Abstract
Esophageal thermal injury caused by food has been reported to occur mostly after drinking hot liquid food, and is known to produce alternating white and red linear mucosal bands. In addition, thermal injury caused by ingestion of hot solid foods is documented to be a cause of esophageal ulcers or pseudomembranes. From January 2006 to August 2012, five patients with suspected esophageal thermal injury underwent esophagogastroduodenoscopy with biopsy. A "candy-cane" appearance was observed in one case, pseudomembrane was observed in two cases, an esophageal ulcer was observed in one case, and a friable and edematous mucosa was noted in one case. We believe that the endoscopic findings of esophageal thermal injury depend on the following factors: causative materials, amount of food consumed, exposure period, and time to endoscopy after the incident. Therefore, physicians who encounter patients with suspected esophageal thermal injury should carefully take the patient's history considering these factors.
Go to : 
Acute esophageal thermal injury caused by food has been reported to occur mostly after drinking hot liquids or swallowing solid foods, both of which are reversible. Furthermore, it has been reported to produce alternating white and red linear mucosal bands (resembling a "candy cane"), esophageal ulcers, or pseudomembranes.1,2,3 The candy-cane appearance is a typical endoscopic feature of esophageal thermal injury caused by hot liquids.3 The exact prevalence of esophageal thermal injury is unknown; however, its occurrence may be more common in the East than in the West because of differences in food culture.
Here, we report five cases of esophageal thermal injury that presented different endoscopic findings, presumably because different foods had caused the thermal injury.
Go to : 
A 45-year-old woman was referred to us for the evaluation of hematemesis and odynophagia. She had no other gastrointestinal symptoms when she arrived at the hospital.
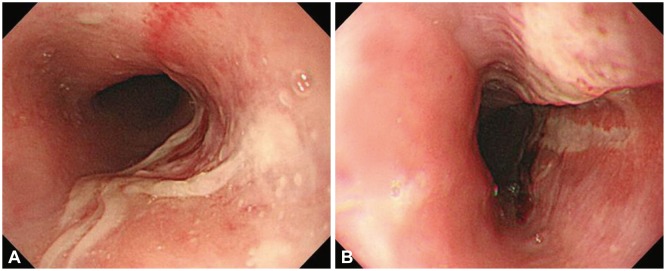
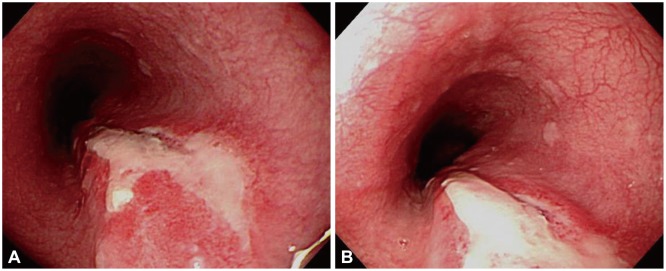
Her vital signs were stable, and the results of laboratory tests were within the reference ranges. L-tube irrigation and digital rectal examination yielded negative results. On the day of her visit, she underwent esophagogastroduodenoscopy (EGD), which found edema on the arytenoid folds. A whitish pseudomembranous mucosa of a geographic shape, which occupied about half of the esophageal lumen, was seen, and it ranged from the hypopharynx to 25 cm from the upper incisors (Fig. 1A). We questioned the patient again about her history, and she claimed that she may have experienced a sore throat after drinking hot green tea a week ago.
The patient was treated with 30 mg/day lansoprazole and 60 mg/day sucralfate, and showed clinical improvements. Seven days later, she underwent a follow-up EGD, and the previous lesion showed the candy-cane appearance (Fig. 1B). The histologic findings were ulceration with acute and chronic inflammation and epithelial atypia.
A 52-year-old man was admitted to our hospital because of burning retrosternal pain since he accidentally swallowed hot stew a week previously.
