Abstract
Background/Aims
To investigate whether the EndoLifter (Olympus), a counter-traction device facilitating submucosal dissection, can accelerate endoscopic submucosal dissection (ESD).
Methods
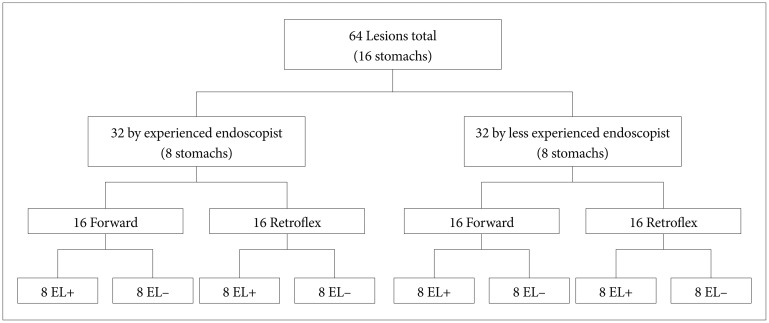
Two endoscopists (novice/expert in ESD) performed 64 ESDs (artificial 3-cm lesions) in 16 ex vivo pig stomachs: per stomach, two at the posterior wall (forward approach) and two at the lesser curvature (retroflex approach). Per approach, one lesion was dissected with (EL+) and one without (EL-) the EndoLifter. The submucosal dissection time (SDT), corrected for specimen size, and the influence of ESD experience on EndoLifter usefulness were assessed.
Results
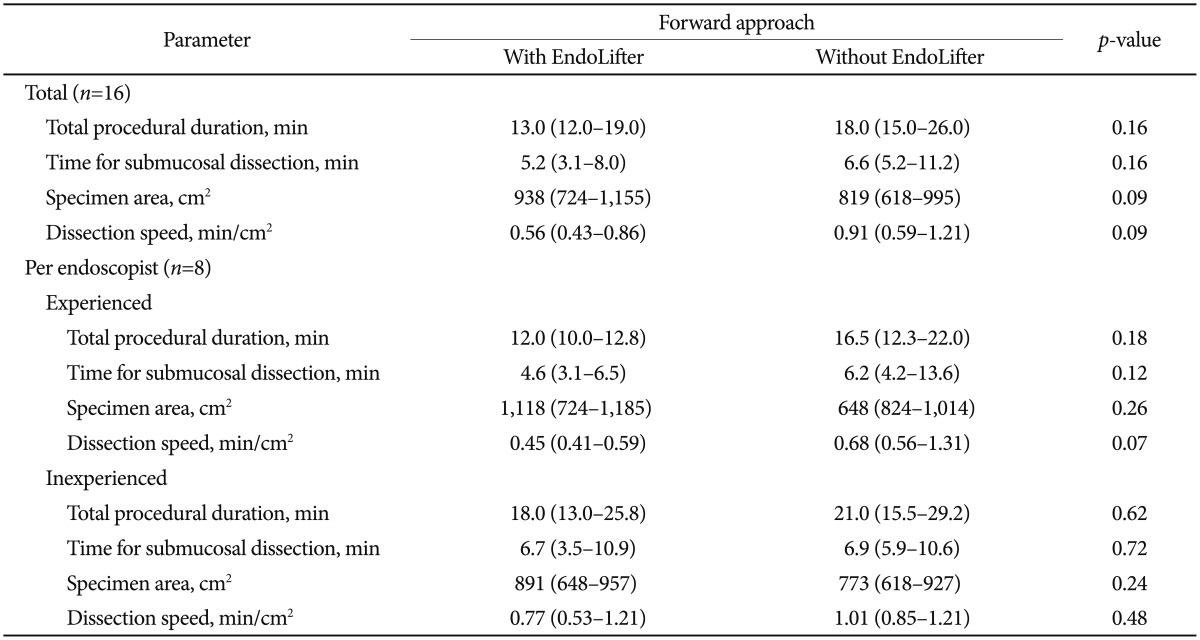
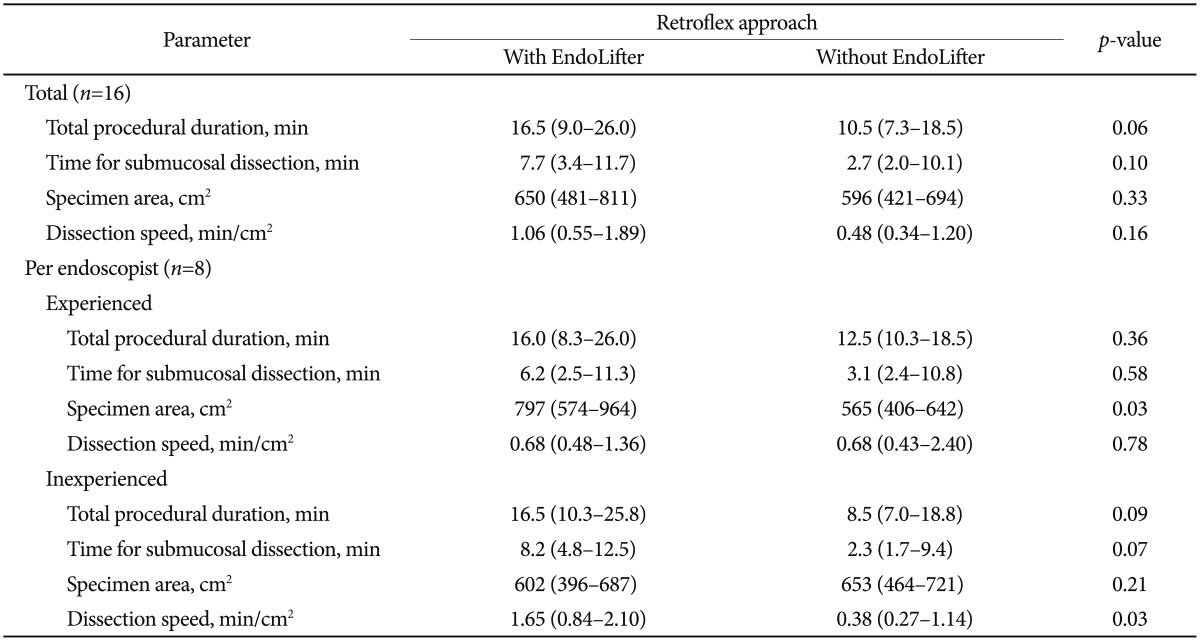
En bloc resection rate was 98.4%. In the forward approach, the median SDT was shorter with the EndoLifter (0.56 min/cm2 vs. 0.91 min/cm2), although not significantly (p=0.09). The ESD-experienced endoscopist benefitted more from the EndoLifter (0.45 [EL+] min/cm2 vs. 0.68 [EL-] min/cm2, p=0.07) than the ESD-inexperienced endoscopist (0.77 [EL+] min/cm2 vs. 1.01 [EL-] min/cm2, p=0.48). In the retroflex approach, the median SDTs were 1.06 (EL+) and 0.48 (EL-) min/cm2 (p=0.16). The EndoLifter did not shorten the SDT for the ESD-experienced endoscopist (0.68 [EL+] min/cm2 vs. 0.68 [EL-] min/cm2, p=0.78), whereas the ESD-inexperienced endoscopist seemed hindered (1.65 [EL+] min/cm2 vs. 0.38 [EL-] min/cm2, p=0.03).
Early cancer in the gastrointestinal tract can be effectively removed by endoscopic resection. In the Western world, endoscopic mucosal resection (EMR) is generally accepted because of its simplicity and convenience.1,2 However, the indications for this technique are limited to relatively small (<2 cm) or non-scarring lesions as proper lifting into the cap is required for snare resection. Accordingly, EMR may result in piecemeal resections in large or fibrotic lesions. By contrast, endoscopic submucosal dissection (ESD), consisting of a circumferential incision of the mucosa around the target lesion followed by dissection of underlying submucosal connective tissue, may provide an en bloc resection for lesions of any size, regardless of the existence of fibrotic tissue, and produce an optimal tissue condition for histopathological assessment.3,4,5,6 ESD is a demanding technique with a higher complication rate than EMR. Accumulating clinical experience, as well as exploring ESD methods, is essential to facilitate the procedure.7 Because of the high incidence of gastric carcinomas in Eastern Asia, gastric ESD has become well established among local endoscopists, whereas in Western countries, experience with gastric ESD is limited because of the low prevalence of gastric cancer. However, esophageal and colon carcinoma are more prevalent in Western countries, and the relatively thin wall and limited luminal space to maneuver within these organs, compared with the stomach, results in a threshold for Western endoscopists to overcome regarding the learning curve for ESD.
