Abstract
Most infants with repaired gastroschisis develop normally and remain in good health. About 10% of patients with gastroschisis have other malformations. We report a case of choledocholithiasis and intestinal malrotation in an adolescent with repaired gastroschisis. A 17-year-old girl presented with fever, jaundice, and abdominal pain. She had undergone an operation to repair gastroschisis at birth. Physical examination revealed icteric sclera, a tight abdominal wall, and a longitudinal surgical scar at the midline. An abdominal computed tomography scan revealed a round calcifying lesion near the pancreas and a midline-positioned liver and gallbladder. Absence of the retroperitoneal duodenum and the anterior and left-sided position of the superior mesenteric vein compared with the superior mesenteric artery were observed. Results of abarium examination revealed intestinal malrotation. Endoscopic retrograde cholangiopancreatography revealed diffuse dilatation of the biliary trees and a malpositioned gallbladder. A single stone was removed by using a basket. The clinical symptoms improved after the patient underwent endoscopic retrograde cholangiopancreatography.
Gastroschisis is an uncommon congenital defect in the abdominal wall. About 10% of infants with gastroschisis have other malformations.1 The most common anomalies associated with gastroschisis are bowel atresia, undescended testicles, and intestinal volvulus.1 The prognosis has improved for patients with repaired gastroschisis.2 Repaired gastroschisis can make the abdominal wall too tight, which induces the contraction of the abdominal cavity and malpositioning of internal organs. In the medical literature, there have been no reports of disoriented biliary architecture associated with intestinal malrotation in patients who had undergone gastroschisis repair. We report a case of choledocholithiasis in an adolescent who had undergone gastroschisis repair, developed distorted biliary architecture combined with intestinal malrotation, and underwent endoscopic retrograde cholangiopancreatography (ERCP) with bile duct stone extraction. We present this rare case along with a literature review.
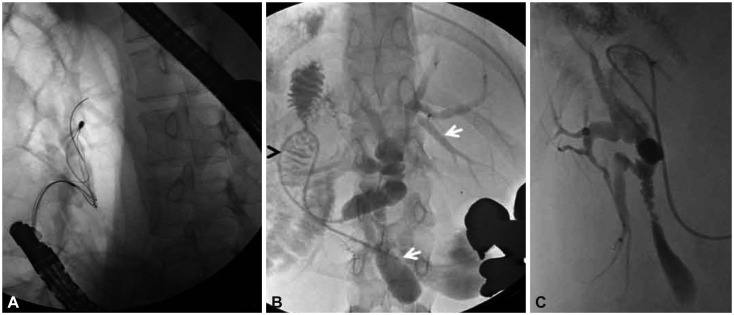
A 17-year-old girl visited Chungbuk National University Hospital, presenting with fever and abdominal pain that had developed 7 days previously. She had undergone an operation for gastroschisis repair at birth. At the time of admission, her vital signs were as follows: blood pressure, 120/80 mm Hg; pulse rate, 70 beats per minute; respiration rate, 18 breaths per minute; and body temperature, 37.5℃. She appeared emaciated and acutely ill. Her body mass index was 18.1 (height, 151 cm; and weight, 41.3 kg). A physical examination revealed icteric sclera, a very thin abdominal cavity, and a longitudinal surgical scar at the midline. Tenderness was noted in the upper abdominal area, and normal bowel sounds were heard. There was no particular finding in the limb or neurological examinations. Laboratory analysis revealed a white blood cell count of 27,000 cells/mm3; hemoglobin level, 12.3 g/dL; platelet count, 277,000 cells/mm3; aspartate aminotransferase level, 108 IU/L; alanine aminotransferase level, 144 IU/L; alkaline phosphatase level, 476 IU/L; total protein level, 6.5 g/dL; albumin level, 3.7 g/dL; total bilirubin level, 14.1 mg/dL; direct bilirubin level, 9.2 mg/dL; amylase level, 592 U/L; lipase level, 825 U/L; blood urea nitrogen level, 5.0 mg/dL; and creatinine level, 0.5 mg/dL. These data were compatible with diagnoses of acute cholangitis and acute biliary pancreatitis. An abdominal computed tomography scan revealed a round calcifying lesion near the pancreas (Fig. 1A), and the absence of the retroperitoneal duodenum and the anterior position of the spleen with respect to the left kidney. The anterior and left-sided position of the superior mesenteric vein compared with that of the superior mesenteric artery was observed in the abdominal computed tomography scan (Fig. 1B). The coronal view revealed the distorted architecture of the liver and a high-attenuation lesion at the extrahepatic bile duct (Fig. 1C). Results of a barium examination revealed a right-sided duodenojejunal flexure and malpositioning of the bowel, with the small bowel on the right side and the colon on the left side (Fig. 2). Intestinal malrotation could be diagnosed based on these findings. ERCP was performed by using a lateral-view endoscope in the usual way. After approaching the ampulla, the endoscope was pushed against the duodenal wall to maintain the papilla in the correct position, and a selective bile duct