Abstract
Obscure gastrointestinal bleeding (OGIB) refers to gastrointestinal (GI) bleeding of unclear origin that persists or recurs after negative findings on esophagogastroduodenoscopy and colonoscopy. OGIB accounts for approximately 5% of all types of GI bleeding. More than 80% of OGIB cases originate in the small bowel. The ability to detect OGIB in the small bowel has significantly advanced and been revolutionized since the introduction of the capsule endoscopy and double-balloon enteroscopy techniques in 2000 and 2001, respectively. With these new methods for small-bowel evaluation, new guidelines have been proposed for the diagnosis and management of OGIB. However, some issues remain unsolved. The purpose of this article is to review the various modalities used for evaluating OGIB, including capsule endoscopy and double-balloon enteroscopy, and to help guide clinicians in their decisions on which modality will be the most effective.
Obscure gastrointestinal bleeding (OGIB) refers to gastrointestinal (GI) bleeding of unclear origin that persists or recurs after negative findings on upper GI endoscopy or colonoscopy. OGIB accounts for approximately 5% of all cases of GI bleeding.1 In >80% of cases, OGIB originates in the small bowel.2 It is classified as "overt" when there are manifestations of bleeding such as hematochezia or melena, and as "occult" when fecal occult blood tests are positive or iron deficiency anemia is presumed to be caused by GI blood loss.3
The recently developed techniques of capsule endoscopy (CE) and double-balloon enteroscopy (DBE) have widely replaced the previously used techniques of push enteroscopy (PE) and laparotomy-assisted enteroscopy for the evaluation of OGIB.
This review summarizes our knowledge about the various modalities for evaluating OGIB, including CE and DBE.
The most common cause of small-bowel bleeding in Western countries is angioectasia (20% to 55%), followed by small-bowel tumors (10% to 20%), Crohn disease (2% to 10%), celiac disease (2% to 5%), Meckel's diverticulum (2% to 5%), and nonsteroidal anti-inflammatory drug enteropathy (5%).1 However, regional variations in the underlying causes of small-bowel bleeding exist. For example, a recent nationwide analysis of patients with small-bowel bleeding in South Korea revealed that the most common cause was active ulcers (26%), followed by angiodysplasia (10%), multiple erosions (8%), and small-bowel tumors (2%).4 The causes of small-bowel bleeding vary according to the patient's age.5 In patients <40 years old, the most common cause of OGIB was reported to be angiodysplasia (54%), followed by Crohn disease (34%), small intestinal tumors (23%), small intestinal ulcers (13%), tumors (12%), nonspecific enteritis (11%), and angioectasia (9%). For patients aged 41 to 64 years, the most common causes of OGIB were angioectasia (35%) and small intestinal tumors (31%), followed by nonspecific enteritis (10%).
PE involves insertion of an endoscope through the oral cavity into the jejunum. PE is a readily available, safe, and effective technique for detecting and treating diseases of the proximal gut. Complications are rare if PE is performed without an overtube. PE with an overtube is generally performed only when a moderate increase in depth of insertion into the small bowel is required. When CE is not available, PE is a reasonable, low-risk option, but produces it produces only a moderate diagnostic yield.6 For example, in a study of 63 patients, after exclusion of all lesions proximal to the ligament of Treitz, the diagnostic yield for PE was 41% in patients with recurrent overt OGIB, 33% in those with persistent overt OGIB, and 26% in those with occult OGIB.7
The benefits of CE include visualization of the entire small bowel, safety, noninvasiveness, and high diagnostic yield. However, CE has some limitations such as the fact that no biopsies are taken to accompany the test, it is difficult to accurately locate the source of the bleeding, and there is a risk of capsule retention.3 CE also cannot be used for therapeutic intervention. Capsule retention has been reported in 1.5% to 5% of patients with suspected Crohn disease and OGIB. CE should be used with caution in patients with known or suspected GI obstruction, fistulas, or motility disorders.3,8
Compared with CE, DBE is more invasive, requires sedation, and can be laborious. It also takes time to learn how to perform DBE. Complications include the potential for pancreatitis and perforation of the small bowel and ileus.9,10,11 However, the major advantage of DBE is that it can be used for therapeutic interventions such as endoscopic hemostasis of bleeding, obtaining tissue biopsies for histological analysis, and marking the location of disease to direct subsequent surgery.12
There are few comparative studies or meta-analyses and no prospective, randomized, controlled trials comparing CE and DBE specifically in OGIB. Arakawa et al.13 reported that the overall diagnostic yield did not differ significantly between DBE (64%) and CE (54%). A meta-analysis also reported a similar diagnostic yield for CE (61.7%) and DBE (55.5%).14 A meta-analysis of 20 prospective studies comparing CE with other diagnostic modalities, such as balloon or spiral-assisted enteroscopy, showed that the diagnostic yield for CE was 56% compared with 26% for PE and 6% for small-bowel follow-through.15 In a recently reported meta- and pooled analysis of 12 eligible studies that included 712 patients with OGIB, the overall diagnostic yields of CE and DBE were similar. In subanalyses, the diagnostic yields of CE and DBE differed significantly for certain causes of OGIB such as blood clots (CE 21.8% vs. DBE 3.3%; p<0.00001) and diverticulum (CE 0.6% vs. DBE 3.97%; p=0.02). Of 205 cases of OGIB, 148 (72.2%) were detected with CE but not DBE and 57 (27.8%) were detected with DBE but not CE.16 Thus, both modalities are important for the detection of OGIB, and their combined use is better than either modality alone.
