This article has been
cited by other articles in ScienceCentral.
Abstract
Peripheral facial nerve palsy (FNP) is a mononeuropathy that affects the peripheral part of the facial nerve. Primary causes of peripheral FNP remain largely unknown, but detectable causes include systemic infections (viral and others), trauma, ischemia, tumor, and extrinsic compression. Peripheral FNP in relation to extrinsic compression has rarely been described in case reports. Here, we report a case of a 71-year-old man who was diagnosed with peripheral FNP following endoscopic submucosal dissection. This case is the first report of the development of peripheral FNP in a patient undergoing therapeutic endoscopy. We emphasize the fact that physicians should be attentive to the development of peripheral FNP following therapeutic endoscopy.
Go to :

Keywords: Facial paralysis, Compression, Endoscopy
INTRODUCTION
Peripheral facial nerve palsy (FNP) can result from idiopathic (primary) or detectable (secondary) causes. Secondary causes include systemic viral or other infections, trauma, ischemia, tumor, and extrinsic compression.
1 However, secondary FNP by external compression has rarely been reported.
2,
3,
4,
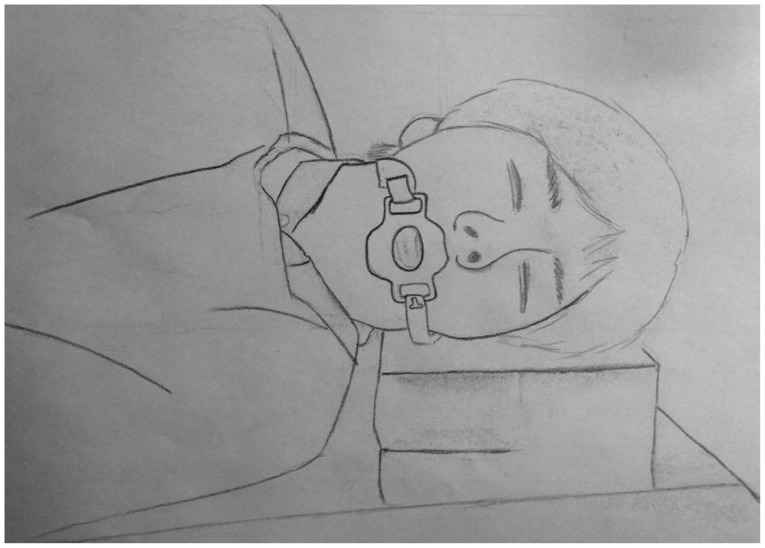
5 Therapeutic endoscopy lasts significantly longer than diagnostic endoscopy, and therefore, the left facial nerve may be compressed by the pillow and mouth piece band during the procedure (
Fig. 1). We encountered a very rare complication of peripheral FNP during therapeutic endoscopy. The purpose of this report is to alert physicians to this possibility. For prophylaxis, the mouth piece band should not be too tight and a soft pillow should be replaced with the hard pillow currently used.
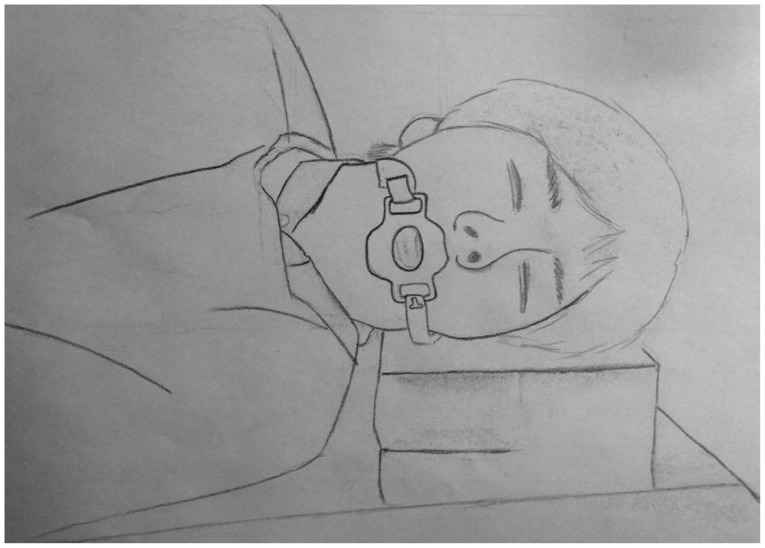 | Fig. 1The patient is in the left lateral decubitus position on the hard pillow during endoscopic submucosal dissection. The mouthpiece is fixed with a rubber band. The left facial nerve may be compressed by the hard pillow or mouthpiece band.
