Abstract
Phlebosclerotic colitis is a rare disease of intestinal ischemia and differentiating it from the typical ischemic colitis. It is caused by venous obstruction due to colonic and mesenteric venous calcification. We report a 36-year-old woman presenting with intermittent abdominal pain. Initial radiologic findings showed multiple tortuous thread-like calcifications in the region of the right side of the colon and transverse colon on plain abdominal radiographs and computed tomography images. In the colonoscopy, edematous dark-bluish colonic mucosa, sclerotic colon wall, and multiple ulcers without clear boundaries were observed from the ascending colon to the transverse colon. In the sigmoid colon only showed the edematous dark-bluish colonic mucosa, sclerotic colon wall. On the basis of these findings, we diagnosed the patient as having phlebosclerotic colitis. We report a rare case of phlebosclerotic colitis in healthy young woman.
Ischemic colitis usually develops due to arteriosclerosis, diabetes, hypovolemic shock, portal hypertension, malignant tumors, pancreatitis, or colonic obstruction. It is very common in elderly people.1 Phlebosclerotic colitis (PC) is a rare form of ischemic colitis that develops as a result of mesenteric venous calcification and calcification in the invaded colonic submucosal layer.23 PC is usually observed in the colons of elderly men.4
A young woman without any underlying diseases visited our hospital owing to abdominal pain. Colonoscopy revealed edematous dark-bluish colonic mucosa, a sclerotic colon wall, and multiple ulcers without clear boundaries from the ascending colon to the transverse colon. The edematous dark-bluish colonic mucosa and sclerotic colon wall were observed only in the sigmoid colon. Abdominopelvic computed tomography (CT) revealed linear calcification on the colon wall from the terminal ileum to the transverse colon. Arterial phase superior mesenteric angiography revealed an irregular and convoluted marginal artery and vasa recta. Delayed phase images showed convoluted and expanded veins along the vasa recta. These findings were related to PC.
Here, we report a case of PC that showed symptomatic improvement with conservative treatment only.
A 36-year-old woman visited our hospital with a major complaint of acute pain in her lower right abdomen. She had no history of tobacco, alcohol, or herbal medicine use, underlying diseases such as hypertension or diabetes, and surgery. She had been treated for unexplained rhinitis for 5 years. At admission, her vital signs were as follows: blood pressure, 100/70 mm Hg; pulse, 98 beats per minute; respiratory rate, 18 breaths per minute; and body temperature, 36.6℃. Physical examination revealed mild oppressive pain and rebound tenderness in the lower right abdominal area. Peripheral blood examination yielded the following results: white blood cell count, 16,700/mm3 hemoglobin level, 14.0 g/dL; platelet count 340,000/mm3; and neutrophil proportion, 91.1%. Biochemical testing revealed the following levels: aspartate aminotransferase/alanine aminotransferase, 21/14 IU/L; total protein/albumin, 7.4/4.5 g/dL; total/direct bilirubin, 0.29/0.28 mg/dL; alkaline phosphatase/γ-glutamyl transpeptidase, 125/18 IU/L; amylase/lipase, 97/86 IU/L; and blood urea nitrogen/creatinine, 13.3/0.84 mg/dL. The results of electrolyte testing were normal. Normal findings were also obtained for rheumatoid factors: antinuclear antibody (-), anti-neutrophil cytoplasmic antibody (-), antiphospholipid immunoglobulin M (IgM) (-), and antiphospholipid IgG (-).
