cervix, or an active infection or other serious underlying medical conditions. All patients signed their written informed consents and the institutional review board approved this study.
After curative resection, patients were stratified according to stage IIIA/ IIIB and the total gastrectomy/subtotal gastrectomy, and then they were randomized to 2 groups; PELF and 5-FU alone. Adjuvant chemotherapy was administered three weeks after the operation (Fig. 1).
The response rate to the PELF combination was promising, but the toxicity of PELF was severe in the clinical trials (8,9). The incidence of grade 3/4 neutropenia and treatment-associated infections were more than 10% and the incidence of gastrointestinal toxicity was high. In one randomized trial, the survival rate of the ELF adjuvant chemotherapy-received group was higher than that of operation alone (10).
Based on these clinical data, we planned that two cycles of the PELF regimen were to be followed by four cycles of the ELF regimen. The PELF regimen was as follows. Cisplatin 40 mg/m2 and epirubicin 30 mg/m2 were administered intravenously on days 1 and 5, and 5-FU 300 mg/m2 and leucovorin 20 mg/m2 were administered intravenously on days 1 to 4. This regimen was repeated every three weeks. Epirubicin 75 mg/m2 was administered intravenously on day 1 with the 5-FU 450 mg/m2 and leucovorin 20 mg/m2 on days 1 to 3. This regimen was also repeated every three weeks.
The 5-FU alone group was administered 5-FU 500 mg/m2 intravenously on days 1 to 4. This regimen was repeated every three weeks for six cycles.
According to the laboratory findings before each treatment cycle, the dose modification was planned as follows; 5-FU, epirubicin and leucovorin were resumed at 25% dose reduction for WBC of 3,000~3,999/mm3, and the drug regimen was delayed a week for WBC ≤2,999/mm3. Cisplatin was resumed at 50% dose reduction for creatinine levels of 1.6~2.4 mg/dL, and it was withheld for creatinine levels≥2.5 mg/dL.
The toxicities were graded according to the WHO Toxicity Criteria.
All patients underwent a medical history and physical examination. Assessments were conducted before enrollment to the study including CBC, renal and liver function tests, urinalysis, EKG, performance status evaluation, chest X-rays, radionuclide bone scan, abdominal ultrasound and abdominal CT.
Before each treatment course, toxicities and routine laboratory exam were evaluated. The creatinine clearance was measured in the cisplatin-administered patients prior to administration.
The follow-up evaluations done after the treatment included a laboratory exam, chest X-rays, abdominal ultrasound and stool occult blood, and these tests were repeated every 3 months for 2 years, and then every 6 months until 5 years. Gastroscopy was repeated every 2 years.
The histological differentiation was classified as 2 types. One was the differentiated type, including papillary adenocarcinoma and tubular adenocarcinoma, and the other was the undifferentiated type, including poorly differentiated adenocarcinoma, mucinous adenocarcinoma and signet-ring cell adenocarcinoma. The histological type, according to Lauren's classification, was divided into the intestinal and diffuse types. All tissues were stained with VEGF (vascular endothelial growth factor) immunohistochemical stain, and we used polyclonal antibody (Biogenex, San Ramon, CA) for the analysis of prognostic factors.
The primary objective was to compare the 5-year disease-free survival rate (DFS) of the 2 regimens, PELF and 5-FU alone, as adjuvant chemotherapy. The difference of the 5-year DFS was 25% with the power of 0.90 at the one-sided significance level of 0.05. We planned to accrue 88 patients that we could evaluate per arm. The expected duration of the subject registration for the study was estimated to be about 2 years and interim analyses were planned. The follow-up was planned for 4 years after treatment.
The survival rates were estimated using the Kaplan-Meier method. The confidence intervals (CI) were constructed around the Kaplan-Meier estimates, using Greenwood's variance formula. The dose-intensity was calculated using the method of Hryniuk and Bush.
As for the prognostic factors, univariate and multivariate analyses for overall survival were estimated using log-rank and Cox regression tests. The prognostic factors of gastric cancer were analyzed with regard to performance status, gender, age, stage, Lauren's classification, degree of differentiation, expression of VEGF, operation method, chemotherapy regimen and the pattern of recurrence. The patients' characteristics and the side effects between the two groups were also analyzed through the use of k2-test and Fisher's exact test (SPSS software, version 9.0; SPSS Inc, Chicago, IL).