cannulation confirmed the presence of a 12-mm round stone in the common bile duct. With a guidewire-assisted technique, the single dark brown stone was removed by using a Dormia basket after the endoscopic sphincterotomy (Fig. 3A). The procedure lasted for 15 minutes. A cholangiogram obtained through an endoscopic nasobiliary drainage tube revealed a distorted biliary system, which was characterized with diffuse dilatation of the intrahepatic and extrahepatic biliary trees, downward-positioned gallbladder and a right intrahepatic biliary tree, and a horizontally located common bile duct. The abnormal orientation of the duodenum suggested intestinal malrotation (Fig. 3B, C). Clinical symptoms and liver function tests normalized after the ERCP procedure. The patient has been monitored for 3 years and is in a normal state.
This is the first report of choledocholithiasis associated with an abnormal biliary architecture and intestinal malrotation in an adolescent with repaired gastroschisis. Distortions of the biliary system, which were because of a malpositioned liver, fibrous bands, and malrotation of the midgut, had induced long-standing cholestasis and the development of a bile duct stone.
Recently, patients with abdominal wall defects have shown improved clinical outcomes.3 Current treatments for abdominal wall defects in newborns, including prosthesis implantation along the abdominal wall and total parenteral nutrition, have resulted in outcomes that are more favorable. Late gastroschisis-related mortality is rare and is often due to unrelated pathologies. In uncomplicated gastroschisis, late morbidity is uncommon and any additional surgery usually results from adhesive intestinal obstruction, a ventral hernia, or undescended testes.4 In one study about the outcomes of gastroschisis, four patients died among 66 patients, all who underwent a primary closure.2 Two of the four deaths were attributed to an excessively tight closure and pulmonary failure.2
This case showed that an excessively tight abdominal wall and intestinal malrotation cause malpositioning of many different internal organs. The distorted biliary system made it difficult to identify the location of the stone. In this case, the radiologist did not recognize the calcified round lesion as choledocholithiasis, and instead diagnosed it as parenchymal calcification. The identification of the distorted biliary tree in this patient who had undergone repaired gastroschisis allowed for early diagnosis and treatment.
Cholestasis rarely develops in gastroschisis patients in association with other anomalies or complications related to gastroschisis. Most cases of cholestasis develop in infants because of prolonged parenteral nutrition. Anomalies of the biliary tree associated with gastroschisis are extremely rare. Two cases of choledochal cyst5 and one case of biliary atresia6 have been reported. In addition, four cases of biliary obstruction with mechanical distortion of the biliary tree in infants who had undergone repaired gastroschisis have been reported.7,8
This case showed several indications of intestinal malrotation. Findings included the absence of the retroperitoneal duodenum,9 an abnormal relationship between the superior mesenteric vein and superior mesenteric artery,10,11 a right-sided duodenojejunal flexure, and malpositioning of the bowel.11 Intestinal malrotation can induce or potentiate biliary stasis by causing contraction or compression of the biliary tract and displacement of the duodenum.5,12 In this case, an abnormal configuration of the duodenum was associated with traction of the common bile duct, which caused its horizontal positioning and induced disturbance in the biliary drainage. Choledocholithiasis can develop in the presence of long-standing cholestasis. Although data about morbidities in patients with repaired gastroschisis are limited, disorders related to the biliary system can develop in these patients that can be potentiated by combined intestinal anomalies. Treatment with ERCP was successful in this patient, and she has been healthy thereafter. ERCP was performed in the usual way with a pushing maneuver. All procedures were performed by using a guidewire-assisted technique to reduce the procedure time with minimal air inflation. ERCP can be performed safely and conveniently in these patients, with excellent outcomes.
Acknowledgments
This work was supported by a research grant from the Chungbuk National University in 2011.
References
1. Hunter AG, Stevenson RE. Gastroschisis: clinical presentation and associations. Am J Med Genet C Semin Med Genet. 2008; 148C:219–230. PMID: 18655099.

