1. Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, et al. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2013; 28:593–607. PMID:
23350673.

2. Deoliveira ML, Schulick RD, Nimura Y, et al. New staging system and a registry for perihilar cholangiocarcinoma. Hepatology. 2011; 53:1363–1371. PMID:
21480336.

3. Bismuth H. Surgical anatomy and anatomical surgery of the liver. World J Surg. 1982; 6:3–9. PMID:
7090393.

4. Dowsett JF, Vaira D, Hatfield AR, et al. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology. 1989; 96:1180–1186. PMID:
2925062.

5. Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010; 72:728–735. PMID:
20883850.

6. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001; 53:547–553. PMID:
11323577.

7. Naitoh I, Ohara H, Nakazawa T, et al. Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009; 24:552–557. PMID:
19220678.

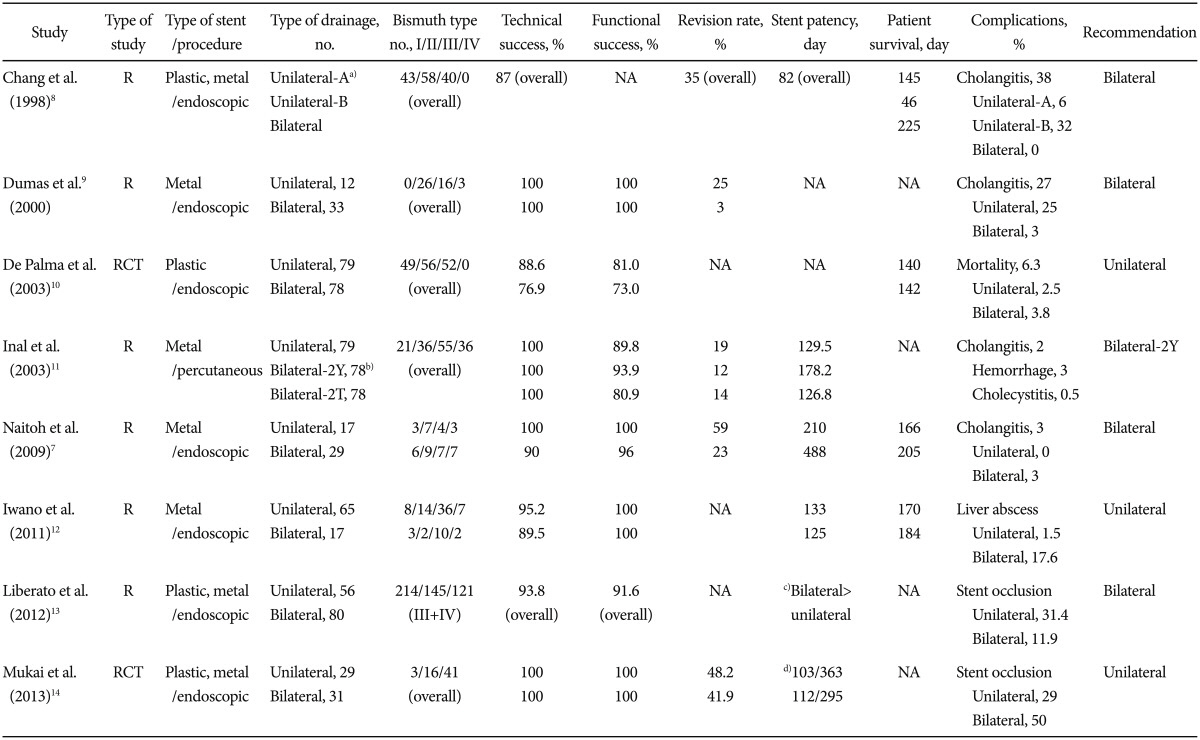
8. Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998; 47:354–362. PMID:
9609426.

9. Dumas R, Demuth N, Buckley M, et al. Endoscopic bilateral metal stent placement for malignant hilar stenoses: identification of optimal technique. Gastrointest Endosc. 2000; 51:334–338. PMID:
10699784.

10. De Palma GD, Pezzullo A, Rega M, et al. Unilateral placement of metallic stents for malignant hilar obstruction: a prospective study. Gastrointest Endosc. 2003; 58:50–53. PMID:
12838220.

11. Inal M, Akgül E, Aksungur E, Seydaoğlu G. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol. 2003; 14:1409–1416. PMID:
14605106.

12. Iwano H, Ryozawa S, Ishigaki N, et al. Unilateral versus bilateral drainage using self-expandable metallic stent for unresectable hilar biliary obstruction. Dig Endosc. 2011; 23:43–48.