Sixty-one patients were enrolled and treated between August 1996 and July 1999. We had planned to enroll a total of 176 patients, however, the toxicity of the PELF regimen was very severe, i.e., grade 2/3 anemia was 64% and the incidence of gastrointestinal toxicity among non-hematologic toxicities was very high. Therefore, we performed the interim analysis for the fifty-four evaluable patients. These patients were followed up until March 2003. Four of the thirty-two patients in the PELF group dropped out after 1 cycle. The reasons for dropping out were refusal of treatment for 3 patients and the loss to follow up for 1 patient, respectively. Three out of the twenty-nine patients in the 5-FU alone group dropped out. The reasons of dropout were refusal of treatment and loss to follow up after 2 cycles for 1 patient each, and there was a confirmed tumor recurrence before the start of the adjuvant chemotherapy in the third.
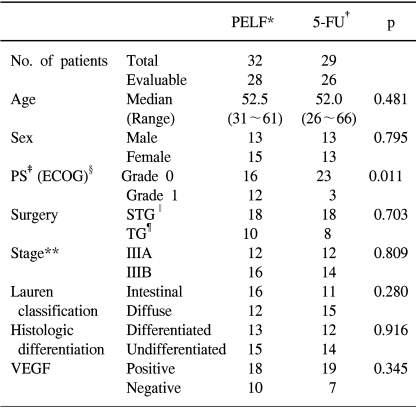
The characteristics of the 54 eligible patients are listed in Table 1. The median age was 52 years, ranging from 31 to 66 years. Twenty-seven (50%) patients were male. The characteristics of both groups were not statistically different, with the exception of the performance status. The performance status of grade 0 was significantly different between the PELF and 5-FU groups (42%: 88%, p=0.011).
A total of 56 cycles of the PELF regimen were administered, with a median of two cycles, ranging from 1 to 2 cycles. A total of 112 cycles of the ELF regimen were administered, with a median of four cycles, ranging from 1 to 4 cycles. A total of 156 cycles of the 5-FU regimen were administered, with a median of six cycles, ranging from 3 to 6 cycles. The mean dose-intensity (DI) of the PELF regimen was 19.9 mg/m2/wk (74.7% of planned dose) for cisplatin, 15.1 mg/m2/wk (75.5% of planned dose) for epirubicin, 302.5 mg/m2/wk (75.6% of planned dose) for 5-FU and 20.4 mg/m2/wk (76.6% of planned dose) for leucovorin. The mean dose-intensity (DI) of the ELF regimen was 19.4 mg/m2/wk (77.6% of planned dose) for epirubicin, 340.0 mg/m2/wk (75.5% of planned dose) for 5-FU and 15.4 mg/m2/wk (76.8% of planned dose) for leucovorin. The mean dose-intensity (DI) of 5-FU alone group was 522.1 mg/m2/wk (78.3% of planned dose).
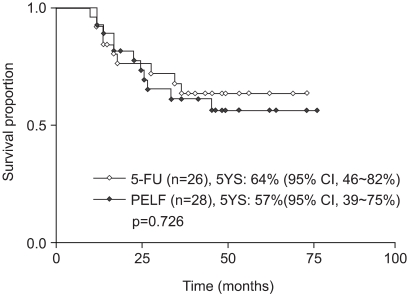
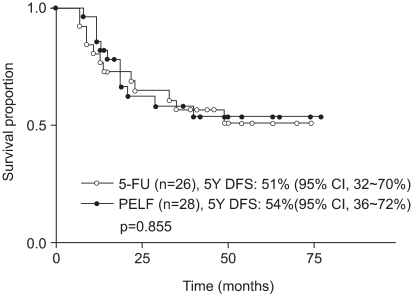
The median follow-up duration was 42 months, ranging from 10 to 77 months. Fig. 2 showed the overall survival of all the patients. The 5-year survival rate (5 YS) between the PELF and 5-FU groups was not different (56.7% vs. 63.8%, p=0.726) (Fig. 3). The disease-free survival rate (DFS) was not different between the two groups (p=0.855) (Fig. 4). The 2- and 5-year DFS of the PELF were 62.5% and 53.8%. Those of 5-FU groups were 65.0% and 51.2%, respectively.