The main difficulty in ESD is to dissect the submucosal layer. A challenge is to find the optimal plane under direct visualization, thereby diminishing the possibility of perforation or unexpected massive bleeding. To simplify submucosal dissection and make it safe, the EndoLifter (LA-202; Olympus Medical Systems Corp., Tokyo, Japan) has been developed, although only indicated for gastric ESD (Fig. 1). This traction device offers a better endoscopic view of the submucosal layer, which should lead to safe and fast dissection. Although the EndoLifter appears to be a promising tool, only one study has so far been published concerning the effects of the EndoLifter.8 The aim of this ex vivo study was to investigate whether the EndoLifter is indeed a contributing factor in the performance of ESD by analyzing its effect on the speed of submucosal dissection.
This ex vivo comparative study was conducted in the animal laboratory at the Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands. Sixteen stomachs, including the whole esophagus, were obtained from recently slaughtered domestic pigs. The stomachs were thawed at room temperature and thoroughly washed with water. Next, the stomachs were sutured onto an ESD training kit in supine position, with the esophagus tied around a bent glass tube as the place of introduction for the endoscope (Fig. 2A). The training models were covered by moistened cloths to keep them flexible and invisible to the endoscopists.
The EndoLifter device consists of a transparent hood with grasping forceps. The hood is mounted on the tip of the endoscope, with the forceps in 12 o'clock position (Fig. 1A). When the handle is pushed, the forceps proceed over the hood to grasp the tissue in the front of the endoscope (Fig. 1B). The forceps can open and close using the handle. By pulling the handle after grasping the partially dissected mucosa, the submucosal tissue can be widely exposed and clearly visualized. This counter-traction enables the endoscopist to dissect the optimal submucosal plane safely. Supplementary Video 1 (available online at http://www.e-ce.org/) demonstrates the EndoLifter.
The procedure was conducted by two endoscopists: one who had extensive clinical experience in ESD (more than 100 cases) and one who had less experience (less than 10 cases). After introduction of the endoscope (GIF 1T140; Olympus Medical Systems Corp.), markings surrounding a simulated lesion with a diameter of 3 cm were placed with the Dual Knife (KD-650L; Olympus Medical Systems Corp.), with its tip inside, in a forced coagulation mode at 40 W using the ICC 200 (ERBE Elektromedizin GmbH, Tuebingen, Germany). The surrounding submucosa of the marked lesion was injected with a preferable amount of injection fluid (1.5 mL hydroxypropyl methylcellulose 3 mg/mL in 10 mL saline with a drop of indigo carmine) followed by a circumferential mucosal incision with the Dual Knife or Hook Knife (KD-620LR; Olympus Medical Systems Corp.), in an endocut mode at effect 3 and 80/40 W, along a line 5 mm outside the markings. Thereafter, submucosal dissection was performed with those knives in a forced coagulation mode at 50 W, with or without help of the EndoLifter. A resected specimen was retrieved with the endoscope by suctioning and then stretched and pinned down on a paraffin board to measure dimensions. Four lesions were created per stomach: two lesions at the posterior wall of the body for the forward approach and two lesions at the lesser curvature of the body for the retroflex approach (Fig. 2B). For each approach, one lesion was dissected with and one without the EndoLifter. The order of ESD for the four conditions was randomly assigned. Per endoscopist, 32 submucosal dissections were performed in a total of eight stomachs (Fig. 3).
