Abstract
Laparoscopic fundoplication is a treatment option for gastroesophageal reflux disease refractory to medical treatment. When deciding whether or not to undergo surgery, patients with refractory gastroesophageal reflux disease and esophageal motility disorder need to fully understand the operative procedure, postoperative complications, and residual symptoms such as dysphagia, globus sensation, and recurrence of reflux. Herein, we report a case of a patient diagnosed with gastroesophageal reflux disease and aperistalsis who underwent Nissen (total, 360°) fundoplication after lack of response to medical treatment and subsequently underwent pneumatic dilatation due to unrelieved postoperative dysphagia and globus sensation.
Laparoscopic fundoplication is the gold standard of antireflux surgery. Approximately 50% to 60% of patients with gastroesophageal reflux disease (GERD) show impairment of esophageal motility.1 When GERD occurs in conjunction with esophageal dysmotility, it is unclear whether esophageal dysmotility is a primary defect that contributes to the etiology of GERD by delaying esophageal clearance of acid or if it is a consequence of direct esophageal injury associated with GERD.1 In patients with primary esophageal dysfunction, Nissen fundoplication may increase symptoms of dysphagia by creating a partial obstruction that esophageal peristalsis cannot overcome. However, in patients with secondary esophageal dysmotiliy, normal motility is expected to return after the refluxate is removed.1 However, aperistalsis is accompanied by refractory GERD, and in these cases, the best operative approach remains controversial.1-3 We report a case of a patient diagnosed with refractory GERD with aperistalsis who underwent pneumatic dilatation after Nissen fundoplication because of postoperative dysphagia.
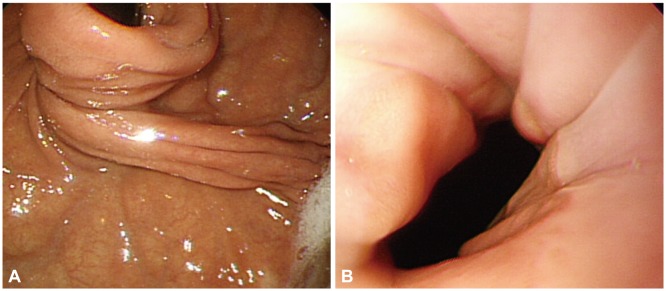
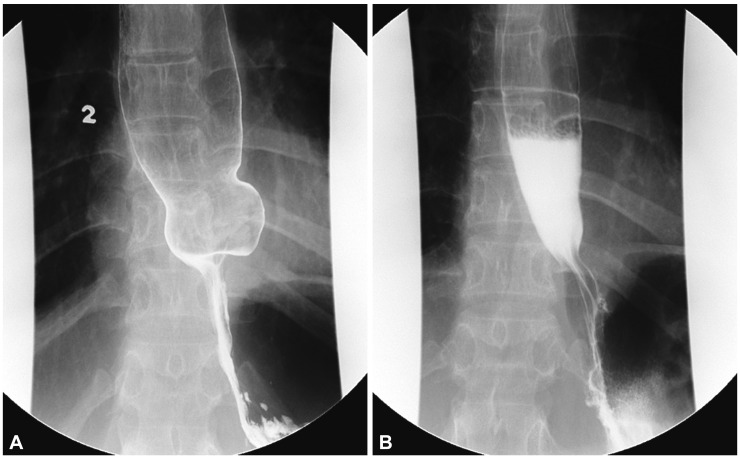
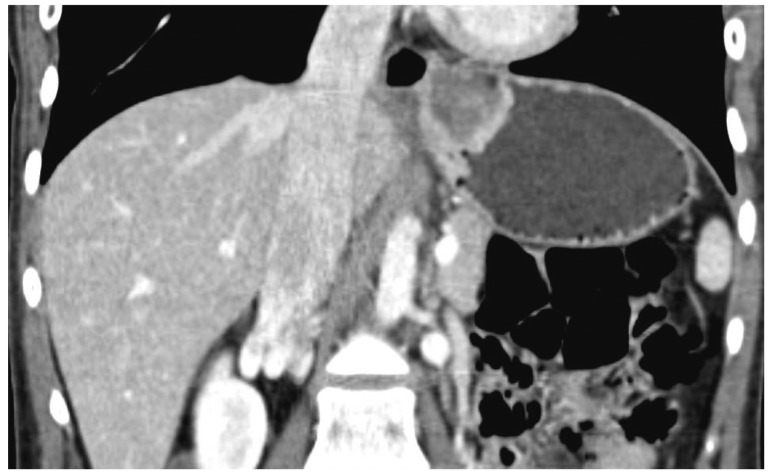
A 25-year-old female patient was referred from an outside hospital in November 2011 for the management of dysphagia. The patient initially presented to a different hospital in 2008 with a 4-year history of heartburn and acid regurgitation and was diagnosed with GERD. The patient did not complain of dysphagia or globus symptoms at the time, and the esophagogastroduodenoscopy (EGD) performed at the previous hospital showed grade B erosive esophagitis according to LA classification. A 24-hour intraesophageal pH study showed a DeMeester score of 33.1 (normal value, <14.2), a total fraction time of pH <4 of 9%, and abnormal acid regurgitation when the patient was upright (upright fraction time of pH <4, 24%). Preoperative esophageal manometry showed normal lower esophageal sphincter (LES) relaxation during swallowing (resting LES pressure 14 mm Hg to LES relaxation 2 mm Hg), and no peristalsis was observed in the esophageal body (Fig. 1). A favorable response to medical treatment (proton pump inhibitor) was not achieved, and subsequent laparoscopic Nissen fundoplication was performed in September 2009 in a previous hospital. Thereafter, the patient developed postoperative complications such as solid and liquid dysphagia, a sensation of inability to belch, and a sticking sensation in her lower to mid chest. Approximately 2 to 3 weeks after the operation, the patient's symptoms showed improvement. However, regurgitation recurred and was soon aggravated to dysphagia. Dysphagia was worse with solids than with liquids, and these symptoms occurred whenever the patient swallowed food. Medical therapy with proton pump inhibitors and prokinetics was attempted in the previous hospital but was ineffective. The patient was then referred to our hospital. EGD performed at our hospital showed postfundoplication status, and the endoscope could pass through the gastroesophageal junction without any resistance (Fig. 2). The previously observed erosive esophagitis was improved. Esophageal mucosal biopsies ruled out eosinophilic esophagitis. Abnormal barium stasis in the esophageal body was found on barium esophagography (Fig. 3A). A paraesophageal hernia was observed on abdominopelvic computed tomography (Fig. 4), which was performed to evaluate the patient for postoperative organic causes of dysphagia. Esophageal manometry showed aperistalsis in the esophageal body, and the resting pressure and percent relaxation of LES were 5 mm Hg and 81%, respectively, which were within the normal range (Fig. 5). In our hospital, medical treatment (prokinetics, mosapride 15 mg; proton pump inhibitor, esomeprazole 40 mg; calcium channel blocker, nifedipine 5 mg) was initiated and continued for 2 