Abstract
Background/Aims
Between endoscopic sphincterotomy (ES) alone and combined endoscopic sphincterotomy and large balloon dilation (ES-LBD) groups, efficacy and long-term complications, difference in biliary stone recurrence rate, and risk factors of stone recurrence were compared.
Methods
Medical records of 222 patients who underwent ERCP for biliary stone removal were retrospectively reviewed. Patients with dilated CBD ≥11 mm and follow-up longer than 6 months were included.
Results
There were 101 patients in ES-LBD group and 121 patients in ES group. Mean follow-up duration was 25.0 (6-48) months and 13.0 (6-43) months, respectively (p=0.001). There was no difference in number of ERCP sessions, brown pigment stones, angle between mid and distal common bile duct (CBD angle) <135°, and lithotripsy rate. Complete retrieval success rate was excellent in both groups (100% vs. 99%). Early complication rate of ES-LBD and ES alone group was 4 and 4.1%, respectively (p=1.000). One patient in ES-LBD group died from delayed bleeding. Late complication rate was 5.9 and 3.3%, respectively (p=1.000). Stone recurrence rate was 6.9% and 5.8%, respectively (p=0.984). The only Independent risk factor of stone recurrence was presence of periampullary diverticulum.
Go to : 
Since the introduction of endoscopic sphincterotomy followed by endoscopic papillary balloon dilation (ES-EPBD) in 2003,1 immediate and acute complications of this procedure have been well studied.2,3 Long-term outcome after ES-EPBD with a ≤8 mm balloon is also known.4,5 However, long-term outcome after ES followed by large balloon dilation (ES-LBD, ≥12 mm) has not been established yet. Since the results of an ex vivo animal study showed that ES-LBD can damage the bile duct wall and cause potential impairment of sphincter of Oddi function and overdilation of extrahepatic bile ducts,6 long-term outcome after ES-LBD may be different from that of ES-EPBD using a balloon with smaller diameter. The aim of this study was to retrospectively compare ES alone and ES-LBD groups in regard to efficacy and late complications, difference in bile duct stone recurrence rate, and risk factors of stone recurrence.
Go to : 
From December 2004 to March 2009, patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) for bile duct stone removal were included if they met all of the following criteria: 1) age >18 years, 2) first trial of ERCP (virgin papilla), 3) dilated common bile duct (CBD) with a diameter of ≥11 mm on a cholangiogram, and 4) follow-up period of ≥6 months either by review of medical records or by phone calls. Patients were excluded if they met any of the following criteria: 1) previous ES, 2) precut or infundibulotomy, 3) previous Billroth II operation, or 4) uncorrected coagulopathy. All patients gave written informed consent before undergoing ERCP for bile duct stone removal.
All ERCP procedures were performed under conscious sedation after intravenous injection of midazolam and pethidine. An Olympus EVIS system, JF-V, or TJF 200 series (Olympus, Tokyo, Japan) was used for ERCP. A generator with an automatically controlled cutout system (Endocut mode) was used for all ES. Selective bile duct cannulation was performed, and cholangiogram was obtained. After the assessment of number and size of bile duct stones and diameter of the bile duct, either ES alone or ES-LBD was chosen at discretion of the endoscopist. A pull-type papillotome (Autotome RX44; Boston Scientific Corp., Natick, MA, USA) was used for sphincterotomy. In the ES-alone group, ES was performed up to the major horizontal fold of the major duodenal papilla. In the ES-LBD group, ES was performed up to the mid-portion of the major duodenal papilla. Then, a wire-guided balloon dilation catheter with a diameter of ≥12 mm was used for LBD (CRE™ Wireguided; Boston Scientific Corp., Natick, MA, USA). Bile duct stones were removed with a basket or a retrieval balloon. A mechanical lithotripter was used when stones could not be retrieved after either maximal ES (in the ES-alone group) or balloon dilation after ES (in the ES-LBD group). After removal of bile duct stones, a 7 Fr nasobiliary catheter (Nagaraja Nasal Biliary Drainage; Wilson-Cook Medical Inc., Winston-Salem, NC, USA) was placed. Cholangiogram through a nasobiliary catheter was obtained one or two days later.