For each approach, the primary outcome parameter was the difference in dissection speed (procedural duration per unit area for submucosal dissection) with or without the EndoLifter in each group. Procedural duration for submucosal dissection (min) was defined as the duration from the point of starting a submucosal dissection, after circumferential mucosal incision, to the point of detachment of the lesion. The surface size (cm2) of the resected specimen was calculated as an ellipse: half of the measured length times half of the measured width multiplied by pi (3.14). Accordingly, the dissection speed was calculated in min/cm2.
As a secondary outcome parameter for each approach, the rates of en bloc resection and perforation were analyzed.
To our knowledge, no data were available on the influence of the EndoLifter on submucosal dissection speed at the start of this experiment; therefore, no power calculation was performed. The forward and retroflex approaches were considered two distinct categories in this experiment and were analyzed as two separate datasets. For descriptive statistics, the median with interquartile range was used for variables with a skewed distribution. Because two ESDs per approach (one with EndoLifter, one without EndoLifter) were performed per stomach, and stomach-related conditions such as ease of insufflation and tissue elasticity may have been of influence, paired analysis was performed using the Wilcoxon signed-rank test. Statistical analysis was performed with the SPSS version 20.0.0.1 (IBM Co., Armonk, NY, USA).
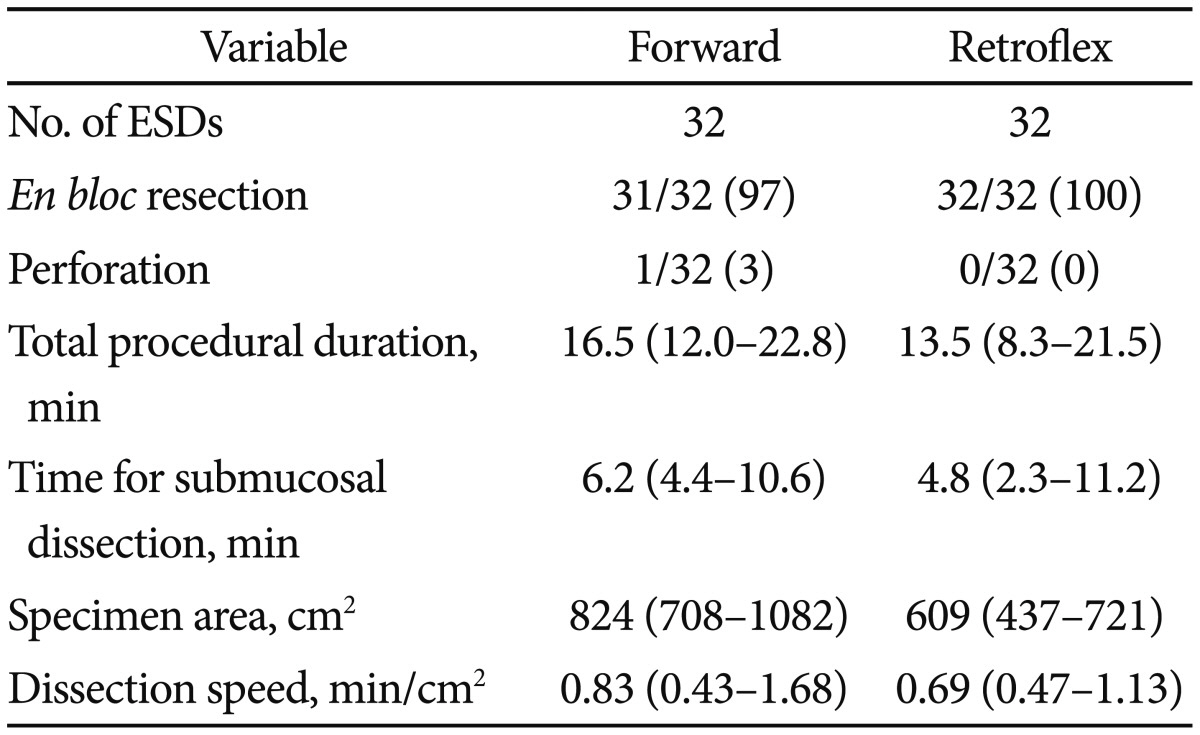
Data of all lesions, per approach, regardless of use of the EndoLifter, are listed in Table 1. En bloc resection rate was 98.4% (63/64 cases). In one case (with EndoLifter), the lesion was resected in two pieces. Perforation occurred in one case with the EndoLifter (1.6%) in forward view. The perforation was clipped and did not affect further en bloc resection.
In the forward approach (i.e., ESD at the posterior wall), the EndoLifter shortened the time for submucosal dissection, especially when correcting for the size of the resected lesion (0.56 min/cm2 vs. 0.91 min/cm2), but this did not reach statistical significance (p=0.09). The more experienced endoscopist seemed to benefit more from the EndoLifter in the forward approach compared with the less experienced endoscopist (p=0.07 vs. p=0.48, respectively) (Table 2).
In contrast to the trend seen with the forward approach, in the retroflex approach (i.e., ESD at lesser curvature), the EndoLifter seemed to prolong the procedure times. Although not statistically significant, the speed for submucosal dissection was 1.06 min/cm2 with EL vs. 0.48 min/cm2 without EndoLifter (p=0.16) (Table 3). Remarkably, in this approach, the less experienced endoscopist showed prolonged procedure times with use of the EndoLifter (1.65 min/cm2 with EndoLifter vs. 0.38 min/cm2 without EndoLifter, p=0.03), whereas the corrected submucosal dissection time (SDT) of the more experienced endoscopist did not seem to be affected at all.
