Abstract
References
Fig. 1
A 58-year-old man who received a total gastrectomy with a Roux-en-Y anastomosis had a 17-mm brown stone removed by single balloon enteroscope (SBE)-assisted endoscopic retrograde cholangiopancreatography (ERCP). (A) Simple radiography showing the tip of the SBE reaching the end of the afferent loop. (B) The SBE was withdrawn leaving the overtube. (C) An esophagogastroduodenoscope was inserted successfully through the in-dwelling overtube. (D) A cholangiogram showing a diffuse dilatation and a 17-mm filling defect in the common bile duct. Endoscopic papillary dilatation was performed with the controlled radial expansion balloon. (E) The stone was removed using a mechanical lithotripter and a retrieval balloon. (F) An endoscopic nasobiliary drain was inserted and ERCP was completed successfully.
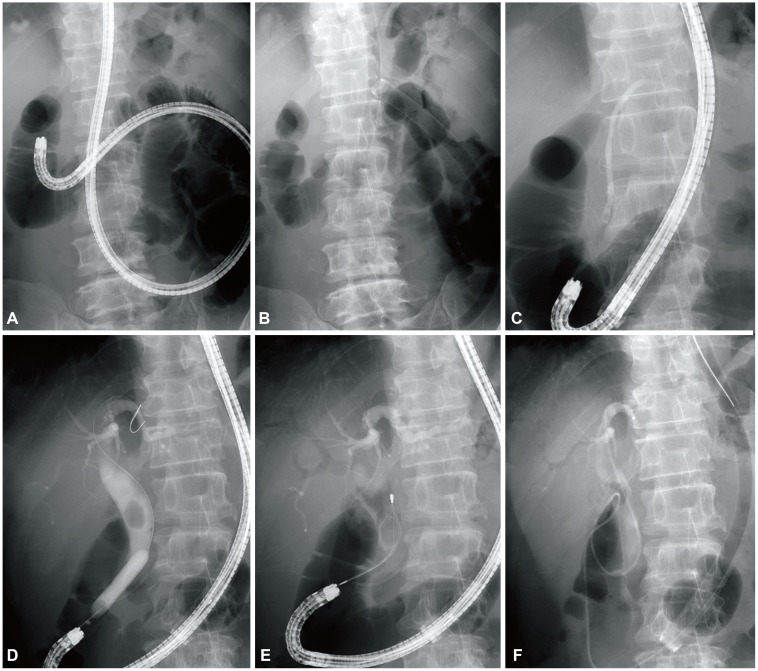
Fig. 2
A 78-year-old man who received a prior total gastrectomy with a Roux-en-Y anastomosis had small brown stones successfully removed by single balloon enteroscope (SBE)-assisted endoscopic retrograde cholangiopancreatography (ERCP). (A) The SBE reached the afferent loop. (B) The enteroscope was 80 cm in length. (C) While inserting the esophagogastroduodenoscope, an acute angulation was made 25 cm distal to the overtube. After the collapsed site was dilated by the controlled radial expansion (CRE) balloon, a conventional endoscope could be inserted into the overtube. (D) Endoscopic view; the CRE balloon dilated the acute angulation. (E) Dilatation of the common bile duct was noted on the cholangiogram. (F) Endoscopic papillary dilatation was performed with a CRE balloon. (G) Small brown stones were removed using the retrieval balloon. (H) An endoscopic nasobiliary drainage was inserted and ERCP was completed successfully.