|
Go to :

CASE REPORT
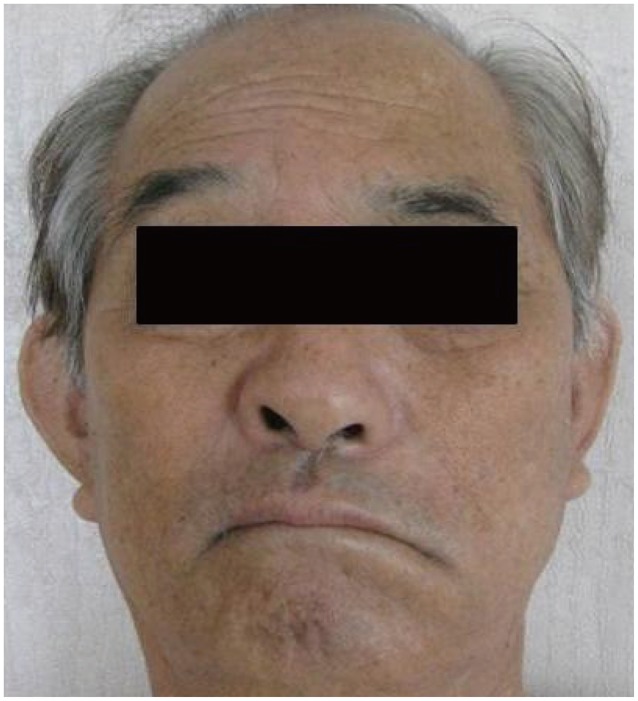
A 71-year-old man underwent endoscopic screening of the upper gastrointestinal tract. He had no previous medical illness. The endoscopy showed a 3-cm, slightly elevated, discolored lesion at the greater curvature side of the antrum, so a biopsy was performed. Biopsy of this region revealed low-grade dysplasia. Our treatment plan consisted of endoscopic submucosal dissection (ESD) using an insulation-tipped knife (KD-610L; Olympus, Tokyo, Japan). ESD was performed under deep sedation with midazolam and propofol. Initially, the endoscopist administered 2.5 mg (0.03 mg/kg) of midazolam and 50 mg of propofol intravenously. Depending on the consciousness state of the patient, the endoscopist added 20 mg of propofol. The total administered dosage was 2.5 mg of midazolam and 170 mg of propofol. On the first day, the ESD procedure lasted 40 minutes, and no complications were observed. On the next day, the patient complained of left facial weakness. On physical examination, the patient showed inability to wrinkle the forehead, eyebrow sagging, disappearance of the nasolabial fold, and drooling at the left corner of the mouth (
Fig. 2). Blink reflex revealed complete left peripheral FNP (
Fig. 3). Symptoms and signs suggestive of viral infections such as parotid gland pain, cough, myalgia, febricity, and skin vesicle lesion were not present. Furthermore, there were no findings of mass or stroke on magnetic resonance imaging (MRI). Therefore, direct compression by the pillow and the mouthpiece band during endoscopy was suggested as the cause of peripheral FNP. Following 2 weeks of conservative treatment, the FNP completely resolved, and the patient remained without recurrence at the follow-up.