months; however, a favorable outcome was not obtained. Pneumatic dilatation with a 30-mm balloon was used for symptom relief, but the symptoms did not improve. Therefore, additional pneumatic dilation with a 35-mm balloon was performed 2 weeks later. Barium esophagography performed after the second pneumatic dilatation showed improved barium passage through the esophagus, but the solid and liquid dysphagia, and globus sensation symptoms were not improved (Fig. 3B). We considered esophageal motility disorder or paraesophageal hernia that developed after fundoplication as the most likely cause of the dysphagia. Therefore, we recommended a revision operation that would involve taking down the wrap or Toupet fundoplication. However, the patient refused to consent to a second operation and is currently undergoing medical treatment.
Severe or persistent dysphagia (with symptoms lasting more than 3 months) is reported in 3% to 24% of fundoplication cases. Dysphagia that persists for more than 12 weeks requires evaluation. Dysphagia of this magnitude may be related to underlying motility abnormalities, esophageal stricture, or the surgery itself. Causative factors related to the operation may include an excessively tight fundoplication, paraesophageal hernia, or intrathoracic migration of the fundoplication (slipped fundoplication).4,5
Esophageal motility disorders can contribute to postoperative dysphagia. Nonspecific motility disorders are common in patients with GERD, and antireflux surgery can be tailored to the underlying motility problem.1,4 In patients with GERD and aperistalsis, the main surgical question involves the type of fundoplication (partial or full) to perform to achieve the best results, and conflicting findings have been reported in the literature.1-3 Some reports indicate that the occurrence of postoperative complications such as dysphagia and globus sensation does not depend on the surgical method but rather on the presence of preoperative dysphagia.1,6 Accordingly, our patient was likely to have residual dysphagia because preoperative esophageal manometry revealed aperistalsis, and the patient had reflux symptoms along with dysphagia prior to the operation. In patients showing severe persistent symptoms despite medical treatment, pneumatic dilatation is a treatment option. Endoscopic dilatation is safe and often effective in patients with postfundoplication dysphagia. However, patients with slipped fundoplication and patients who have undergone multiple fundoplications respond poorly to endoscopic dilatation.4,7 Moreover, atypical symptoms such as chest pain, epigastric pain, and bloating do not resolve after dilatation.4
To improve dysphagia in our patient, pneumatic dilatation was attempted twice and led to radiological but not clinical improvement. We believe that her residual dysphagia was secondary to esophageal aperistalsis rather than GERD.
Granderath et al.8 compared 3-month postoperative outcomes between patients who underwent laparoscopic Toupet fundoplication and those who underwent Nissen fundoplication and found that gas-related symptoms occurred with less frequency in the Toupet group. Furthermore, they noted a positive association between immediate postoperative belching and reduced gas-related complications.8 In the present case, the patient experienced gas-related symptoms such as inability to belch and gastric fullness during the initial diagnosis of GERD, indicating that Toupet fundoplication may have been a better choice as an initial operation. Therefore, we recommended Toupet fundoplication as a revisional surgery to relieve dysphagia and globus sensation, but the patient refused and is currently being observed with medical therapy. In patients with GERD, we emphasize the importance of a thorough preoperative evaluation including a clear understanding of symptoms. In addition, esophageal manometry, barium esophagography, and 24-hour intraesophageal pH study should be performed before performing an antireflux surgery for GERD. If evaluations reveal that aperistalsis is combined with refractory GERD, the choice of surgical approach is important. In addition, patients with preoperative dysphagia should be made aware that unlike reflux symptoms, dysphagia may not improve with surgery. Further studies are needed to identify more efficient surgical or medical methods for the treatment of patients with both refractory GERD and aperistalsis.
References
1. Tsereteli Z, Sporn E, Astudillo JA, Miedema B, Eubanks WS, Thaler K. Laparoscopic Nissen fundoplication is a good option in patients with abnormal esophageal motility. Surg Endosc. 2009; 23:2292–2295. PMID: 19172353.