This is the first report to directly demonstrate the effects of the EndoLifter on the time needed for ESD. In our ex vivo study, we observed that the EndoLifter, in trend, may be beneficial for gastric ESD in the forward approach but not in the retroflex approach.
The EndoLifter was invented to facilitate submucosal dissection and has already been commercially introduced. During the ESD procedure, a long time is needed to dissect the submucosa beneath a lesion when it is not well exposed, and submucosal dissection under poor visualization could lead to unexpected complications, such as perforation or massive bleeding from a large vessel. The EndoLifter is, therefore, expected to be helpful for achieving an easy and safe procedure in a short time.
In the forward approach, submucosal dissection sometimes becomes difficult as the procedure proceeds because of suboptimal exposure of the submucosa. In addition, in certain areas of the stomach, such as the greater curvature, submucosal dissection is hampered by the more perpendicular position of the endoscope to the gastric wall (as opposed to the safer parallel position), which can lead to perforation. The EndoLifter enables the hidden submucosa to be exposed by flipping over the partially dissected mucosa. In this study, the submucosa was dissected more rapidly, in trend, as hypothesized, yet no statistical difference was reached.
In contrast to the forward approach, the EndoLifter seemed ineffective in the retroflex approach. Two possible explanations for this are restricted maneuverability and redundancy of the EndoLifter. In the ESD procedure, the retroflex approach stabilizes the endoscope, which can be helpful during ESD but which might impair the maneuverability of the EndoLifter. In addition, once the mucosa has been grabbed by the EndoLifter, the movement of the endoscope is severely limited under the condition of full angulation. Secondly, in a lesion located on the lesser curvature, gravity will help open up the submucosal space, whereas in a lesion on the posterior wall, gravity is counteractive.
We expected the less experienced endoscopist to benefit most from the EndoLifter. However, remarkably, we found the more experienced endoscopist to profit most, though not significantly, from the EndoLifter in the forward approach. Moreover, in the retroflex approach, the less experienced endoscopist seemed to struggle with the EndoLifter, resulting in a prolonged SDT. Skillfulness is required for ESD, especially in the handling of endoscopic knives such as the Dual Knife. The same may hold true for the EndoLifter as an endoscopic device, which may explain why the more experienced endoscopist benefitted from the EndoLifter in the forward approach, and the less experienced endoscopist struggled with the retroflex approach. Secondly, the difference in usefulness of the EndoLifter between endoscopists, experienced or novice in ESD, was a secondary outcome parameter that was assessed in only two endoscopists. Further studies with multiple endoscopists will generate more solid data concerning this matter.
Teoh et al.8 reported the usefulness of the EndoLifter in an ex vivo porcine model, showing that the EndoLifter could obtain a good view of the submucosa, especially in the forward approach, which is consistent with our results. However, in contrast to the surrogate markers used to measure the usefulness of the EndoLifter by Teoh et al.,8 the more clinically orientated dissection speed was scored as a primary outcome measurement in our study. Furthermore, we performed a larger number of cases in a more clinically relevant model.