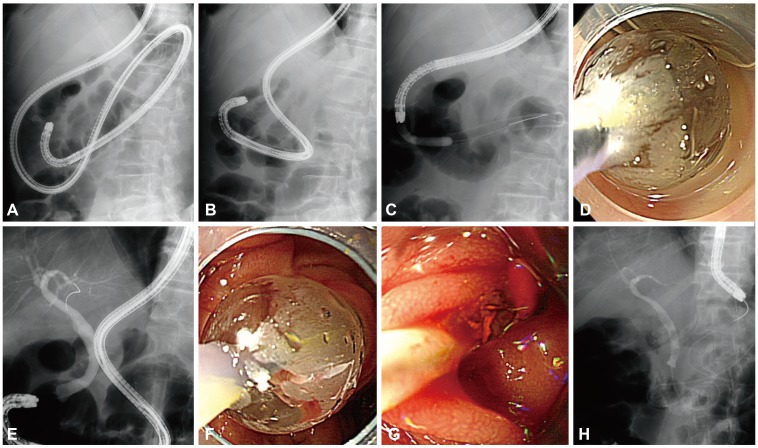
Table 1
Characteristics and Diagnostic and Therapeutic Success Rate for Endoscopic Retrograde Cholangiopancreatography of Colonoscopy, DBE, and SBE Performed in Patients with Altered Anatomy
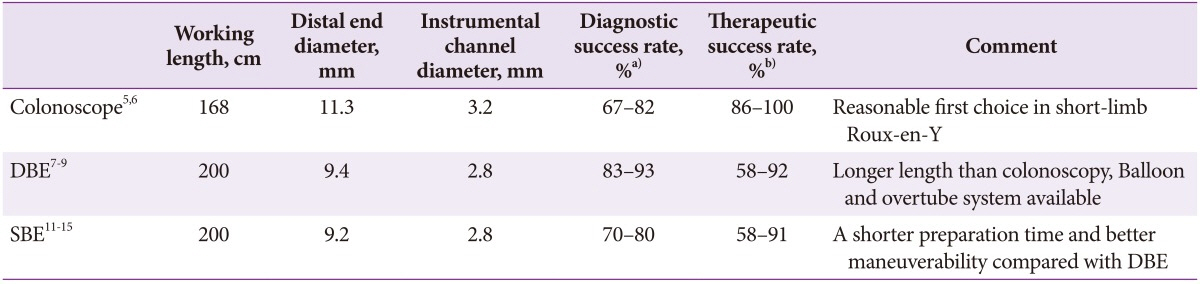
Pediatric colonoscope (PCF-140L; Olympus Co.), DBE (EN-450T5; Fujinon), and SBE (SIF-Q180 or SIF-Q260; Olympus Co.) were used in these studies.
DBE, double balloon enteroscopy; SBE, single balloon enteroscopy.
a)Diagnostic success rate defined as successful pancreaticobiliary duct cannulation or securing of the diagnosis; b)Therapeutic success rate defined as successfully accomplishing the endoscopic therapy.
Table 2
Patient Characteristics and Outcomes of Single Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography
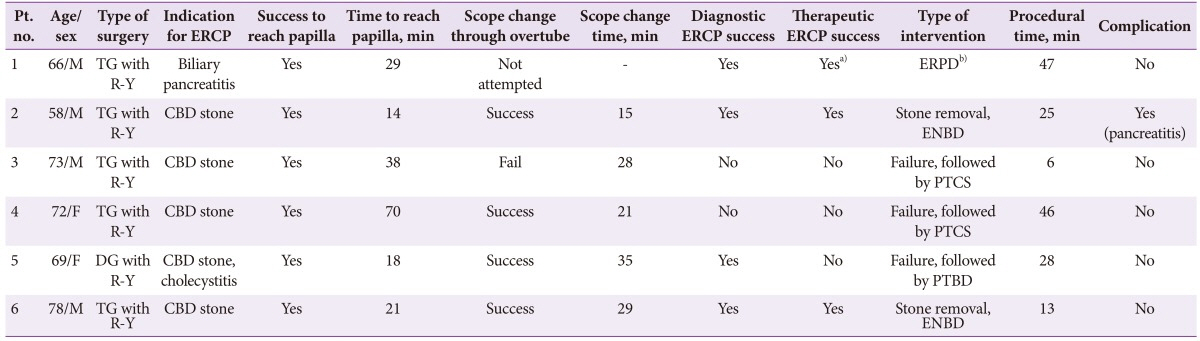
Pt., patient; ERCP, endoscopic retrograde cholangiopancreatography; TG, total gastrectomy; R-Y, Roux-en-Y anastomosis; ERPD, endoscopic retrograde pancreatic drainage; CBD, common bile duct; ENBD, endoscopic nasobiliary drainage; PTCS, percutaneous transhepatic choledochoscopy; DG, distal gastrectomy; PTBD, percutaneous transhepatic biliary drainage.
a)A self-assembled long catheter was used in this case; b)In this patient, a plastic stent was inserted into the pancreatic duct to improve a pancreatitis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download