2. Tunell WP, Puffinbarger NK, Tuggle DW, Taylor DV, Mantor PC. Abdominal wall defects in infants. Survival and implications for adult life. Ann Surg. 1995; 221:525–528. PMID: 7748034.

3. Islam S. Clinical care outcomes in abdominal wall defects. Curr Opin Pediatr. 2008; 20:305–310. PMID: 18475100.

4. Davies BW, Stringer MD. The survivors of gastroschisis. Arch Dis Child. 1997; 77:158–160. PMID: 9301359.

5. Serber J, Stranzinger E, Geiger JD, Teitelbaum DH. Association of gastroschisis and choledochal cyst. J Pediatr Surg. 2009; 44:e23–e26. PMID: 19302840.

6. Lee TC, Barshes NR, Nguyen L, et al. Gastroschisis and biliary atresia in a neonate: uncommon presentation or common precipitant. Eur J Pediatr Surg. 2005; 15:434–436. PMID: 16418964.

7. Teoh L, Wong CK, Martin H, O'Loughlin EV. Anterior abdominal wall defects and biliary obstruction. J Paediatr Child Health. 2005; 41:143–146. PMID: 15790327.

8. Hancock BJ, Wiseman NE, Rusnak BW. Bile duct stricture in an infant with gastroschisis treated by percutaneous transhepatic drainage, biliary stenting, and balloon dilation. J Pediatr Surg. 1989; 24:1071–1073. PMID: 2530328.

9. Daneman A. Malrotation: the balance of evidence. Pediatr Radiol. 2009; 39(Suppl 2):S164–S166. PMID: 19308379.

10. Loyer E, Eggli KD. Sonographic evaluation of superior mesenteric vascular relationship in malrotation. Pediatr Radiol. 1989; 19:173–175. PMID: 2654854.

11. Applegate KE. Evidence-based diagnosis of malrotation and volvulus. Pediatr Radiol. 2009; 39(Suppl 2):S161–S163. PMID: 19308378.

12. Kirby CP, Freeman JK, Ford WD, Davidson GP, Furness ME. Malrotation with recurrent volvulus presenting with cholestasis, pruritus, and pancreatitis. Pediatr Surg Int. 2000; 16:130–131. PMID: 10663862.

