1. Kimmey MB. The ERCP room. In : Baron TH, Kozarek R, Carr-Locke DL, editors. ERCP. Philadelphia: Saunders/Elsevier;2008. p. 13–18.
2. Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009; 70:80–88. PMID:
19286178.

3. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918. PMID:
8782497.

4. Sullivan DM, Hood TR, Griffen WO Jr. Biliary tract surgery in the elderly. Am J Surg. 1982; 143:218–220. PMID:
6800276.

5. Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997; 41:433–435. PMID:
9391238.

6. Hacker KA, Schultz CC, Helling TS. Choledochotomy for calculous disease in the elderly. Am J Surg. 1990; 160:610–612. PMID:
2252122.

7. Ashton CE, McNabb WR, Wilkinson ML, Lewis RR. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Ageing. 1998; 27:683–688. PMID:
10408661.

8. Clarke GA, Jacobson BC, Hammett RJ, Carr-Locke DL. The indications, utilization and safety of gastrointestinal endoscopy in an extremely elderly patient cohort. Endoscopy. 2001; 33:580–584. PMID:
11473328.

9. Kim JE, Cha BH, Lee SH, et al. Safety and efficacy of endoscopic retrograde cholangiopancreatograpy in very elderly patients. Korean J Gastroenterol. 2011; 57:237–242. PMID:
21519177.

10. Lukens FJ, Howell DA, Upender S, Sheth SG, Jafri SM. ERCP in the very elderly: outcomes among patients older than eighty. Dig Dis Sci. 2010; 55:847–851. PMID:
19337836.

11. Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc. 2000; 52:187–191. PMID:
10922089.

12. Lillemoe KD. Pancreatic disease in the elderly patient. Surg Clin North Am. 1994; 74:317–344. PMID:
8165471.

13. Fisher L, Fisher A, Thomson A. Cardiopulmonary complications of ERCP in older patients. Gastrointest Endosc. 2006; 63:948–955. PMID:
16733108.

14. Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004; 60:721–731. PMID:
15557948.

15. Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007; 66:27–34. PMID:
17591470.

16. Davenport DL, Bowe EA, Henderson WG, Khuri SF, Mentzer RM Jr. National Surgical Quality Improvement Program (NSQIP) risk factors can be used to validate American Society of Anesthesiologists Physical Status Classification (ASA PS) levels. Ann Surg. 2006; 243:636–641. PMID:
16632998.

17. Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. Lichtenstein DR, Jagannath S, et al. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008; 68:815–826. PMID:
18984096.

18. Trapani G, Altomare C, Liso G, Sanna E, Biggio G. Propofol in anesthesia. Mechanism of action, structure-activity relationships, and drug delivery. Curr Med Chem. 2000; 7:249–271. PMID:
10637364.

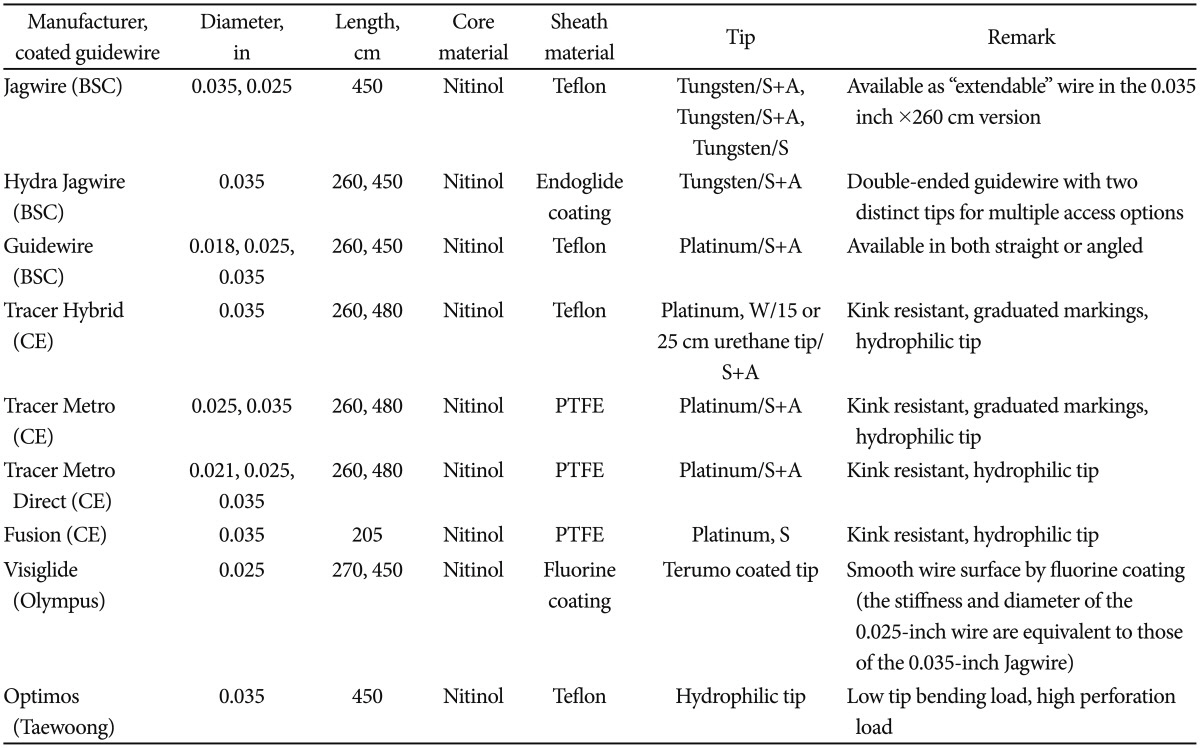
19. Somogyi L, Chuttani R, Croffie J, et al. Guidewires for use in GI endoscopy. Gastrointest Endosc. 2007; 65:571–576. PMID:
17383455.

