INTRODUCTION
CASE REPORT
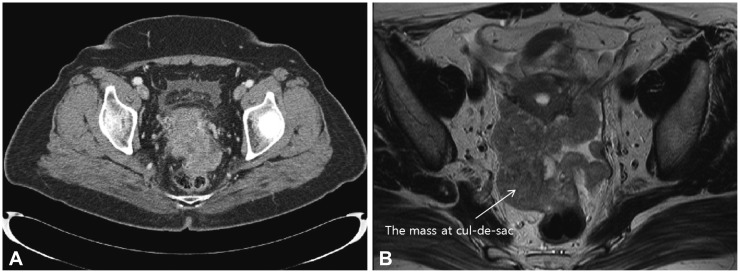 | Fig. 1Computed tomography (CT) and magnetic resonance imaging (MRI) of the adnexal mass. (A) An about 8-cm, heterogeneous enhancing mass with irregular shape, involving from the uterine cervix to the uterine fundus, was detected by using CT. (B) The mass at cul-de-sac (white arrow) has directly invaded to the rectum on MRI. |
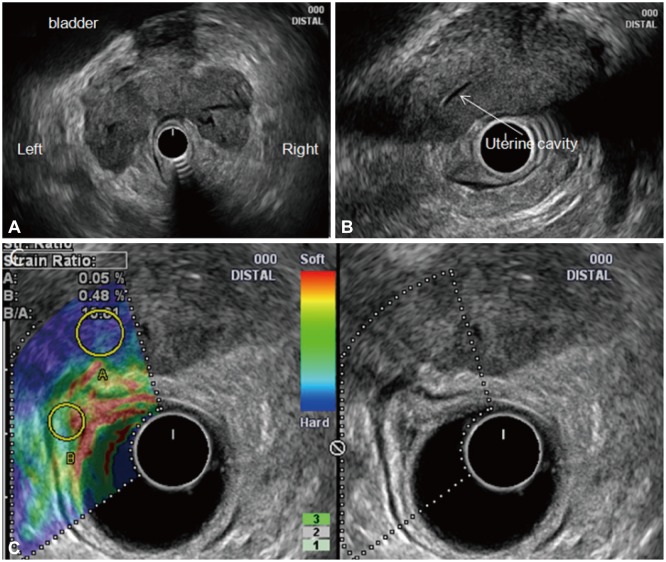 | Fig. 2Endoscopic ultrasound elastography of the adnexal mass. (A) A sausage-shaped hypoechoic mass, 8 cm in size, with irregular margins and heterogeneous internal echoes extending to both adnexa and that had obliterated the lumen of both fallopian tubes was detected. (B) The mass had invaded the right side of the uterine body, making it difficult to delineate the borderline between the lesion and the uterus. (C) Elastographic image of the left side of the dual image showing the blue color pattern (representing hard stiffness) of the mass and heterogeneous green/red coloration (representing intermediate stiffness) outside the tumor. |
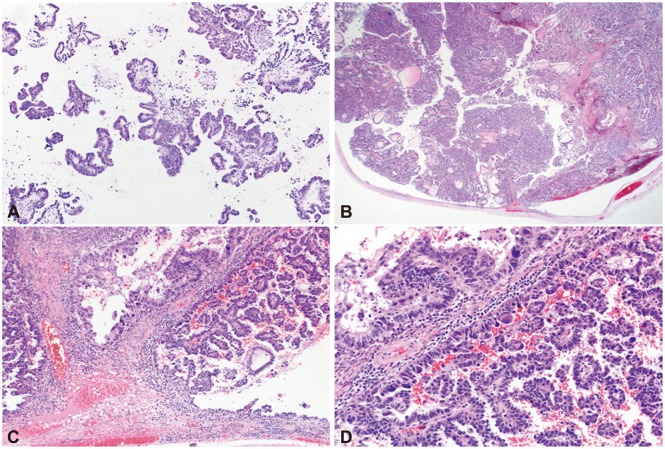 | Fig. 3Histopathologic analyses of needle biopsy and operative tissue specimens. (A) The ProCore needle biopsy specimen revealed papillary growing tumor cells with hyperchromatic nuclei and frequent mitoses, suggestive of primary or metastatic papillary adenocarcinoma of the pelvic cavity (H&E stain, ×100). (B) The operative specimen revealed a tumor occupying the lumen of the right residual fallopian tube that had extended to the pelvic cavity (H&E stain, ×12.5). (C) Operative specimen showing the tumor arising from the luminal epithelium with a papillary growth pattern (H&E stain, ×100). (D) Operative specimen showing that the tumor consisted of a fibrovascular core lined by a single layer of tumor cells with occasional pleomorphic cells and frequent atypical mitosis (H&E stain, ×200). These findings are similar to those of the endoscopic ultrasound-guided biopsy. |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download