2. Novitsky YW, Wong J, Kercher KW, Litwin DE, Swanstrom LL, Heniford BT. Severely disordered esophageal peristalsis is not a contraindication to laparoscopic Nissen fundoplication. Surg Endosc. 2007; 21:950–954. PMID: 17177077.

3. Chan WW, Haroian LR, Gyawali CP. Value of preoperative esophageal function studies before laparoscopic antireflux surgery. Surg Endosc. 2011; 25:2943–2949. PMID: 21424193.

4. Malhi-Chowla N, Gorecki P, Bammer T, Achem SR, Hinder RA, Devault KR. Dilation after fundoplication: timing, frequency, indications, and outcome. Gastrointest Endosc. 2002; 55:219–223. PMID: 11818926.

5. Mattox HE 3rd, Albertson DA, Castell DO, Richter JE. Dysphagia following fundoplication: "slipped" fundoplication versus achalasia complicated by fundoplication. Am J Gastroenterol. 1990; 85:1468–1472. PMID: 2239875.
6. Herron DM, Swanström LL, Ramzi N, Hansen PD. Factors predictive of dysphagia after laparoscopic Nissen fundoplication. Surg Endosc. 1999; 13:1180–1183. PMID: 10594261.

7. Wo JM, Trus TL, Richardson WS, et al. Evaluation and management of postfundoplication dysphagia. Am J Gastroenterol. 1996; 91:2318–2322. PMID: 8931410.
8. Granderath FA, Kamolz T, Granderath UM, Pointner R. Gas-related symptoms after laparoscopic 360 degrees Nissen or 270 degrees Toupet fundoplication in gastrooesophageal reflux disease patients with aerophagia as comorbidity. Dig Liver Dis. 2007; 39:312–318. PMID: 17306636.
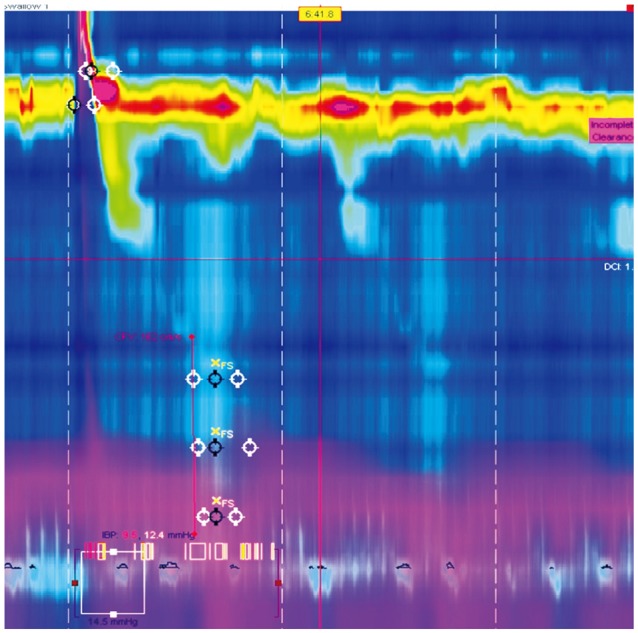
Fig. 1
Preoperative manometry showing normal lower esophageal sphincter relaxation during swallowing, and no peristalsis was seen in the esophageal body.
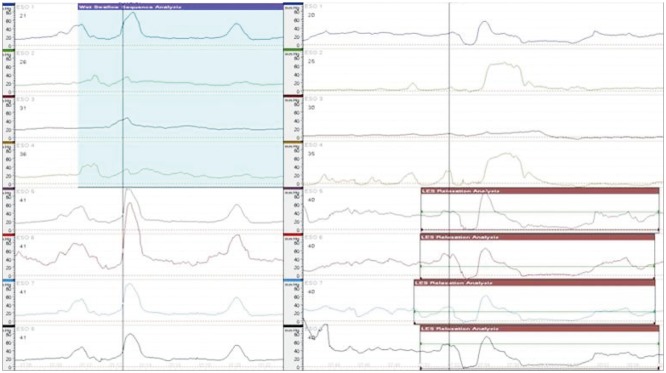
Fig. 2
(A) Postoperative esophagogastroduodenoscopic images showing postfundoplication status. (B) The endoscope could pass through the gastroesophageal junction without any resistance.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download