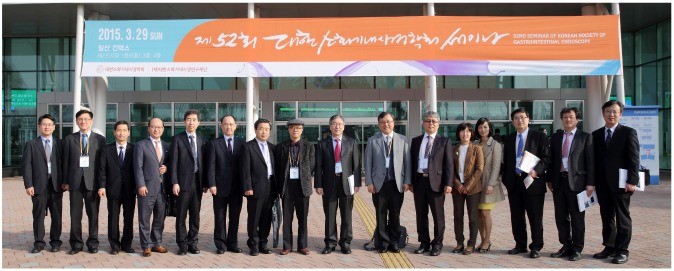
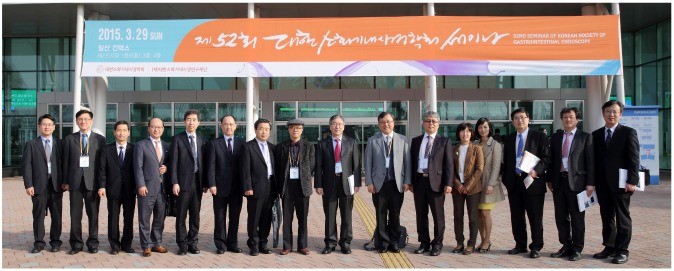
 | Fig. 1A group photo showing the great contribution at the successful 52nd Seminar of the Korean Society of Gastrointestinal Endoscopy. From the left, Jae Myung Park (Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul), Sam Ryong Jee (Inje University Busan Paik Hospital, Inje University College of Medicine, Busan), Jeong Seop Moon (Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul), Il Kwun Chung (Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan), Yoon Tae Jeen (Korea University Anam Hospital, Korea University College of Medicine, Seoul), Oh Young Lee (Hanyang University Seoul Hospital, Hanyang University College of Medicine, Seoul), Yong Woon Shin (Inha University Hospital, Inha University School of Medicine, Incheon), Sang Yong Seol (Inje University Busan Paik Hospital, Inje University College of Medicine, Busan), Sei Jin Youn (Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju), Myung-Gyu Choi (Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul), Chang-Hun Yang (Dongguk University Gyeongju Hospital, Dongguk University College of Medicine, Gyeongju), Eun Young Kim (Daegu Catholic University Medical Center, Catholic University of Daegu School of Medicine, Daegu), Ki-Nam Shim (Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul), Ki Baik Hahm (CHA Bundang Medical Center, CHA University, Seongnam), Don Haeng Lee (Inha University Hospital, Inha University School of Medicine, Incheon), and Young Seok Cho (Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea).
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download