The following parameters were assessed and compared between the two groups:
• Patient characteristics
• Bile duct stone characteristics: number, maximal diameter of the largest stone, type, requirement for lithotripsy
• Complication rate: bleeding, hyperamylasemia, pancreatitis, perforation
• Stone recurrence rate
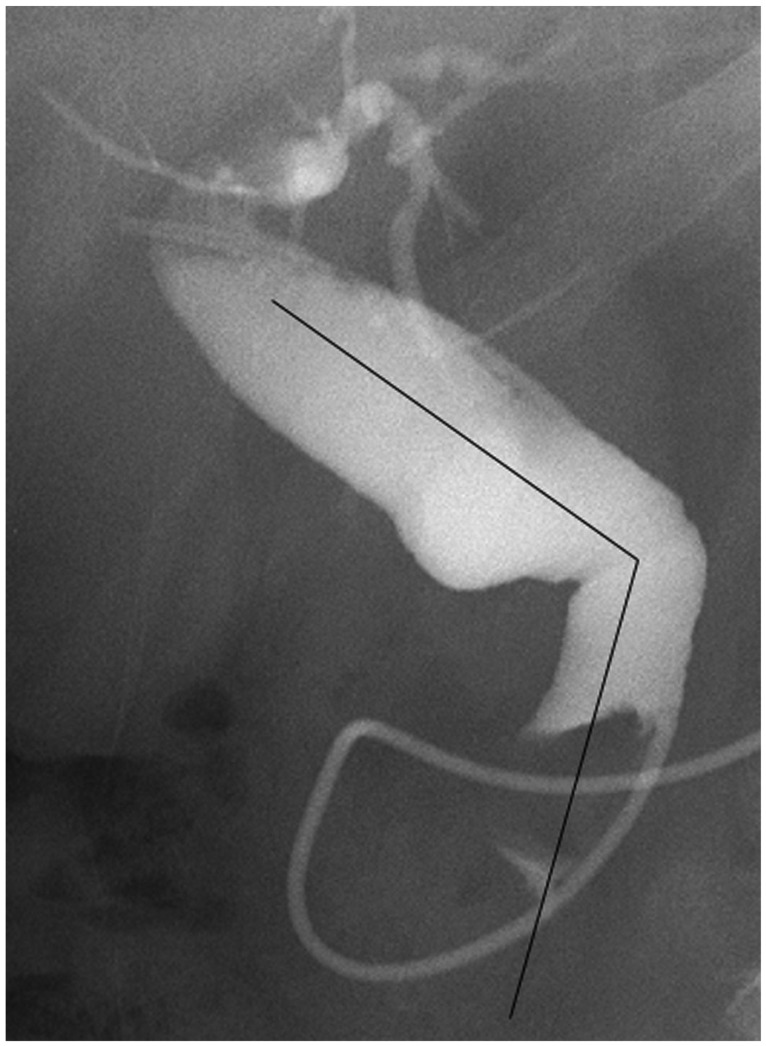
• Risk factors of stone recurrence: CBD angle (Fig. 1), periampullary diverticulum, intrahepatic duct stone, common hepatic duct stricture, history of cholecystectomy, gallbladder stones left in situ, mechanical lithotripsy, CBD diameter after stone extraction
Definitions of complications related to ES and ES-LBD were similar to those of Cotton et al.7 Minor bleeding was defined as a decrease of at least 2 g/dL in the hemoglobin concentration and achievement of hemostasis during the same procedure. Major bleeding was defined as interruption of the procedure, clinical evidence of bleeding such as melena or hematemesis with a decrease of at least 2 g/dL in hemoglobin concentration, or the need for at least two units of packed red blood cell transfusion. Delayed bleeding was defined as bleeding that developed after the procedure. Procedure-induced hyperamylasemia was defined as an increase in the serum amylase level ≥3 times that of the upper normal limit without pancreatic pain and normalized serum amylase level within 2 days. Procedure-induced pancreatitis was defined as the development of pancreatic pain with an increase in the serum amylase level ≥3 times that of the upper normal limit lasting over 2 days. Early complication was defined as complication that developed within 72 hours after the procedure and included bleeding, hyperamylasemia, post-ERCP pancreatitis, perforation, and death. Late complication was defined as complication that occurred more than 72 hours after the procedure and included recurrent cholangitis, biliary pancreatitis, bile duct stricture, and cholecystitis. CBD angle was defined as the first angulation from the ampullary orifice along the course of CBD, and measured on the cholangiogram (Fig. 1).8 Bile duct stone recurrence was defined as presence of biliary pain and abnormal liver function test results and/or bile duct stone detected on an abdominal computed tomography scan.
Statistical analysis was performed with SPSS version 14.0 software for Windows (SPSS Inc., Chicago, IL, USA). Values were presented as median with range. Potentially relevant risk factors were assessed by univariate analysis with the chi-square statistic for categorical variables and simple logistic regression for continuous variables. Significant factors (p<0.1) from univariate analysis were included in a forward, stepwise multiple logistic regression model to identify the risk factors for recurrent bile duct stones. A p<0.05 was considered statistically significant.
Go to : 
There were 101 patients in the ES-LBD group and 121 patients in the ES-alone group. Baseline characteristics of the patients are summarized in Table 1. There was no significant difference between the two groups except for age, presence of gallbladder stone and periampullary diverticulum, and follow-up duration.