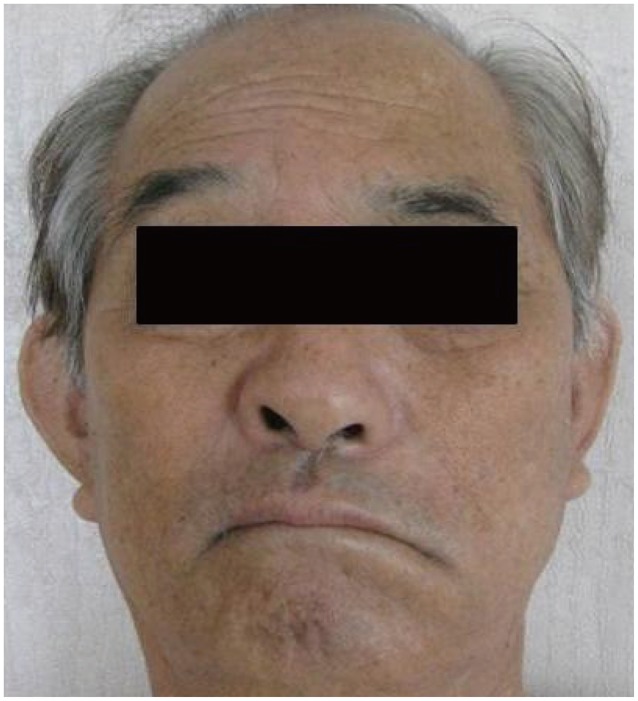 | Fig. 2Patient showing left side peripheral facial nerve palsy with inability to wrinkle the forehead, eyebrow sagging, disappearance of the nasolabial fold, and drooling at the left corner of the mouth.
|
 | Fig. 3Blink reflex test. Ipsilateral R1 and R2 were absent upon left-side stimulation, whereas contralateral R2 was present. Ipsilateral R1 and R2 were present upon right-side stimulation, whereas contralateral R2 was absent. These findings are consistent with peripheral facial nerve palsy. (A) Left-side stimulation. (B) Right-side stimulation.
|
Go to :

DISCUSSION
Peripheral FNP may arise from a detectable cause (secondary FNP) or from an idiopathic cause (primary FNP). Secondary peripheral FNP is generally less prevalent than primary FNP (25% vs. 75%).
6 Secondary FNP caused by external compression has rarely been reported.
2,
3,
4 The facial nerve is a primary motor nerve with a small sensorial component; it emerges at the stylomastoid foramen, turns anterolaterally, and passes through the parotid gland. Five groups of the nerve emerge from the parotid gland and are distributed to the facial muscles in a complex pattern.
7 Hence, the facial nerve can be subject to extrinsic compression, at the parotid gland level by the mouth piece band and pillow during endoscopy in the left lateral decubitus position. In addition, because therapeutic endoscopy requires longer than diagnostic endoscopy, it is a possible risk factor for secondary peripheral FNP by extrinsic compression.
Peripheral FNP is diagnosed based on typical clinical features and the blink reflex test. A brain MRI, exhaustive medical history, and careful physical examinations are required to confirm causality. In our case, the brain MRI was inconclusive, and physical examination that was suggestive of viral infection revealed no small blisters or vesicles on the external hearing disturbances. The patient developed FNP following ESD but rapidly, fully recovered with only conservative treatment. Therefore, extrinsic compression is suggested as the cause of peripheral FNP. Although treatment of FNP is still controversial, empirically antiviral agents and corticosteroids have been successfully administered.
6,
8,
9,
10,
11 In this case, clinical findings that are suggestive of viral infection were non-existent, and corticosteroid treatment was not prescribed due to bleeding risk. Previous reports on peripheral FNP caused by external compression showed complete recovery within few days or months using only conservative treatment without special treatment in most cases.
2,
3,
4 The patient in our case presented had rapid and complete recovery with conservative treatment without any antiviral agents or corticosteroids.
The prognosis of FNP is relatively favorable, with approximately 80% to 85% of patients recovering spontaneously and completely, and only 15% to 20% of patients experiencing some permanent nerve damage.
1 Prognosis of FNP should be based on the clinical assessment using nerve conduction studies 2 to 3 weeks following diagnosis.
1 Long-term sequelae of FNP may include weakness, contractures, facial spasms, synkinesis, decreased tears, or psychosocial effects.
6
In conclusion, we report the first case of peripheral FNP developed following therapeutic endoscopy. There are two points arising from this case report that we would like to highlight. First, physicians should be aware of the possibility of development of peripheral FNP following therapeutic endoscopy and should inform patients of the possible side effects and that complete recovery is possible with adequate treatment. Second, the mouth piece band should not be too tight, and the hard pillow should be replaced with a soft pillow during endoscopic procedure.
Further studies are required to determine the extent to which the strength or duration of the compression may contribute to FNP.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download