For patients with OGIB, the diagnostic yield of traditional radiological examination modalities such as small-bowel follow-through or enteroclysis is relatively low (6% to 10%).17 Computed tomography (CT) enterography is a noninvasive technique that visualizes the extravasation of contrast medium into the intestinal lumen to identify the source of OGIB.18 In a study of 26 patients with massive GI bleeding, multidetector CT accurately diagnosed 89%, with a positive predictive value of 95%. The location of the actively bleeding lesions in these patients corresponded exactly to sites revealed by angiograms.19 Of these patients, 56% had small-bowel tumors. CT enterography is more appropriate than multidetector CT when GI obstruction is suspected, as in cases of small-bowel tumors.20 Therefore, CT enterography should be the modality of choice when neoplastic disease is suspected but CE findings are negative.
Angiography is useful for the evaluation of overt OGIB. The diagnostic yield of angiography for lower GI bleeding has been reported to be 27% to 77%, but there are limited data on the diagnostic yield of angiography in OGIB.21 Vascular lesions, mainly small-bowel angiodysplasia, have the highest rates of rebleeding, despite endoscopic therapy, and are associated with comorbid conditions.22
The diagnostic yield of CE allowed the identification of bleeding lesions in 67% of patients with overt OGIB, which was higher than in previous studies.23 The diagnostic yield of CE is improved when it is performed early after the bleeding, varying from 44.2% to 92.3% in patients with OGIB.24 When DBE was performed during active bleeding, the diagnostic yield was 83% to 100%,25,26 which was significantly higher than the 48% to 58% noted when the examination was performed after bleeding ceased. "Emergency" DBE can be performed within 24 hours of onset of overt OGIB.27 With DBE, it is possible to diagnose and treat the lesion simultaneously. However, 45% of the patients were given a nonendoscopic treatment such as surgery, radiology, or conservative medical therapy.23 DBE is an invasive and time-consuming procedure that often requires general anesthesia. In addition, it is unlikely to be feasible in most centers.
Therefore, the Korean Gut Image Study Group and the American Society for Gastrointestinal Endoscopy (ASGE) have recommended CE or tagged red blood cell scintigraphy for patients with massive upper bleeding and negative esophagogastroduodenoscopy (EGD) findings (Figs. 1, 2).18 CE permits clinicians to choose the appropriate therapeutic option for patients. For patients with overt inactive OGIB, the ASGE guidelines recommend CE, deep enteroscopy, PE, and/or colonoscopy.18
Repeated endoscopy (including EGD) and colonoscopy are recommended for patients with occult OGIB. A retrospective review of prospectively collected data on the use of CE showed that 9 of 140 patients with OGIB had lesions that could have been evaluated by using conventional endoscopy or colonoscopy.28 Generally, CE detects bleeding lesions that could have been evaluated by using conventional endoscopy in 3% to 17% of cases and that could have been evaluated by using EGD and colonoscopy in 2% to 4% of cases. Repeated endoscopy should be considered when the initial examination was suboptimal or when there is reason to suspect that lesions have gone undetected.29
CE is recommended as the first diagnostic test if no contraindications exist (Figs. 1, 3). If a lesion is detected, appropriate endoscopic, angiographic, medical, or surgical intervention should be performed. If CE findings are negative, the patient's clinical status should be considered.18 Stable patients may be observed without further testing. In patients with negative CE findings who were reevaluated within a mean of 24 months, the rebleeding rate was 16.4%, which was significantly lower than that of patients with positive CE findings. However, for patients with negative CE findings who are taking anticoagulation medicine, close observation is required and alternative modalities should be considered.4,30 There are currently no clear indications about which alternative technique should be used or the appropriate timing for additional testing. A significant increase in the diagnostic yield of CE was reported on repeating the procedure in patients who exhibited decreased hemoglobin of at least 4 g/dL or in patients converting from occult to overt bleeding.31 Another option is to proceed with DBE instead of repeating CE. DBE may detect the source of bleeding in 30% of OGIB patients after CE yielding negative findings.14 Thus, patients with ongoing or recurrent overt bleeding, or patients with occult bleeding who experience significantly reduced hemoglobin levels, should proceed with either repeat CE or with DBE after an initial CE with negative findings.3
It remains preferable to begin clinical evaluation of small-bowel bleeding by using CE rather than DBE under most circumstances. However, the role of both procedures in diagnosing and managing OGIB has been generally accepted and can be summarized as CE-guided DBE or targeted DBE. CE and DBE demonstrate similar yields for the detection of OGIB. Various factors must be considered when deciding which technique to use, including the characteristics of each method, clinical factors such as the patient's status and long-term outcomes, availability of the technology, and availability of the expertise required to perform the tests and interpret the results. In addition, cost-effectiveness should be considered. The differences in cost when a public health system covers the expenses of medical care in different countries must be acknowledged.32 In conclusion, CE and DBE remain complementary methods that are essential for the detection and successful management of OGIB.
References
1. Liu K, Kaffes AJ. Review article: the diagnosis and investigation of obscure gastrointestinal bleeding. Aliment Pharmacol Ther. 2011; 34:416–423. PMID: 21692820.