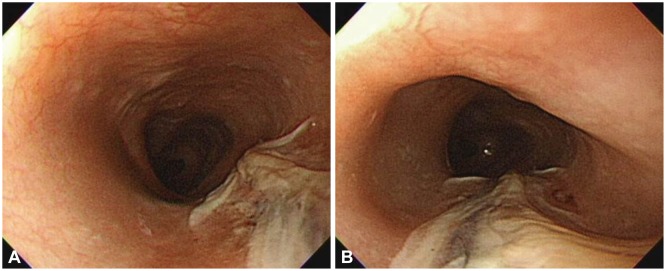
Physical examination and laboratory tests yielded unremarkable results. EGD showed a whitish pseudomembrane ranging from the proximal third of the esophagus to the distal portion, and three small erosions at 30 cm below the incisor. The size of the erosions was 1×1 cm, and the erosions had confluent whitish exudates. There was no evidence of reflux esophagitis (Fig. 2). The patient was administered with 30 mg/day ranitidine and 60 mg/day sucralfate for 3 weeks. The EGD was repeated 3 weeks later, which showed that the erosions had improved and the pseudomembrane had disappeared.
A 29-year-old man with schizophrenia experienced an auditory hallucination directing him to drink hot water, on the day of his visit to our hospital. He drank about 150 mL of hot water at once, because of which he developed a sore throat and odynophagia and was brought to the emergency room.
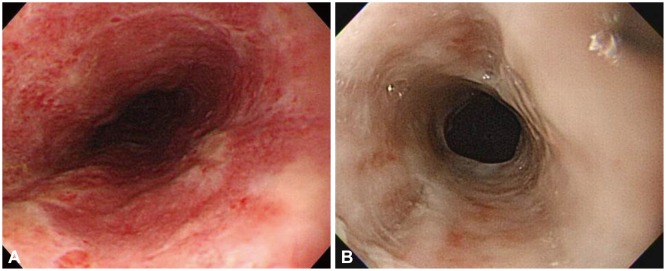
Physical examination and laboratory tests yielded unremarkable findings. EGD showed a whitish pseudomembrane that had nearly completely encircled the esophageal mucosa; the partially exposed hyperemic mucosa, from the upper and lower esophagus, easily bled on touching (Fig. 3A). Seven days later, we performed a follow-up endoscopy, which showed a hyperemic and edematous mucosa and mild whitish fibrosis on the upper and middle esophagus (Fig. 3B). This patient was also administered with 30 mg/day lansoprazole and 60 mg/day sucralfate. He was discharged on the following week with no persisting symptoms.
A 57-year-old woman was admitted to our hospital because of anemia. She has schizophrenia. A few days ago, she had drunk a glass of hot water at once but did not complain of any gastrointestinal symptoms.
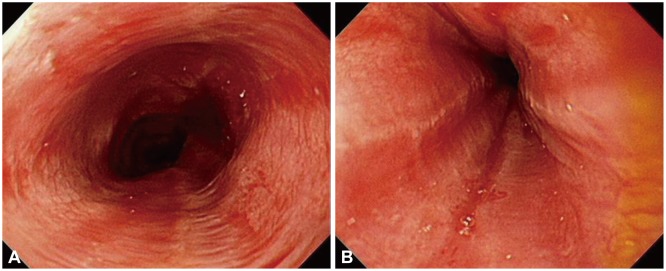
The laboratory results were as follows: hemoglobin, 8.5 g/dL (reference, 13 to 16); hematocrit, 25.5% (reference, 39 to 52). Other laboratory results were within the reference ranges, and no specific cause of the anemia was found. EGD showed a whitish pseudomembrane in the oral cavity and esophagus. In addition, from the lower esophagus, the mucosa was edematous, hemorrhagic, and corrosive, and it easily bled on touching (Fig. 4). This patient was also administered with 30 mg/day lansoprazole and 60 mg/day sucralfate. She was discharged a week later with no adverse events and with improvements in the condition of the esophageal mucosa.
A 54-year-old man presented with odynophagia after swallowing a steamed egg while intoxicated. At that time, he experienced substernal pain. On the following day, he experienced odynophagia during swallowing. His medical history was uneventful, and he showed no gastrointestinal symptoms and no drug history before the present symptoms. We performed an EGD 5 days after the initial event.
Physical examination showed unremarkable results. EGD showed a large 3.5×2.5 cm ulcer with a severely erythematous friable mucosa and marginal necrotic debris at 34 cm below the incisor (Fig. 5). Histologic findings showed necrosis with white cells and cellular debris. There was no evidence of viral infection or candidiasis and malignant cells. The patient was administered with 30 mg/day lansoprazole and 60 mg/day sucralfate for 1 month. A repeat endoscopy after 1 month showed marked improvement of the mucosa.