Plain abdominal X-ray revealed a paralytic ileus and linear calcification along the colon wall in the lower right abdominal area (Fig. 1). Abdominopelvic CT revealed that the colon wall from the terminal ileum to the transverse colon was thickened, and multiple calcifications were observed on the colon wall and in the ramifications of the colonic blood vessels (Fig. 2). Abdominopelvic CT also revealed that the portal vein size was normal in size, implying that portal pressure was within the normal range (Fig. 2).
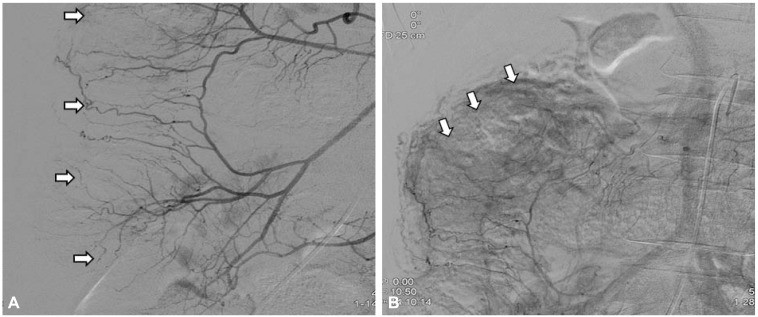
Colonoscopy showed edematous dark-bluish colonic mucosa, a sclerotic colon wall, and multiple ulcers without clear boundaries from the ascending colon to the transverse colon. The edematous dark-bluish colonic mucosa and sclerotic colon wall was seen only in the sigmoid colon (Fig. 3A, B). Superior mesenteric angiography arterial-phase images showed an irregular and convoluted marginal artery and vasa recta, and delay-phase images showed convoluted and expanded veins along the vasa recta (Fig. 4).
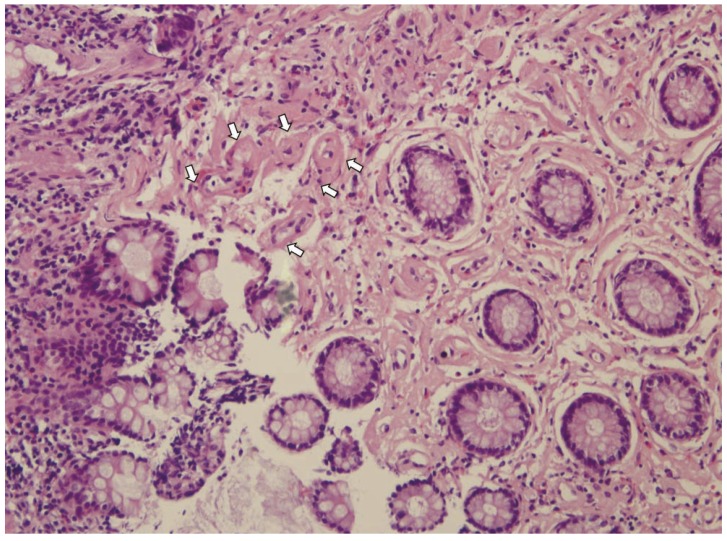
A biopsy conducted during colonoscopy revealed fibrosis in the blood vessel walls and lamina propria mucosae, but fibrosis in the submucosal layer was not confirmed due to the insufficient number of samples (Fig. 5).
Based on the characteristics discussed above, we made a diagnosis of PC, after which conservative treatment including fasting and fluid therapy was initiated. These conservative treatments were continued given the absence of any findings of inflammation along the entirety of the colon wall and the presence of accompanying peritonitis caused by necrosis and perforation. The patient's abdominal pain was alleviated; she no longer complained of symptoms even after starting a solid food diet, and was discharged 10 days after admission. She underwent follow-up colonoscopy 10 days after discharge, and slightly improved ulcerative findings were obtained (Fig. 3C).
Endoscopic mucosal resection was performed to obtain submucosal tissues, but insufficient samples could be collected due to severe sclerosis in the colonic mucosa.
PC is a rare type of ischemic colitis, an on-thrombotic venous colitis characterized by colonic and mesenteric venous calcification and fibrosis.1 The pathogenesis of PC is unclear, although calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia syndrome; toxic chemicals; and pressure increases in the colon lumen, which may be hereditary, have been reported; as none of these were observed in this patient, they are not of clinical relevance.356789 Kusanagi et al.2 suggested that secondary portal hypertension caused by liver cirrhosis or chronic liver disease may represent the etiology of PC. Meanwhile, Yao et al.1 reported two cases of PC accompanied by normal portal vein pressure, implying that no clear mechanism has yet been established.
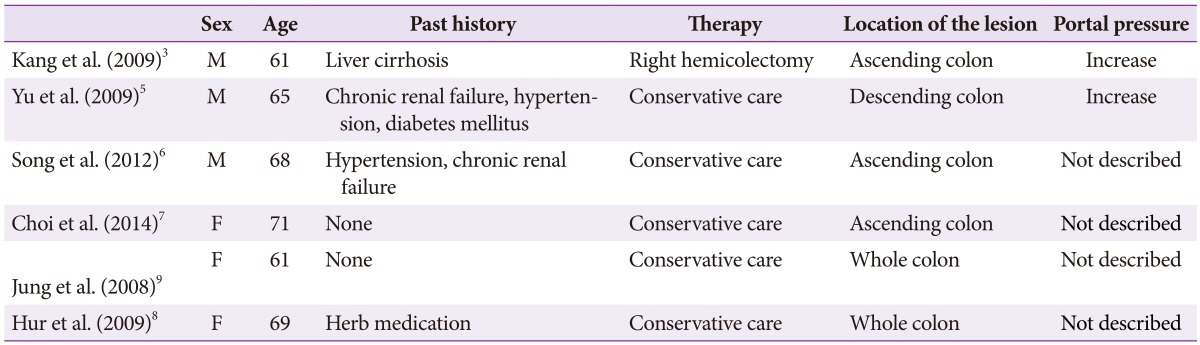
The six cases of PC reported in South Korea to date included three men with underlying diseases such as renal failure, liver cirrhosis, diabetes, and hypertension (Table 1). In women, there was no underlying disease in two patients, while a history of herbal medication was observed in one patient. The average age of the six patients was 65.8 years, and all patients were aged from 60 to 70 years. In South Korea, there was no common cause considering the associated diseases (Table 1). In the present case, a young woman had a medical history of treatment for rhinitis of unknown origin and dark blue pigmentation around her eyes for 5 years. We thought that the pigmentation was a sign of venous congestion. We suspected a relationship between PC and the pigmentation around her eyes, even though it is not clear whether PC invades any organs other than the mesenteric vein.