2. Keum B, Chun HJ. Capsule endoscopy and double balloon enteroscopy for obscure gastrointestinal bleeding: which is better? J Gastroenterol Hepatol. 2011; 26:794–795. PMID: 21488944.

3. Teshima CW. Small bowel endoscopy for obscure GI bleeding. Best Pract Res Clin Gastroenterol. 2012; 26:247–261. PMID: 22704568.

4. Min YW, Kim JS, Jeon SW, et al. Long-term outcome of capsule endoscopy in obscure gastrointestinal bleeding: a nationwide analysis. Endoscopy. 2014; 46:59–65. PMID: 24254387.

5. Zhang BL, Chen CX, Li YM. Capsule endoscopy examination identifies different leading causes of obscure gastrointestinal bleeding in patients of different ages. Turk J Gastroenterol. 2012; 23:220–225. PMID: 22798110.

6. Akerman PA, Cantero D. Spiral enteroscopy and push enteroscopy. Gastrointest Endosc Clin N Am. 2009; 19:357–369. PMID: 19647645.
7. Lara LF, Bloomfeld RS, Pineau BC. The rate of lesions found within reach of esophagogastroduodenoscopy during push enteroscopy depends on the type of obscure gastrointestinal bleeding. Endoscopy. 2005; 37:745–750. PMID: 16032494.

8. Rey JF, Gay G, Kruse A, Lambert R. ESGE Guidelines Committee. European Society of Gastrointestinal Endoscopy guideline for video capsule endoscopy. Endoscopy. 2004; 36:656–658. PMID: 15243892.

9. Mehdizadeh S, Ross A, Gerson L, et al. What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006; 64:740–750. PMID: 17055868.

10. Gross SA, Stark ME. Initial experience with double-balloon enteroscopy at a U.S. center. Gastrointest Endosc. 2008; 67:890–897. PMID: 18178204.

11. Pasha SF, Hara AK, Leighton JA. Diagnostic evaluation and management of obscure gastrointestinal bleeding: a changing paradigm. Gastroenterol Hepatol (N Y). 2009; 5:839–850. PMID: 20567529.
12. May A, Nachbar L, Pohl J, Ell C. Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations. Am J Gastroenterol. 2007; 102:527–535. PMID: 17222315.