Other techniques for creating counter-traction during gastric ESD have been introduced, and some of these have already been published. These methods are roughly divided into two groups on the basis of whether or not a grasping point is stabilized. In the first group, a clip is mainly used to create counter-traction, accompanied by a sinker,9 string,10,11,12 magnet,13 or spring.14 In the second group, counter-traction is accomplished with grasping forceps detached/attached to the endoscope15,16 or introduced from a double-channel endoscope,17 transanal/nasal thin endoscope,18,19 or percutaneous trocar.20 Each method has merits and demerits. Using a clip is simple but presents some difficulty in controlling the counter-traction because the direction of traction is limited. Using a grasping forceps is a more flexible way to create counter-traction, but difficulties may arise in handling the forceps itself.
The present study has some limitations. First, no sample size calculation was performed, and the number of lesions per group was small. This may have resulted in certain trends instead of significant differences. Secondly, gravity might have been a confounding factor. Because of the training kit used in our study, the stomachs were placed in the supine position, which is different from the usual left lateral decubitus position in clinical practice. With the stomach in supine position, the ESD procedures at the lesser curvature (retroflex approach) were facilitated by the effects of gravity on the mucosal flap, rendering a traction device possibly less useful. In the ESD procedures at the posterior wall (forward approach), however, the submucosal space was not exposed by the effect of gravity, making a traction device more useful. This might be an additional reason why the EndoLifter appeared to be more useful in the forward approach. Thirdly, the use of isolated stomachs in this ex vivo study carries certain limitations. The EndoLifter aims for a quicker and safer ESD. In an ex vivo model, the absence of motility and breathing makes assessment of true feasibility and efficacy difficult. Moreover, we could not assess the feasibility of the EndoLifter in case of bleeding, and though no difference in perforations was observed, the ex vivo model is not truly suitable for safety assessment. Finally, the number of participating endoscopists was small although the number of resected lesions per endoscopist was acceptably large.
In conclusion, in this ex vivo porcine model, we observed that the EndoLifter did not significantly contribute to the acceleration of dissection speed during gastric ESD although a trend was seen towards a faster ESD in the forward approach by the ESD expert endoscopist. However, the limitations of this study made it difficult to truly assess the efficacy of the EndoLifter in a clinical situation. Thus, an in vivo trial would be desirable.
References
1. Pouw RE, Bergman JJ. Endoscopic resection of early oesophageal and gastric neoplasia. Best Pract Res Clin Gastroenterol. 2008; 22:929–943. PMID: 18790439.