Recurrences of tumor in the PELF and 5-FU groups occurred in twelve patients each. The recurrence rate of both groups was not different (p=0.512). The patterns of recurrence in PELF were 8 patients (67%) had a locoregional and peritoneal metastasis and 4 patients (33%) had a distant metastasis. In the 5-FU groups, the patterns of recurrence were 58% and 42%, respectively.
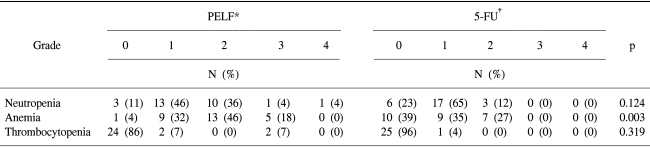
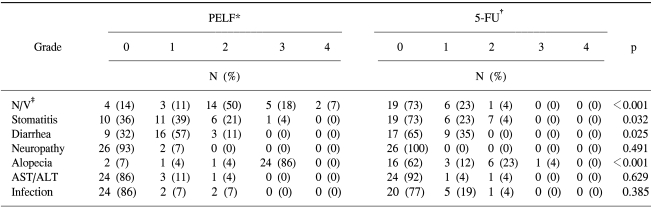
The hematological toxicities of the PELF group were more severe than those of the 5-FU group (Table 2). The grade 3 anemia of the PELF group occurred in 5 (18%) of the 28 patients, and the severe anemia that occurred along with the other hematological toxicities of the PELF group was greater than that of the 5-FU group (p=0.003). Grade 3 or 4 neutropenia and thrombocytopenia only occurred in the PELF group.
Among the non-hematological toxicities, nausea/vomiting, stomatitis, diarrhea, peripheral neuropathy and alopecia were analyzed (Table 3). In the PELF group, there was grade 3/4 nausea/vomiting in 7 patients (25%), grade 3 stomatitis in 1 patient (4%) and alopecia in 24 (86%) of the 28 patients. These non-hematological toxicities in the PELF group were significantly higher than those in the 5-FU group.
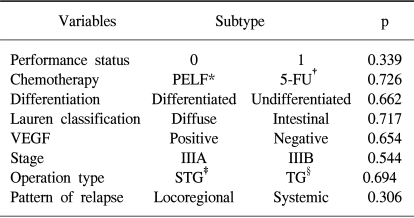
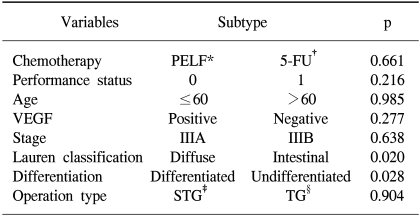
For a univariate analysis for overall survival, the performance status, gender, age, stage, Lauren's classification, histological differentiation, VEGF expression, operation type, chemotherapy regimen and the pattern of recurrence were analyzed. There was no significant variable found (Table 4). In the multivariate analysis for overall survival, the Lauren's classification and histological differentiation were found to be independent factors (Table 5).
Gastric cancer is a chemo-sensitive tumor. 40% of patients diagnosed with gastric cancer are inoperable at the time of diagnosis (13), and 30~40% of those curative resected patients experience recurrence of tumor (14). These are the patients that are suitable for chemotherapy. Since the 1980s and early 1990s, a survival benefit was observed with the use of adjuvant chemotherapy for advanced gastric cancer (15). The hazard ratio for death from four meta-analyses ranged from 0.72 to 0.88, and adjuvant chemotherapy for gastric cancer tended to improve the survival (4~6). However, the efficacy of adjuvant chemotherapy still remains controversial (7,10,16~18). Many phase III trials have been performed using heterogeneous groups, including variable stages and different operative methods, and with no stratification of prognostic factors (3,10,16,17,19~21).
This study was planned to compare the efficacy between two regimens after curative resected stage III gastric cancer with D2 dissection. The result of this study showed that there was no significant difference in the 5-year survival rates (57% vs. 64%, p=0.726) and 5-year DFS (54% vs. 51%, p=0.855) between the PELF and 5-FU alone groups. The performance status among the patients' characteristics was significant different between the two groups. However, we enrolled performance status of 0 to 1, and no difference in the survival according to the performance status was shown. The difference in the performance status had little effect in the analysis of the survival rates between the two groups. There were no differences in overall survival (p=0.805) and DFS (p=0.796) for the performance status of 0 between the two groups. The survival rates of both groups were higher than those of previous reports.