Go to : 
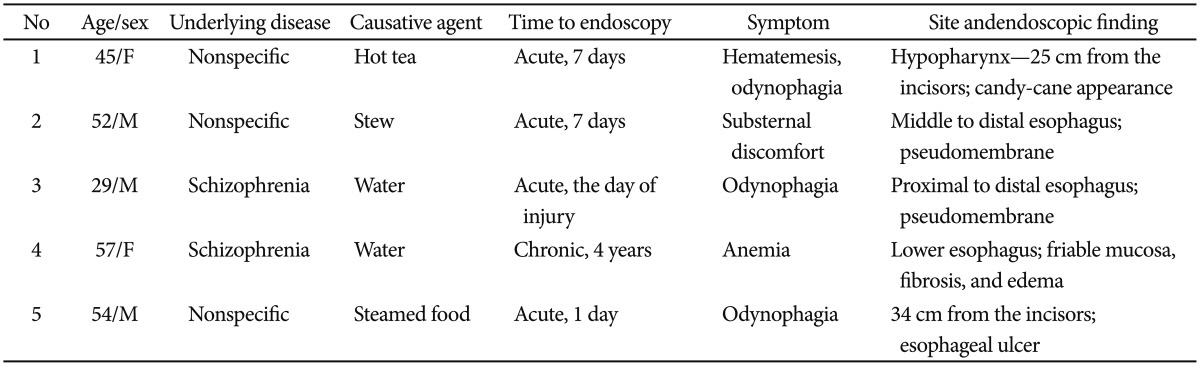
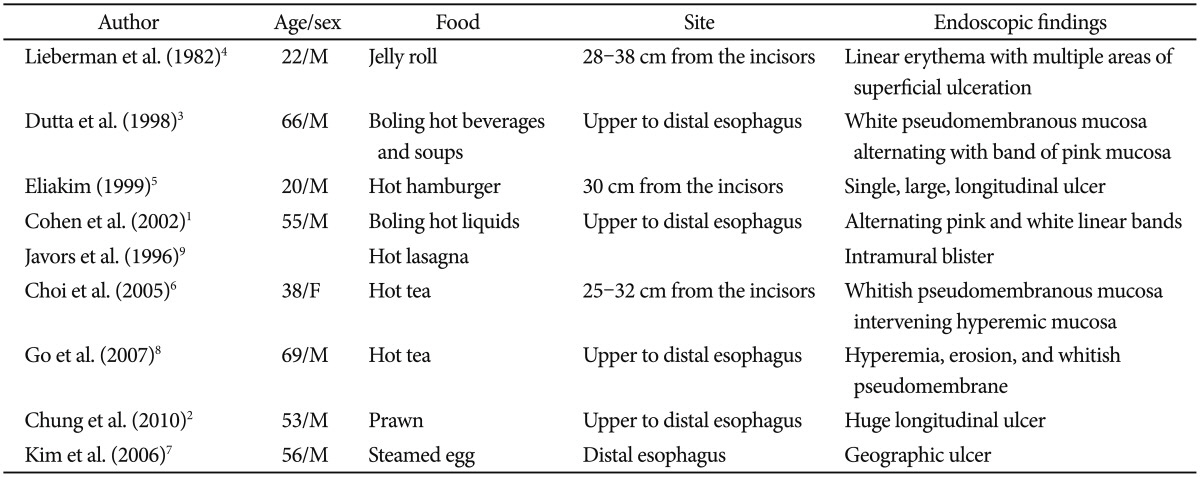
Acute esophageal thermal injury is a rare cause of esophageal disease. The exact prevalence of esophageal thermal injury is unknown, and the exact clinical course is unclear. Here, we present the clinical endoscopic findings of five patients who sustained this injury by consuming different hot foods, of different amounts and at different periods of exposure (Table 1). Previous studies have reported on the endoscopic and histological characteristics of esophageal injuries due to hot solid or liquid materials only (Table 2).1,2,3,4,5,6,7,8,9
Choi et al.6 reported the candy-cane appearance of the esophagus after the patient drank hot tea, and found a mucosa with a mixed whitish pseudomembrane and flare. Dutta et al.3 and Cohen and Kegel1 also reported cases in which the candy-cane appearance with mucous and a mixed whitish pseudomembrane and flare appeared after drinking boiling hot beverages. They assumed that the candy-cane appearance of the esophagus was due to the flow of hot liquid. What was interesting is that in Choi et al.6 case, the initial endoscopic finding was mainly a whitish pseudomembrane, while the follow-up endoscopic finding 4 days later was the candy-cane appearance. In our first case, the patient drank hot tea; here as well, the initial endoscopic finding was a whitish pseudomembranous mucosa in the mucosal geographic shape, while the follow-up endoscopic findings 7 days later showed the candy-cane appearance. In addition, the lesion showed a geographic pattern rather than a band pattern. It is thought that blisters are initially formed and, as they break, they change into pseudomembrane lesions. Furthermore, in our second case, the patient swallowed hot stew, and the initial endoscopic finding was a whitish pseudomembrane. We believe that thermal injury to the esophagus results in tissue damage, which leads to the whitish pseudomembrane observed in the first endoscopy. Over time, the endoscopic findings change with the development of inflammatory responses, resulting in alternating bands of whitish pseudomembranous lesions and linear erythema, resembling a candy cane. Thus, the endoscopic findings of thermal injury differ depending on the material causing the injury and the time at which the endoscopy is performed.
