1. Winawer SJ, Zauber AG, Ho MN, et al. The National Polyp Study Workgroup. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med. 1993; 329:1977–1981. PMID:
8247072.

2. Han DS, Park JY, Yun HR, Bae SC. Cost-effectiveness analysis of colon cancer screening by colonosopic examination in Korea. Korean J Gastrointest Endosc. 2004; 28:1–8.
3. Kim HS. Postpolypectomy colonoscopy surveillance. Korean J Gastrointest Endosc. 2009; 39:257–264.
4. Gastrointestinal Pathology Study Group of Korean Society of Pathologists. Kang YK, Jin SY, et al. Early colorectal epithelial neoplasm in Korea: a multicenter survey of pathologic diagnosis. Korean J Pathol. 2013; 47:245–251. PMID:
23837017.

5. Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012; 143:844–857. PMID:
22763141.

6. Yang DH, Hong SN, Kim YH, et al. Korean guidelines for post-polypectomy colonoscopic surveillance. Intest Res. 2012; 10:89–109.

7. Snover DC, Ahnen DJ, Burt RW, Odze RD. Serrated polyps of the colon and rectum and serrated polyposis. In : Bosman FT, editor. World Health Organization; International Agency for Research on Cancer. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research on Cancer;2010. p. 160.
8. Rex DK, Kahi C, O'Brien M, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011; 73:419–422. PMID:
21353837.

9. Kaminski MF, Hassan C, Bisschops R, et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014; 46:435–449. PMID:
24639382.

10. Rastogi A. Optical diagnosis of small colorectal polyp histology with high-definition colonoscopy using narrow band imaging. Clin Endosc. 2013; 46:120–129. PMID:
23614121.

11. Shepherd NA, Warren BF, Williams GT, Greenson JK, Lauwers GY, Novelli MR. Polyps and tumour-like lesions of the large intestine. In : Morson BC, Shepherd NA, editors. Morson and Dawson's Gastrointestinal Pathology. 5th ed. Chichester: Wiley-Blackwell;2013. p. 647–684.
12. Talbot JC, Price A, Salto-Tellez M. Biopsy Pathology in Colorectal Disease. 2nd ed. London: Hodder Arnold;2007. p. 251–291.
13. Messick CA, Church J, Casey G, Kalady MF. Identification of the methylator (serrated) colorectal cancer phenotype through precursor serrated polyps. Dis Colon Rectum. 2009; 52:1535–1541. PMID:
19690479.

14. Kang GH. Four molecular subtypes of colorectal cancer and their precursor lesions. Arch Pathol Lab Med. 2011; 135:698–703. PMID:
21631262.

15. Aust DE, Baretton GB. Members of the Working Group GI-Pathology of the German Society of Pathology. Serrated polyps of the colon and rectum (hyperplastic polyps, sessile serrated adenomas, traditional serrated adenomas, and mixed polyps)-proposal for diagnostic criteria. Virchows Arch. 2010; 457:291–297. PMID:
20617338.

16. Lee SK, Chang HJ, Kim TI, et al. Clinicopathologic findings of colorectal traditional and sessile serrated adenomas in Korea: a multicenter study. Digestion. 2008; 77:178–183. PMID:
18617741.

17. Gurudu SR, Heigh RI, De Petris G, et al. Sessile serrated adenomas: demographic, endoscopic and pathological characteristics. World J Gastroenterol. 2010; 16:3402–3405. PMID:
20632442.

18. Mohammadi M, Bzorek M, Bonde JH, Nielsen HJ, Holck S. The stem cell marker CD133 is highly expressed in sessile serrated adenoma and its borderline variant compared with hyperplastic polyp. J Clin Pathol. 2013; 66:403–408. PMID:
23436931.

19. Hassan C, Pickhardt PJ, Kim DH, et al. Systematic review: distribution of advanced neoplasia according to polyp size at screening colonoscopy. Aliment Pharmacol Ther. 2010; 31:210–217. PMID:
19814745.

20. Chaptini L, Chaaya A, Depalma F, Hunter K, Peikin S, Laine L. Variation in polyp size estimation among endoscopists and impact on surveillance intervals. Gastrointest Endosc. 2014; 80:652–659. PMID:
24679658.

21. Turner JK, Wright M, Morgan M, Williams GT, Dolwani S. A prospective study of the accuracy and concordance between in-situ and postfixation measurements of colorectal polyp size and their potential impact upon surveillance. Eur J Gastroenterol Hepatol. 2013; 25:562–567. PMID:
23325278.

22. Odze RD, Riddel RH, Bosman FT, et al. Premalignant lesions of the digestive system. In : Bosman FT, editor. World Health Organization. International Agency for Research on Cancer. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research on Cancer;2010. p. 10–12.
23. van Putten PG, Hol L, van Dekken H, et al. Inter-observer variation in the histological diagnosis of polyps in colorectal cancer screening. Histopathology. 2011; 58:974–981. PMID:
21585430.