PC usually involves symptoms such as acute abdominal pain, diarrhea, bloody stool, and vomiting, but sometimes shows no symptoms. PC is found in the appendix or ascending colon by accident during colonoscopy, and appears as thread-like calcifications on plain abdominal radiography and venous congestion and hyperplasia in the colon wall, calcification in the colon wall, and mesenteric veins on abdominopelvic CT scans.145671011121314151617
Among the six PC cases reported in South Korea, three involved ascending to transverse colon wall calcification, one involved ileum to descending colon wall calcification, and two involved whole colonic wall calcification detected by abdominopelvic CT scans.356789 Among the four reported cases studied by superior mesenteric angiography, three showed a convoluted marginal artery on arterial-phase images, and one showed expanded and convoluted veins on delay-phase images.131013 In the present case, an irregular and convoluted marginal artery and vasa recta were observed on arterial-phase images, and convoluted and expanded veins were observed along the vasa recta (Fig. 4).
Colonoscopy often reveals bluish violet or dark-brownish mucosa invading the colon, cylindrical ulcers, and loss of the fissures of the semilunar colon fold.456711121314 In the tissues obtained during surgery, findings of colonic hyperplasia accompanying sclerosis and edema, and loss of the fissures on the semilunar colon fold are observable. Microscopic findings often include mucosal and submucosal necrosis, submucosal blood vessel calcification, and sclerosis. Mucosal atrophy or treatable ulcers may also be seen.141015
PC can be treated with surgery or conservative therapy. Markos et al.10 suggested surgical treatments such as colectomy in cases involving inflammation is present on the whole colon wall in addition to peritonitis caused by necrosis and perforation. However, Yu et al.18 reported a case in which conservative treatments were used, which showed no specific symptoms during the 4-year follow-up period.
The six cases of PC reported in South Korea included one case in which a right hemicolectomy was performed, and five cases in which the patient was discharged and experienced improvement in symptoms after conservative treatment (Table 1).
It is necessary to differentiate PC from diseases that can cause chronic mesenteric ischemia, including Churg-Strauss syndrome, Behcet's disease, lymphocytic phlebitis, Degos disease, Wegener's granulomatosis, and polyarteritis nodosa.1920 However, these diseases do not involve fibrosis and calcification in the veins.
The etiology and mechanisms of PC are not yet fully understood, and appropriate treatment methods other than colectomy in cases with complications have not yet been established. Further studies may be necessary.
In this study, PC was diagnosed through radiography and colonoscopy in a 36-year-old woman who visited our hospital with a major complaint of pain in her lower right abdomen. Here, we report, with a literature review, a rare case of PC that developed in a young woman with no underlying diseases.
References
1. Yao T, Iwashita A, Hoashi T, et al. Phlebosclerotic colitis: value of radiography in diagnosis: report of three cases. Radiology. 2000; 214:188–192. PMID: 10644121.
2. Kusanagi M, Matsui O, Kawashima H, et al. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am J Roentgenol. 2005; 185:441–447. PMID: 16037518.