13. Arakawa D, Ohmiya N, Nakamura M, et al. Outcome after enteroscopy for patients with obscure GI bleeding: diagnostic comparison between double-balloon endoscopy and videocapsule endoscopy. Gastrointest Endosc. 2009; 69:866–874. PMID: 19136098.

14. Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol. 2011; 26:796–801. PMID: 21155884.

15. Triester SL, Leighton JA, Leontiadis GI, et al. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005; 100:2407–2418. PMID: 16279893.

16. Zhang Q, He Q, Liu J, Ma F, Zhi F, Bai Y. Combined use of capsule endoscopy and double-balloon enteroscopy in the diagnosis of obscure gastrointestinal bleeding: meta-analysis and pooled analysis. Hepatogastroenterology. 2013; 60:1885–1891. PMID: 24719922.
17. Malik A, Lukaszewski K, Caroline D, et al. A retrospective review of enteroclysis in patients with obscure gastrointestinal bleeding and chronic abdominal pain of undetermined etiology. Dig Dis Sci. 2005; 50:649–655. PMID: 15844696.

18. Fisher L, Lee Krinsky M, et al. ASGE Standards of Practice Committee. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010; 72:471–479. PMID: 20801285.

19. Yoon W, Jeong YY, Shin SS, et al. Acute massive gastrointestinal bleeding: detection and localization with arterial phase multi-detector row helical CT. Radiology. 2006; 239:160–167. PMID: 16484350.

20. Hakim FA, Alexander JA, Huprich JE, Grover M, Enders FT. CT-enterography may identify small bowel tumors not detected by capsule endoscopy: eight years experience at Mayo Clinic Rochester. Dig Dis Sci. 2011; 56:2914–2919. PMID: 21735085.

21. Zuckerman GR, Prakash C. Acute lower intestinal bleeding: part I: clinical presentation and diagnosis. Gastrointest Endosc. 1998; 48:606–617. PMID: 9852451.
22. Gerson LB. Is there a role for angiography in patients with obscure overt bleeding? Am J Gastroenterol. 2012; 107:1377–1379. PMID: 22951877.
23. Lecleire S, Iwanicki-Caron I, Di-Fiore A, et al. Yield and impact of emergency capsule enteroscopy in severe obscure-overt gastrointestinal bleeding. Endoscopy. 2012; 44:337–342. PMID: 22389234.

24. Pennazio M, Santucci R, Rondonotti E, et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology. 2004; 126:643–653. PMID: 14988816.

25. Shinozaki S, Yamamoto H, Yano T, et al. Long-term outcome of patients with obscure gastrointestinal bleeding investigated by double-balloon endoscopy. Clin Gastroenterol Hepatol. 2010; 8:151–158. PMID: 19879968.

26. Tanaka S, Mitsui K, Yamada Y, et al. Diagnostic yield of double-balloon endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2008; 68:683–691. PMID: 18561920.

27. Monkemuller K, Neumann H, Meyer F, Kuhn R, Malfertheiner P, Fry LC. A retrospective analysis of emergency double-balloon enteroscopy for small-bowel bleeding. Endoscopy. 2009; 41:715–717. PMID: 19670141.

28. Kitiyakara T, Selby W. Non-small-bowel lesions detected by capsule endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005; 62:234–238. PMID: 16046986.

29. Shim KN, Moon JS, Chang DK, et al. Guideline for capsule endoscopy: obscure gastrointestinal bleeding. Clin Endosc. 2013; 46:45–53. PMID: 23423225.

30. Koh SJ, Im JP, Kim JW, et al. Long-term outcome in patients with obscure gastrointestinal bleeding after negative capsule endoscopy. World J Gastroenterol. 2013; 19:1632–1638. PMID: 23539070.

31. Viazis N, Papaxoinis K, Vlachogiannakos J, Efthymiou A, Theodoropoulos I, Karamanolis DG. Is there a role for second-look capsule endoscopy in patients with obscure GI bleeding after a nondiagnostic first test? Gastrointest Endosc. 2009; 69:850–856. PMID: 18950762.