24. Kim HG, Kim JO, Lee SH, et al. Clinical classification of colorectal epithelial tumors and proposal for diagnostic coding. Intest Res. 2011; 9:1–11.

25. Jung ES, Kang YK, Cho MY, et al. Update on the proposal for creating a guideline for cancer registration of the gastrointestinal tumors (I-2). Korean J Pathol. 2012; 46:443–453. PMID:
23136571.

26. Rosai J. Why microscopy will remain a cornerstone of surgical pathology. Lab Invest. 2007; 87:403–408. PMID:
17401434.

27. Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost-effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol. 2010; 8:865–869. PMID:
20621680.

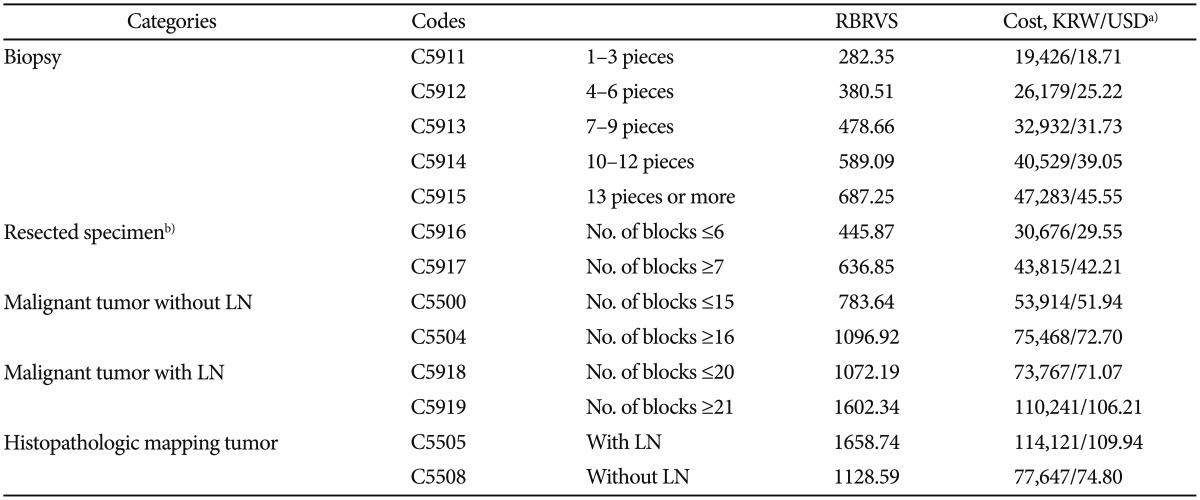
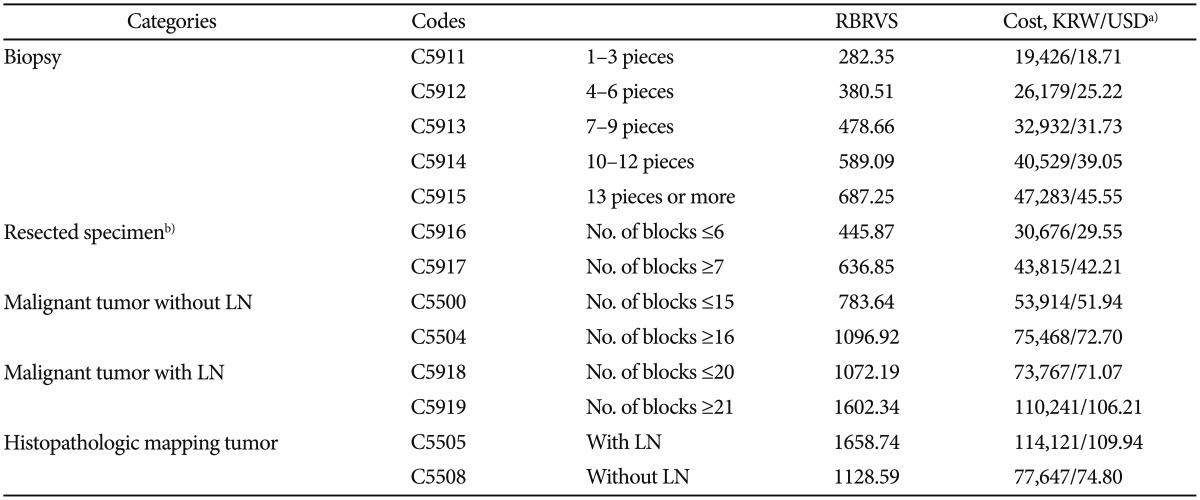
28. Hwang I, Kang YN, Kwon KY, et al. Comparative study of relative value for diagnostic procedure of surgical pathology in Korea and United States. Korean J Pathol. 2011; 45:9–14.

29. American Medical Association. Principles of CPT Coding. 5th ed. Chicago: American Medical Association;2007. p. 392–403.
30. Kessler WR, Imperiale TF, Klein RW, Wielage RC, Rex DK. A quantitative assessment of the risks and cost savings of forgoing histologic examination of diminutive polyps. Endoscopy. 2011; 43:683–691. PMID:
21623556.