Fig. 1
Abdominal computed tomography findings. (A) A pre-enhanced computed tomography scan revealed a round calcifying lesion near the pancreas (arrow). (B) The absence of the retroperitoneal duodenum and the anterior and left-sided position of the superior mesenteric vein (arrowhead) compared with that of the superior mesenteric artery (arrow) were identified. (C) Coronal view showing the distorted architecture of the liver (arrows) and a high-attenuation lesion at the extrahepatic bile duct (arrowhead).
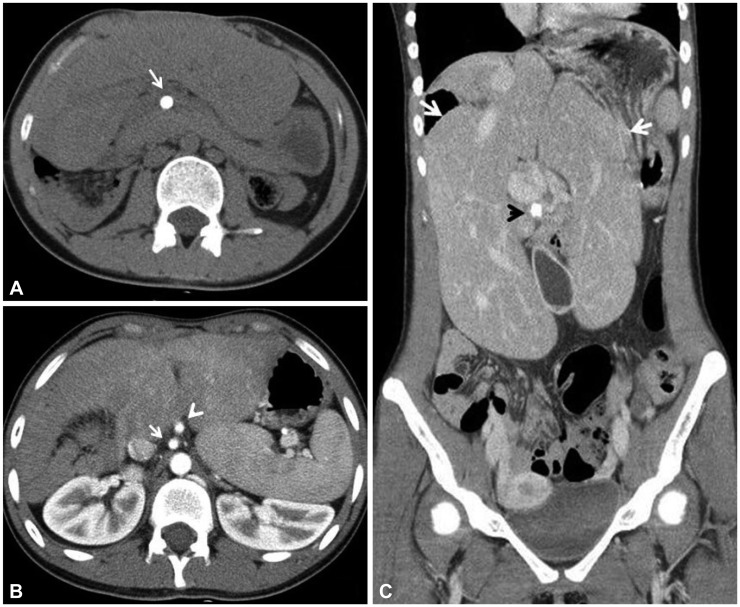
Fig. 2
A barium meal examination revealed a right-sided duodenojejunal flexure and malpositioning of the bowel, with the small bowel on the right side (arrows) and the colon on the left side (arrowheads).
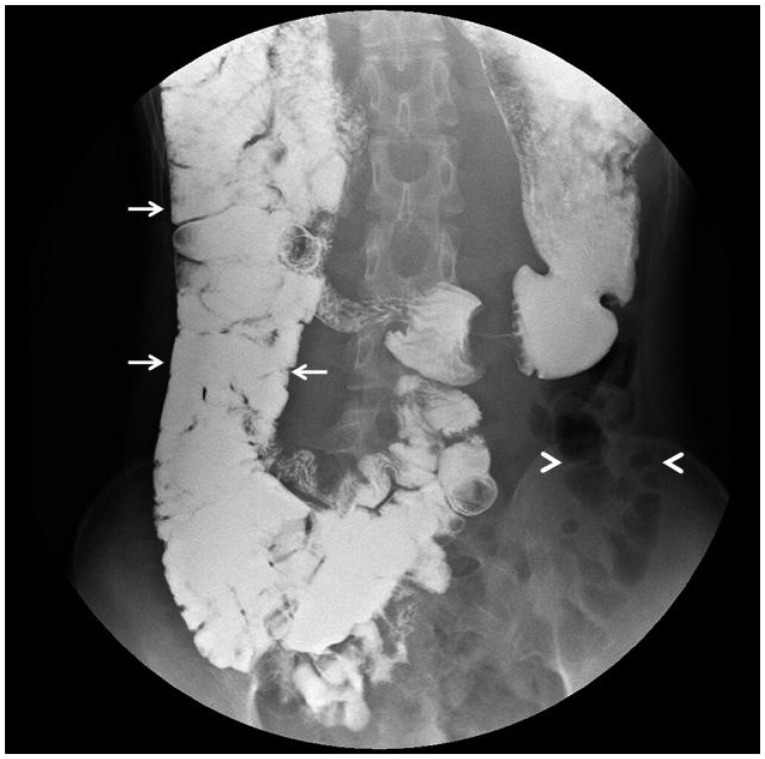
Fig. 3
Cholangiography. (A) With a guidewire-assisted technique, the single stone was removed by using a Dormia basket. (B) Diffuse dilatation of the intrahepatic and extrahepatic biliary trees and a downward-positioned gallbladder (arrows). The abnormal orientation of the duodenum (arrowhead) suggested intestinal malrotation. (C) Distorted architecture of the biliary tree.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download