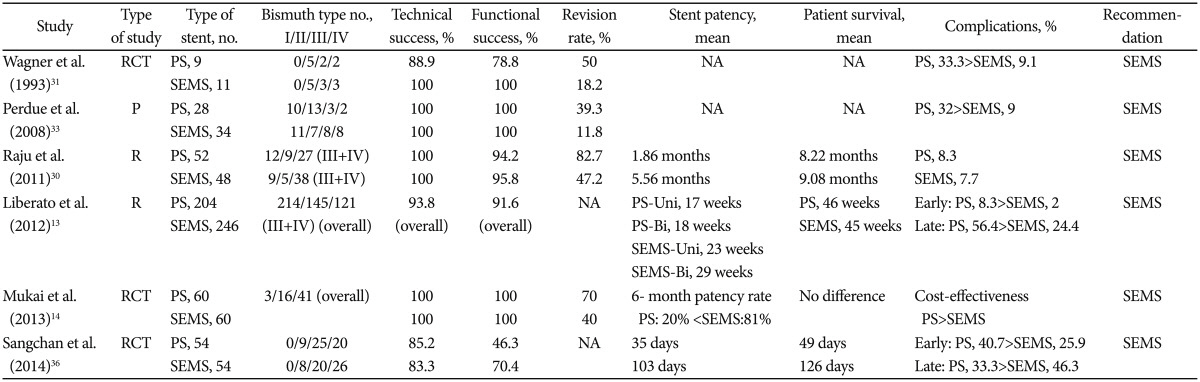
13. Liberato MJ, Canena JM. Endoscopic stenting for hilar cholangiocarcinoma: efficacy of unilateral and bilateral placement of plastic and metal stents in a retrospective review of 480 patients. BMC Gastroenterol. 2012; 12:103. PMID:
22873816.

14. Mukai T, Yasuda I, Nakashima M, et al. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013; 20:214–222. PMID:
22415652.

15. Ertuğrul I, Yüksel I, Parlak E, et al. Risk factors for endoscopic retrograde cholangiopancreatography-related cholangitis: a prospective study. Turk J Gastroenterol. 2009; 20:116–121. PMID:
19530044.
16. Hanninen EL, Pech M, Jonas S, et al. Magnetic resonance imaging including magnetic resonance cholangiopancreatography for tumor localization and therapy planning in malignant hilar obstructions. Acta Radiol. 2005; 46:462–470. PMID:
16224919.

17. Freeman ML, Overby C. Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with self-expanding metallic stents. Gastrointest Endosc. 2003; 58:41–49. PMID:
12838219.

18. Lopera JE, Soto JA, Múnera F. Malignant hilar and perihilar biliary obstruction: use of MR cholangiography to define the extent of biliary ductal involvement and plan percutaneous interventions. Radiology. 2001; 220:90–96. PMID:
11425978.

19. Masselli G, Manfredi R, Vecchioli A, Gualdi G. MR imaging and MR cholangiopancreatography in the preoperative evaluation of hilar cholangiocarcinoma: correlation with surgical and pathologic findings. Eur Radiol. 2008; 18:2213–2221. PMID:
18463877.

20. Zidi SH, Prat F, Le Guen O, Rondeau Y, Pelletier G. Performance characteristics of magnetic resonance cholangiography in the staging of malignant hilar strictures. Gut. 2000; 46:103–106. PMID:
10601064.

21. Bae JI, Park AW, Choi SJ, et al. Crisscross-configured dual stent placement for trisectoral drainage in patients with advanced biliary hilar malignancies. J Vasc Interv Radiol. 2008; 19:1614–1619. PMID:
18823794.

22. Ridtitid W, Rerknimitr R, Janchai A, Kongkam P, Treeprasertsuk S, Kullavanijaya P. Outcome of second interventions for occluded metallic stents in patients with malignant biliary obstruction. Surg Endosc. 2010; 24:2216–2220. PMID:
20177930.

23. Kim JY, Kang DH, Kim HW, et al. Usefulness of slimmer and open-cell-design stents for endoscopic bilateral stenting and endoscopic revision in patients with hilar cholangiocarcinoma (with video). Gastrointest Endosc. 2009; 70:1109–1115. PMID:
19647244.

24. Kogure H, Isayama H, Nakai Y, et al. Newly designed large cell Niti-S stent for malignant hilar biliary obstruction: a pilot study. Surg Endosc. 2011; 25:463–467. PMID:
20602139.

25. Köklü S, Koçak E, Akbal E. Air cholangiography for severe hilar obstruction at ERCP. Gastrointest Endosc. 2011; 73:1326. PMID:
21628021.

26. Kato H, Kawamoto H, Noma Y, et al. Dilatation by Soehendra stent retriever is feasible and effective in multiple deployment of metallic stents to malignant hilar biliary strictures. Hepatogastroenterology. 2013; 60:286–290. PMID:
23858539.
27. Kim JY, Kang DH, Choi CW, Kim HW, Park SB, Kim DU. Selective intrahepatic duct cannulation by using a triple-lumen catheter for endoscopic bilateral stenting in hilar cholangiocarcinoma. Gastrointest Endosc. 2010; 72:192–198. PMID:
20546732.

28. Pisello F, Geraci G, Modica G, Sciumè C. Cholangitis prevention in endoscopic Klatskin tumor palliation: air cholangiography technique. Langenbecks Arch Surg. 2009; 394:1109–1114. PMID:
19707784.