PELF combination chemotherapy has shown high response rates of 43% to 47% in phase II and III trials for advanced gastric cancer (8). In the phase II study, the hematological toxicities observed were grade 3/4 leukopenia and associated infections in 11% and 13%, respectively. Grade 3/4 nausea/vomiting and diarrhea were observed of 13% and 8%, respectively. In the phase III study, nausea/vomiting, stomatitis and diarrhea were observed to be higher than in the control group (p<0.05) In this study, grade 3 anemia of the PELF group was 18% (p=0.003). Grade 3/4 leukopenia and grade 3 thrombocytopenia were only observed in the PELF group. Grade 3/4 nausea/vomiting and stomatitis of the PELF group were higher than for the 5-FU group (p<0.05).
The principal prognostic factors of gastric cancer are the TNM staging, with the depth of the tumor invasion, the number of involved lymph nodes and distant metastasis, as well as the Lauren's classification, differentiation and tumor markers. In this study, the TNM staging, operation type (tumor location, subtotal or total gastrectomy), Lauren's classification, differentiation, VEGF expression, chemotherapy regimen and the pattern of recurrence were analyzed as the prognostic factors. In the multivariate analysis for overall survival, the Lauren's classification and differentiation were found to be the independent prognostic factors. The survival for patients with the intestinal tumor type has been shown to be better than that of the diffuse type (p=0.020). The survival of the differentiated group has been shown to be better than that of the undifferentiated group (p=0.028). According to the analysis of prognostic factors, these subtypes should be more aggressively treated.
The overall and disease-free survival rate were not significantly different between the two groups (5YS for PELF vs. 5-FU alone: 57% vs. 64%, 5-year DFS: 54% vs. 51%). The PELF combination treatment was more toxic in terms of anemia, anorexia, nausea, stomatitis and diarrhea, than the 5-FU treatment alone. This study showed that the PELF combination treatment, as an adjuvant therapy for gastric cancer after curative resection, was less effective but had more toxic side effects than the 5-FU treatment alone. In the future, the use of new chemotherapeutic agents along with irinotecan, capecitabine, paclitaxel and docetaxel should be tried as adjuvant chemotherapy regimens (22~25).
References
1. Government of the Republic of Korea. Annual report on the cause of death statistics, 2001. 2002. Daejeon: Korea National Statistical Office.
2. Abe S, Ogawa Y, Nagasue N, Sasaki Y, Akamizu H, Hirose S, Yukaya H, Suehiro S. Early gastric cancer: results in general hospital in Japan. World J Surg. 1984; 8:308–314. PMID: 6464487.
3. Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ. Extended lymph node dissection for gastric cancer. Dutch Gastric cancer Group. N Engl J Med. 1999; 340:908–914. PMID: 10089184.
4. Hermans J, Bonenkamp JJ, Boon MC, Bunt AMG, Ohyama S, Sasako M, Van de Velde CJH. Adjuvant therapy after curative resection for gastric cancer: Mea-analysis of randomized trials. J Clin Oncol. 1993; 11:1441–1447. PMID: 8336183.
5. Earle CC, Maroun JA. Adjuvant chemotherapy after curative resection for gastric cancer in non-asian patients: Revisiting a meta-analysis of randomised trials. Eur J Cancer. 1999; 35:1059–1064. PMID: 10533448.

6. Janunger KG, Hafstrom L, Nygren P, Glimelius B. A systemic overview of chemotherapy effects in gastric cancer. Acta Oncol. 2001; 40:300–326.
7. Coombes RC, Schein PS, Chilvers CE, Wils J, Beretta G, Bliss JM, Rutten A, Amadori D, Cortes-Funes H, Villar-Grimalt A. A randomized trial comparing adjuvant fluorouracil, doxorubicin, and mitomycin with no treatment in operable gastric cancer. International Collaborative Cancer Group. J Clin Oncol. 1990; 8:1362–1369. PMID: 2199622.