20. Lee TH, Park do H, Park JY, et al. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest Endosc. 2009; 69(3 Pt 1):444–449. PMID:
19007927.

21. Lella F, Bagnolo F, Colombo E, Bonassi U. A simple way of avoiding post-ERCP pancreatitis. Gastrointest Endosc. 2004; 59:830–834. PMID:
15173796.

22. Mariani A, Giussani A, Di Leo M, Testoni S, Testoni PA. Guidewire biliary cannulation does not reduce post-ERCP pancreatitis compared with the contrast injection technique in low-risk and high-risk patients. Gastrointest Endosc. 2012; 75:339–346. PMID:
22075192.

23. Kawakami H, Maguchi H, Mukai T, et al. A multicenter, prospective, randomized study of selective bile duct cannulation performed by multiple endoscopists: the BIDMEN study. Gastrointest Endosc. 2012; 75:362–372. PMID:
22248605.

24. Katsinelos P, Paroutoglou G, Kountouras J, et al. A comparative study of standard ERCP catheter and hydrophilic guide wire in the selective cannulation of the common bile duct. Endoscopy. 2008; 40:302–307. PMID:
18283621.

25. Artifon EL, Sakai P, Cunha JE, Halwan B, Ishioka S, Kumar A. Guidewire cannulation reduces risk of post-ERCP pancreatitis and facilitates bile duct cannulation. Am J Gastroenterol. 2007; 102:2147–2153. PMID:
17581267.

26. Bailey AA, Bourke MJ, Williams SJ, et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008; 40:296–301. PMID:
18389448.

27. Lee TH, Park DH. Endoscopic prevention of post-ERCP pancreatitis. World J Gastroenterol. Forthcoming 2014.
28. Cennamo V, Fuccio L, Zagari RM, et al. Can a wire-guided cannulation technique increase bile duct cannulation rate and prevent post-ERCP pancreatitis? A meta-analysis of randomized controlled trials. Am J Gastroenterol. 2009; 104:2343–2350. PMID:
19532133.

29. Cheung J, Tsoi KK, Quan WL, Lau JY, Sung JJ. Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Gastrointest Endosc. 2009; 70:1211–1219. PMID:
19962504.

30. Tse F, Yuan Y, Moayyedi P, Leontiadis GI. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2012; 12:CD009662. PMID:
23235679.

31. Lee TH, Park SH, Son BS, et al. Four cases of guidewire induced periampullary perforation during endoscopic retrograde cholangiopancreatography. Korean J Gastrointest Endosc. 2011; 42:334–340.
32. Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002; 34:293–298. PMID:
11932784.

33. Martin DF, Tweedle DE. Retroperitoneal perforation during ERCP and endoscopic sphincterotomy: causes, clinical features and management. Endoscopy. 1990; 22:174–175. PMID:
2209500.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download