In our third case, the patient drank a large amount of hot water at once. We performed the endoscopy 2 days later, and the results showed a whitish pseudomembrane that had nearly completely encircled the esophageal mucosa; moreover, the partially exposed hyperemic mucosa easily bled on touching. Such severe endoscopic findings have not been reported previously. Seven days later, a follow-up endoscopy showed hyperemic and edematous mucosa and mild whitish fibrosis on the upper and middle esophagus. Since the patient did not return for follow-up after discharge, we could not obtain long-term follow-up data. However, from our observations, we believe that the amount of hot food consumed might make a difference to the endoscopic findings and to the prognosis of esophageal thermal injury.
We also found that the period of exposure to the hot food contributes to differences in endoscopic findings. In our fourth case, the patient had always been drinking hot water. Thus, she was exposed to hot water chronically, and the endoscopic finding was edematous, friable esophageal mucosa that easily bled on touching. There is no such reported case of a patient consuming hot liquid foods over a long term. We assumed that the repeated inflammatory response led to esophageal corrosion, which may progress to fibrosis. Unfortunately, since the patient did not return for follow-up after discharge, we could not obtain long-term follow-up data or determine the prognosis, especially with regard to esophageal stricture and anemia after treatment.
We assumed that the esophageal ulcer in case 5 was induced by the hot steamed egg. A review of previous such cases indicated that hot solid foods tend to induce esophageal ulcers.2,4,5
In conclusion, the endoscopic findings of esophageal thermal injury depend on the time to endoscopy after the incident, the causative material, the amount of food consumed, and the exposure period. Therefore, when patients present with unspecific esophagitis, ulcer, or a pseudomembranous band, their history should be examined in detail.
Go to : 
References
2. Chung WC, Paik CN, Jung JH, Kim JD, Lee KM, Yang JM. Acute thermal injury of the esophagus from solid food: clinical course and endoscopic findings. J Korean Med Sci. 2010; 25:489–491. PMID: 20191054.

3. Dutta SK, Chung KY, Bhagavan BS. Thermal injury of the esophagus. N Engl J Med. 1998; 339:480–481. PMID: 9705693.

4. Lieberman DA, Keeffe EB. Esophageal burn and the microwave oven. Ann Intern Med. 1982; 97:137. PMID: 7091986.

5. Eliakim R. Thermal injury from a hamburger: a rare cause of odynophagia. Gastrointest Endosc. 1999; 50:282–283. PMID: 10425431.

6. Choi EK, Lee GH, Jung HY, et al. The healing course of thermal esophageal injury: a case report. Gastrointest Endosc. 2005; 62:158–160. PMID: 15990841.

7. Kim SM, Jung SH, Kim YM, et al. Esophageal ulcer by thermal injury from steamed egg. Korean J Gastrointest Endosc. 2006; 32:190–193.
8. Go H, Yang HW, Jung SH, et al. Esophageal thermal injury by hot adlay tea. Korean J Intern Med. 2007; 22:59–62. PMID: 17427650.

9. Javors BR, Panzer DE, Goldman IS. Acute thermal injury of the esophagus. Dysphagia. 1996; 11:72–74. PMID: 8556881.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download