8. Giorgio C, Mariangela B, Sandra Z, Renato A, Cecilia F. Fluorouracil, doxorubicin, and mitomycin combination versus PELF chemotherapy in advanced gastric cancer: A prospective randomized trial of the Italian oncology group for clinical research. J Clin Oncol. 1994; 12:2687–2693. PMID: 7989945.
9. Park IR, Kim SY, Kim JH, Yoon HJ, Cho KS. Cisplatin, epirubicin, leucovorin and 5-fluorouracil combination chemotherapy for advanced gastric cancer: Interim report. J Korean Cancer Assoc. 1998; 30:907–913.
10. Neri B, de Leonardis V, Romano S, Cini G. Adjuvant chemotherapy after gastric resection in node-positive cancer patients: a multicenter randomised study. Br J Cancer. 1996; 73:549–552. PMID: 8595173.
11. Louvert C, de Gramont A, Demuynck B. High-dose folinic acid, 5-fluorouracil bolus and continuous infusion in poor- prognosis patients with advanced measurable gastric cancer. Ann Oncol. 1991; 2:229–230. PMID: 2043494.
12. Chou F, Sheen-Chen S, Liu P, Liu PP, Chen FC. Adjuvant chemotherapy for resectable gastric cancer: a preliminary report. J Surg Oncol. 1994; 57:40–45. PMID: 8065152.

13. Woo BI, Park SH, Choi KW. Clinical analysis of patients with gastrectomized stage IV stomach cancer. J Korean Cancer Assoc. 1999; 31:1120–1128.
14. Comis RL, Canter SK. A review of chemotherapy in gastric cancer. Cancer. 1974; 34:1576–1586. PMID: 4279136.

15. Glimelius B, Ekstrom K, Hoffmann K. Randomized comparison between chemotherapy plus best supportive care with best supportive care in advancced gastric cancer. Ann Oncol. 1997; 8:163–167. PMID: 9093725.
16. Cirera L, Balil A, Batiste-Alentorn E. Randomized clinical trial of adjuvant mitomycin plus tegafur in patients with resected stage III gastric cancer. J Clin Oncol. 1999; 17:3810–3815. PMID: 10577853.

17. Grau J, Estape J, Alcobendas F. Positive results of adjuvant MMC in resected gastric cancer: a randomized trial on 134 patients. Eur J cancer. 1993; 29:340–342. PMID: 8398330.
18. MacDonald JS, Fleming TR, Peterson RF. Adjuvant chemotherapy with FAM versus surgery alone for patients with locally advanced gastric adenocarcinoma: a Southwest Oncology Group study. Ann Surg Oncol. 1995; 2:488–494. PMID: 8591078.
19. Imanaga H, Nakazato H. Rseults of surgery for gastric cancer and effect of adjuvant mitomycin C on cancer recurrence. World J Surg. 1977; 2:213–221. PMID: 868069.
20. Pugliese R, Maggioni D, Berardi V, Scandroglio I, Pisani D, Mariani A, Di Lernia S, Valli C, Cocotta E. Extended (D2) lymphadenectomy in gastric cancer: a five year experience. Int Surg. 2000; 85:209–215. PMID: 11324997.
21. Onate-Ocana LF, Aiello-Crocifoglio V, Mondragon-Sanchez R, Ruiz-Molina JM. Survival benefit of D2 lympadenectomy in patients with gastric adenocarcinoma. Ann Surg Oncol. 2000; 7:210–217. PMID: 10791852.
22. Boku N, Ohtsu A, Shimada Y. Phase II study of a combination of irinotecan and cisplatin against metastatic gastric cancer. J Clin Oncol. 1999; 17:319–323. PMID: 10458249.

23. Murad AM, Petroianu A, Guimaraes RC. Phase II trial of the combination of paclitaxel and 5-fluorouracil in the treatment of advanced gastric cancer: a novel, safe, and effective regimen. Am J Clin Oncol. 1999; 22:580–586. PMID: 10597742.
24. Kim T, Ahn J, Lee J. A phase II trial of capecitabine and cisplatin in previous untreated advanced gastric cancer. Proc Am Soc Clin Oncol. 2001; 20:142b.
25. Chun HG, Puccio CA, Mittelman A. Weekly docetaxel and continuous infusion 5-fluorouracil in elderly patients with cancer of stomach and distal esophagus. Proc Am Soc Clin Oncol. 2001; 20:162b.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download