2. Ribeiro-Mourão F, Pimentel-Nunes P, Dinis-Ribeiro M. Endoscopic submucosal dissection for gastric lesions: results of an European inquiry. Endoscopy. 2010; 42:814–819. PMID: 20886399.

3. Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001; 48:225–229. PMID: 11156645.

4. Yamamoto H, Kawata H, Sunada K, et al. Successful en-bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy. 2003; 35:690–694. PMID: 12929067.

5. Oyama T, Tomori A, Hotta K, et al. Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol. 2005; 3(7 Suppl 1):S67–S70. PMID: 16013002.

6. Yahagi N, Uraoka T, Ida Y, et al. Endoscopic submucosal dissection using the Flex and the Dual knives. Tech Gastrointest Endosc. 2011; 13:74–78.

7. Deprez PH, Bergman JJ, Meisner S, et al. Current practice with endoscopic submucosal dissection in Europe: position statement from a panel of experts. Endoscopy. 2010; 42:853–858. PMID: 20623442.

8. Teoh AY, Chiu PW, Hon SF, Mak TW, Ng EK, Lau JY. Ex vivo comparative study using the Endolifter(R) as a traction device for enhancing submucosal visualization during endoscopic submucosal dissection. Surg Endosc. 2013; 27:1422–1427. PMID: 23093235.
9. Saito Y, Emura F, Matsuda T, et al. A new sinker-assisted endoscopic submucosal dissection for colorectal cancer. Gastrointest Endosc. 2005; 62:297–301. PMID: 16046999.

10. Chen PJ, Chu HC, Chang WK, Hsieh TY, Chao YC. Endoscopic submucosal dissection with internal traction for early gastric cancer (with video). Gastrointest Endosc. 2008; 67:128–132. PMID: 18054010.

11. Jeon WJ, You IY, Chae HB, Park SM, Youn SJ. A new technique for gastric endoscopic submucosal dissection: peroral traction-assisted endoscopic submucosal dissection. Gastrointest Endosc. 2009; 69:29–33. PMID: 19111686.

12. Li CH, Chen PJ, Chu HC, et al. Endoscopic submucosal dissection with the pulley method for early-stage gastric cancer (with video). Gastrointest Endosc. 2011; 73:163–167. PMID: 21030018.

13. Gotoda T, Oda I, Tamakawa K, Ueda H, Kobayashi T, Kakizoe T. Prospective clinical trial of magnetic-anchor-guided endoscopic submucosal dissection for large early gastric cancer (with videos). Gastrointest Endosc. 2009; 69:10–15. PMID: 18599053.

14. Sakamoto N, Osada T, Shibuya T, et al. Endoscopic submucosal dissection of large colorectal tumors by using a novel spring-action S-O clip for traction (with video). Gastrointest Endosc. 2009; 69:1370–1374. PMID: 19403131.

15. Imaeda H, Iwao Y, Ogata H, et al. A new technique for endoscopic submucosal dissection for early gastric cancer using an external grasping forceps. Endoscopy. 2006; 38:1007–1010. PMID: 16673308.

16. Motohashi O, Nishimura K, Nakayama N, Takagi S, Yanagida N. Endoscopic submucosal dissection (two-point fixed ESD) for early esophageal cancer. Dig Endosc. 2009; 21:176–179. PMID: 19691765.