32. Marmo R, Rotondano G, Rondonotti E, et al. Capsule enteroscopy vs. other diagnostic procedures in diagnosing obscure gastrointestinal bleeding: a cost-effectiveness study. Eur J Gastroenterol Hepatol. 2007; 19:535–542. PMID: 17556898.

Fig. 1
Korea Gut Image Study Group guidelines for obscure gastrointestinal bleeding. Adapted from Shim et al. Clin Endosc 2013;46:45-53.29 Dashed arrows indicate less-preferred options. GI, gastrointestinal; EGD, esophagogastroduodenoscopy; CE, capsule endoscopy; CTE, computed tomography enterography; DE, deep enteroscopy; PE, push enteroscopy; SB, small bowel; IOE, intraoperative enteroscopy.
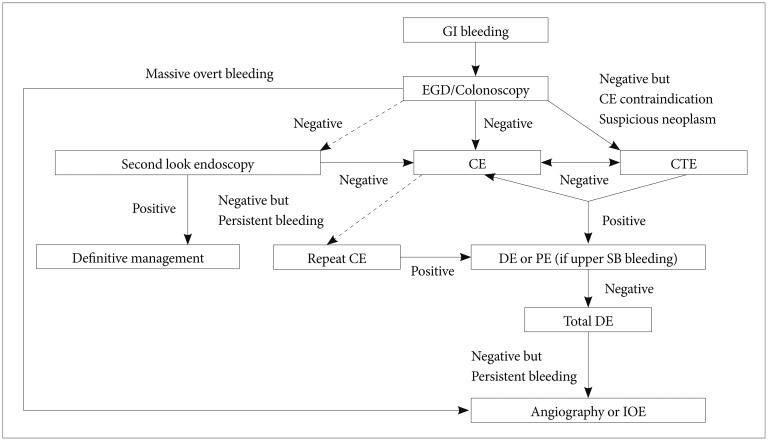
Fig. 2
American Society for Gastrointestinal Endoscopy guidelines in the management of overt gastrointestinal bleeding. Dashed arrows indicate less-preferred options. Positive test results should direct specific therapy. Because diagnostic tests can be complementary, more than one test may be needed, and the first-line test may be based on institutional expertise and availability. Adapted from ASGE Standards of Practice Committee et al. Gastrointest Endosc 2010;72:471-479, with permission from Elsevier.18 GI, gastrointestinal; EGD, esophagogastroduodenoscopy; PE, push enteroscopy; CT, computed tomography; OGIB, obscure gastrointestinal bleeding.
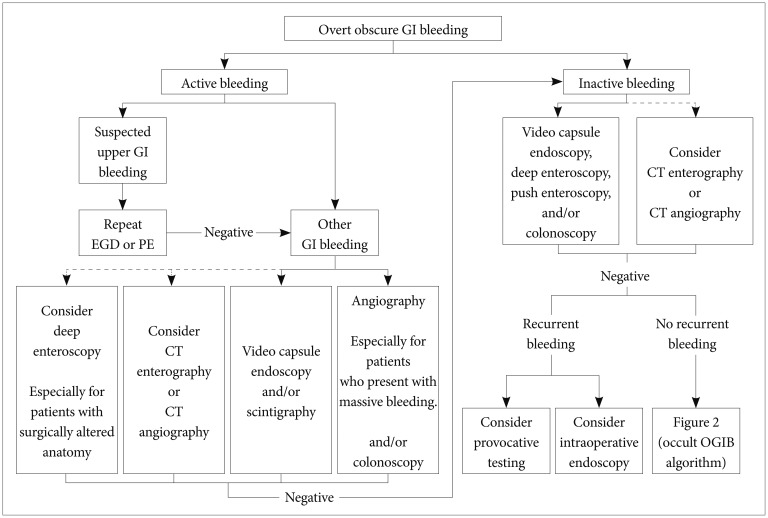
Fig. 3
American Society for Gastrointestinal Endoscopy guidelines for the management of occult gastrointestinal bleeding. Dashed arrows indicate less-preferred options. Positive test results should direct specific therapy. Because diagnostic tests can be complementary, more than one test may be needed, and the first-line test may be based on institutional expertise and availability. Adapted from ASGE Standards of Practice Committee et al. Gastrointest Endosc 2010;72:471-479, with permission from Elsevier.18 GI, gastrointestinal; EGD, esophagogastroduodenoscopy; CT, computed tomography; Hb, hemoglobin.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download