3. Kang HY, Noh R, Kim SM, Shin HD, Yun SY, Song IH. Phlebosclerotic colitis in a cirrhotic patient with portal hypertension: the first case in Korea. J Korean Med Sci. 2009; 24:1195–1199. PMID: 19949682.

4. Hu P, Deng L. Phlebosclerotic colitis: three cases and literature review. Abdom Imaging. 2013; 38:1220–1224. PMID: 23589075.

5. Yu SC, Kim JI, Lee SY, et al. A case of phlebosclerotic colitis in a patient of chronic renal failure. Korean J Gastrointest Endosc. 2009; 38:107–110.
6. Song JH, Kim JI, Jung JH, et al. A case of phlebosclerotic colitis in a hemodialysis patient. Korean J Gastroenterol. 2012; 59:40–43. PMID: 22289953.

7. Choi JM, Lee KN, Kim HS, et al. Idiopathic phlebosclerotic colitis: a rare entity of chronic ischemic colitis. Korean J Gastroenterol. 2014; 63:183–186. PMID: 24651592.

8. Hur CJ, Kim EY, Oh JS, et al. A case of idiopathic mesenteric phlebosclerosis. Korean J Gastrointest Endosc. 2009; 38:352–355.
9. Jung HG, Koh JW, Lee MY. A case of idiopathic mesenteric phlebosclerosis. Korean J Gastroenterol. 2008; 52:261–264. PMID: 19077529.
10. Markos V, Kelly S, Yee WC, Davis JE, Cheifetz RE, Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am J Roentgenol. 2005; 184:1584–1586. PMID: 15855120.

11. Maruyama Y, Watanabe F, Kanaoka S, et al. A case of phlebosclerotic ischemic colitis: a distinct entity. Endoscopy. 1997; 29:334. PMID: 9255548.

12. Chen MT, Yu SL, Yang TH. A case of phlebosclerotic colitis with involvement of the entire colon. Chang Gung Med J. 2010; 33:581–585. PMID: 20979710.
13. Saito Y, Taniguchi M, Tagawa K, Ibukuro K, Mori M, Emura F. Phlebosclerotic colitis with deep circumferential ulceration: three-year endoscopic follow-up. Report of a case. Dis Colon Rectum. 2005; 48:2347–2351. PMID: 16258707.

14. Hozumi H, Hokari R, Shimizu M, et al. Phlebosclerotic colitis that was difficult to distinguish from collagenous colitis. Dig Endosc. 2014; 26:594–598. PMID: 23902595.

15. Kato T, Miyazaki K, Nakamura T, Tan KY, Chiba T, Konishi F. Perforated phlebosclerotic colitis: description of a case and review of this condition. Colorectal Dis. 2010; 12:149–151. PMID: 19175648.
16. Tamamoto F, Ishizaki H, Maehara T. Phlebosclerotic colitis. Radiat Med. 2008; 26:164–167. PMID: 18683572.

17. Chang YY, Lin HH, Lin CC. Phlebosclerotic colitis presenting as intestinal obstruction. Clin Gastroenterol Hepatol. 2014; 12:e81–e82. PMID: 24561098.

18. Yu CJ, Wang HH, Chou JW, et al. Phlebosclerotic colitis with nonsurgical treatment. Int J Colorectal Dis. 2009; 24:1241–1242. PMID: 19390857.