17. Yonezawa J, Kaise M, Sumiyama K, Goda K, Arakawa H, Tajiri H. A novel double-channel therapeutic endoscope ("R-scope") facilitates endoscopic submucosal dissection of superficial gastric neoplasms. Endoscopy. 2006; 38:1011–1015. PMID: 17058166.

18. Uraoka T, Kato J, Ishikawa S, et al. Thin endoscope-assisted endoscopic submucosal dissection for large colorectal tumors (with videos). Gastrointest Endosc. 2007; 66:836–839. PMID: 17905031.

19. Ahn JY, Choi KD, Choi JY, et al. Transnasal endoscope-assisted endoscopic submucosal dissection for gastric adenoma and early gastric cancer in the pyloric area: a case series. Endoscopy. 2011; 43:233–235. PMID: 21165828.

20. von Delius S, Karagianni A, von Weyhern CH, et al. Percutaneously assisted endoscopic surgery using a new PEG-minitrocar for advanced endoscopic submucosal dissection (with videos). Gastrointest Endosc. 2008; 68:365–369. PMID: 18561928.

Fig. 1
The EndoLifter (Olympus). (A) The EndoLifter mounted on the tip of an endoscope. (B) Grasping forceps proceeding forward over the tip of the endoscope and opening.
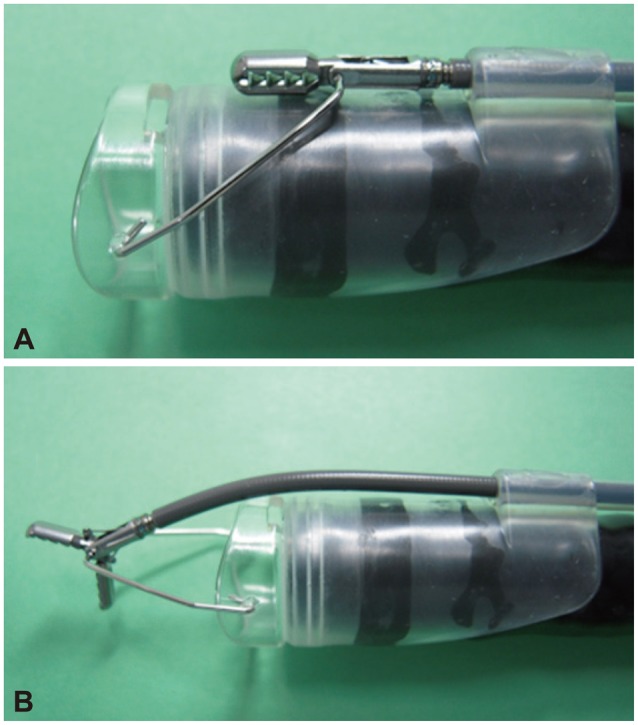
Fig. 2
Experimental set-up. (A) A training kit and the EndoLifter (Olympus). A porcine stomach with the esophagus in a training model, tied with sutures and a glass loop. (B) Per stomach, four artificial lesions (3 cm) are created: I and II at the lesser curvature (retroflex approach) and III and IV at the posterior wall (forward approach).
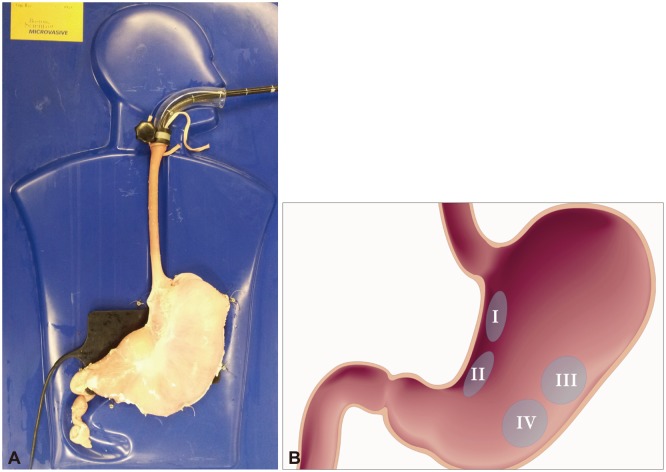
Table 1
Outcomes for Endoscopic Submucosal Dissection on Isolated Porcine Stomachs per approach (i.e., Forward or Retroflex Approach)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download