29. Sud R, Puri R, Choudhary NS, Mehta A, Jain PK. Air cholangiogram is not inferior to dye cholangiogram for malignant hilar biliary obstruction: a randomized study of efficacy and safety. Indian J Gastroenterol. 2014; 33:537–542. PMID:
25616350.

30. Raju RP, Jaganmohan SR, Ross WA, et al. Optimum palliation of inoperable hilar cholangiocarcinoma: comparative assessment of the efficacy of plastic and self-expanding metal stents. Dig Dis Sci. 2011; 56:1557–1564. PMID:
21222156.

31. Wagner HJ, Knyrim K, Vakil N, Klose KJ. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy. 1993; 25:213–218. PMID:
7686100.

32. Kim JH. Endoscopic stent placement in the palliation of malignant biliary obstruction. Clin Endosc. 2011; 44:76–86. PMID:
22741117.

33. Perdue DG, Freeman ML, DiSario JA, et al. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J Clin Gastroenterol. 2008; 42:1040–1046. PMID:
18719507.
34. Goenka MK, Goenka U. Palliation: hilar cholangiocarcinoma. World J Hepatol. 2014; 6:559–569. PMID:
25232449.

35. Kaneko T, Sugimori K, Shimizu Y, et al. Efficacy of plastic stent placement inside bile ducts for the treatment of unresectable malignant hilar obstruction (with videos). J Hepatobiliary Pancreat Sci. 2014; 21:349–355. PMID:
24123806.

36. Sangchan A, Chaiyakunapruk N, Supakankunti S, Pugkhem A, Mairiang P. Cost utility analysis of endoscopic biliary stent in unresectable hilar cholangiocarcinoma: decision analytic modeling approach. Hepatogastroenterology. 2014; 61:1175–1181.
37. Hookey LC, Le Moine O, Deviere J. Use of a temporary plastic stent to facilitate the placement of multiple self-expanding metal stents in malignant biliary hilar strictures. Gastrointest Endosc. 2005; 62:605–609. PMID:
16185978.

38. Cheng JL, Bruno MJ, Bergman JJ, Rauws EA, Tytgat GN, Huibregtse K. Endoscopic palliation of patients with biliary obstruction caused by nonresectable hilar cholangiocarcinoma: efficacy of self-expandable metallic Wallstents. Gastrointest Endosc. 2002; 56:33–39. PMID:
12085032.

39. Chennat J, Waxman I. Initial performance profile of a new 6F self-expanding metal stent for palliation of malignant hilar biliary obstruction. Gastrointest Endosc. 2010; 72:632–636. PMID:
20579991.

40. Lee TH, Park do H, Lee SS, et al. Technical feasibility and revision efficacy of the sequential deployment of endoscopic bilateral side-by-side metal stents for malignant hilar biliary strictures: a multicenter prospective study. Dig Dis Sci. 2013; 58:547–555. PMID:
22886596.

41. Lee JH, Kang DH, Kim JY, et al. Endoscopic bilateral metal stent placement for advanced hilar cholangiocarcinoma: a pilot study of a newly designed Y stent. Gastrointest Endosc. 2007; 66:364–369. PMID:
17643714.
42. Park do H, Lee SS, Moon JH, et al. Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: multicenter prospective feasibility study (with videos). Gastrointest Endosc. 2009; 69:1357–1360. PMID:
19481654.
43. Chahal P, Baron TH. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest Endosc. 2010; 71:195–199. PMID:
19945101.

44. Kawamoto H, Tsutsumi K, Fujii M, et al. Endoscopic 3-branched partial stent-in-stent deployment of metallic stents in high-grade malignant hilar biliary stricture (with videos). Gastrointest Endosc. 2007; 66:1030–1037. PMID:
17963891.
45. Hwang JC, Kim JH, Lim SG, Kim SS, Yoo BM, Cho SW. Y-shaped endoscopic bilateral metal stent placement for malignant hilar biliary obstruction: prospective long-term study. Scand J Gastroenterol. 2011; 46:326–332. PMID:
21082874.

46. Lee TH, Moon JH, Kim JH, et al. Primary and revision efficacy of cross-wired metallic stents for endoscopic bilateral stent-in-stent placement in malignant hilar biliary strictures. Endoscopy. 2013; 45:106–113. PMID:
23212727.

47. Naitoh I, Nakazawa T, Ban T, et al. 8-mm versus 10-mm diameter self-expandable metallic stent in bilateral endoscopic stent-in-stent deployment for malignant hilar biliary obstruction. J Hepatobiliary Pancreat Sci. 2015; 22:396–401. PMID:
25611012.

48. Naitoh I, Hayashi K, Nakazawa T, et al. Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci. 2012; 57:3279–3285. PMID:
22732832.

49. Paik WH, Park YS, Hwang JH, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009; 69:55–62. PMID:
18657806.

50. Kim CW, Park AW, Won JW, Kim S, Lee JW, Lee SH. T-configured dual stent placement in malignant biliary hilar duct obstructions with a newly designed stent. J Vasc Interv Radiol. 2004; 15:713–717. PMID:
15231885.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download