19. Oshitani N, Matsumura Y, Kono M, et al. Asymptomatic chronic intestinal ischemia caused by idiopathic phlebosclerosis of mesenteric vein. Dig Dis Sci. 2002; 47:2711–2714. PMID: 12498290.
20. Iwashita A, Yao T, Schlemper RJ, et al. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003; 46:209–220. PMID: 12576895.
Fig. 1
Plain abdominal radiographic finding. It showed multiple linear calcifications in the right lower quadrant (white arrows).
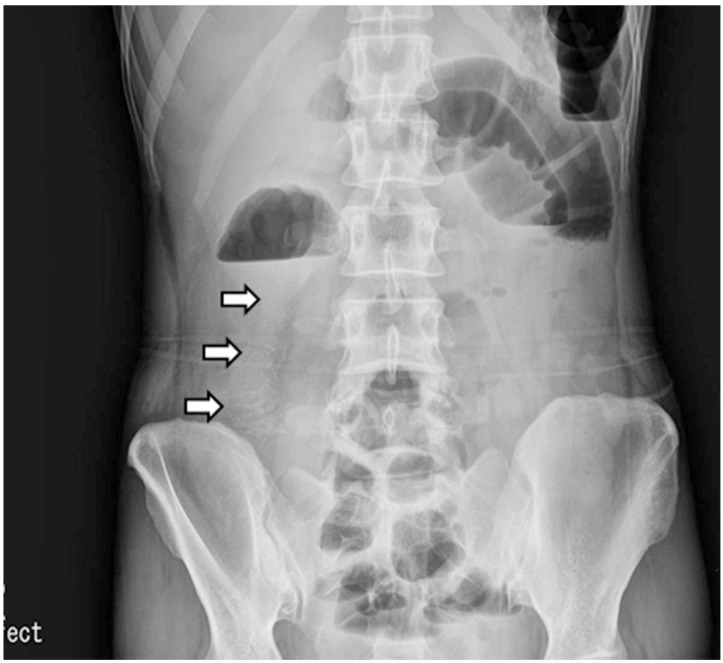
Fig. 2
(A, B) Abdominopelvic computed tomography finding. The enhanced computed tomography showed the thickening of the colonic wall with calcifications (white arrows).
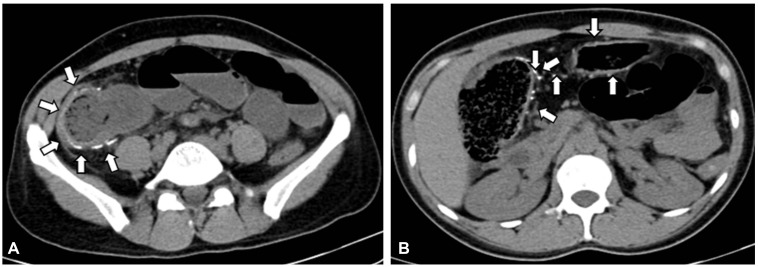
Fig. 3
Colonoscopic findings. (A, B) It noted dark blue colored edematous mucosa and ulcerations without clear boundaries from ascending colon to the sigmoid colon. (C) The follow-up colonoscopy. Improved fine ulcers were found in the ascending colon after 10 days of a discharge.
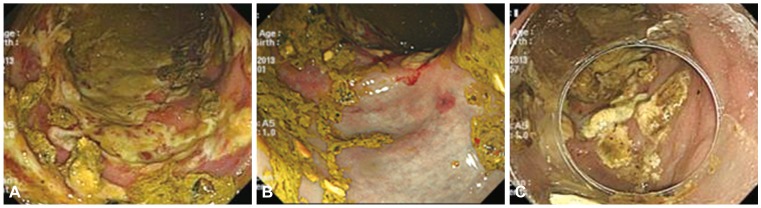
Fig. 4
Superior mesenteric angiography. (A) It indicated irregularity and tortuosity (arrows) of marginal arteries and vasa recta in right colic area at the arterial phase. (B) It indicated venous pooling (arrows) along the ascending colon at the delayed phase.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download