Bile duct stones in the ES-LBD group were greater in number and larger in maximal diameter than those in the ES alone group (1.0 [1 to ≥5] vs. 2.0 [1 to ≥5], p=0.001; 10.0 [2 to 20] vs. 12.0 [3 to 25] mm, p=0.000, respectively). However, there was no significant difference between the ES-LBD and ES-alone groups regarding number of ERCP sessions for removal, number of patients with brown pigment stones, use of lithotripsy, and complete removal rate (1.0 [1 to 3] vs. 1.0 [1 to 4], p=0.149; 80 [79.2%] vs. 94 [75.2%], p=0.870; 25 [24.8%] vs. 33 [27.3%], p=0.759; 100 [99%] vs. 121 [100%], p=0.455, respectively).
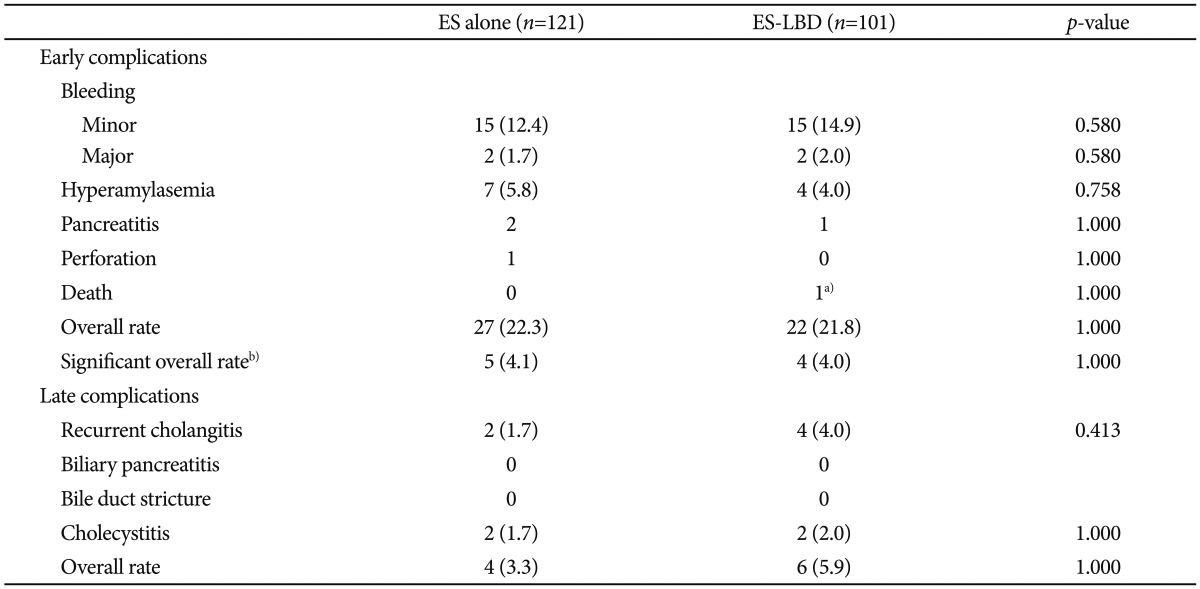
Complications related to ES and ES-LBD are summarized in Table 2. The most common early complication in both groups was minor bleeding (15/121 vs. 15/101; p=0.580). One death occurred in the ES-LBD group from delayed major bleeding and rapid development of hypovolemic shock that did not respond to resuscitation and intervention. The most common late complication in both groups was recurrent cholangitis (2/121 vs. 4/101; p=0.413). Acute cholecystitis occurred in two patients of each group (p=1.000).
Bile duct stone recurred in seven patients from the ES-alone group and seven patients from the ES-LBD group (5.8% vs. 6.9%; p=0.786). Between the two groups, there was no significant difference in sex and age of the patients with bile duct stone recurrence (5 males vs. 2 males, p=0.286; 79.0 [46 to 83] years vs. 75.0 [51 to 87] years, p=0.932, respectively). Also, there was no significant difference in maximal bile duct diameter, maximal stone diameter, and number of bile duct stones (14.0 [10 to 17] mm vs. 14 [12 to 15] mm, p=0.788; 11.0 [6 to 15] mm vs. 14.0 [3 to 21] mm, p=0.289; 2.0 [1 to ≥5] vs. 5.0 [1 to ≥5], p=0.052, respectively). Presence of periampullary diverticulum was not different between the two groups (1/7 vs. 2/7; p=0.515). Mechanical lithotripsy was performed in three patients of the ES-alone group and five patients of the ES-LBD group (p=0.280). Patients with recurrent bile duct stones had gallbladder stones left in situ in two patients from the ES-alone group and two from the ES-LBD group (p=1.000). CBD angle did not show significant difference between patients with recurrent bile duct stones from the ES-alone and ES-LBD groups (<90°, 1 vs. 1, p=0.409; 90° to 135°, 3 vs. 4, p=1.000; 135° to 180°, 3 vs. 2, p=0.181, respectively). Time to recurrence and follow-up duration of patients with recurrent bile duct stones from each group did not show significant difference (16.0 [10 to 42] months vs. 14.0 [1 to 35] months, p=0.395; 36 [13 to 44] months vs. 20.0 [6 to 42] months, p=0.202, respectively).
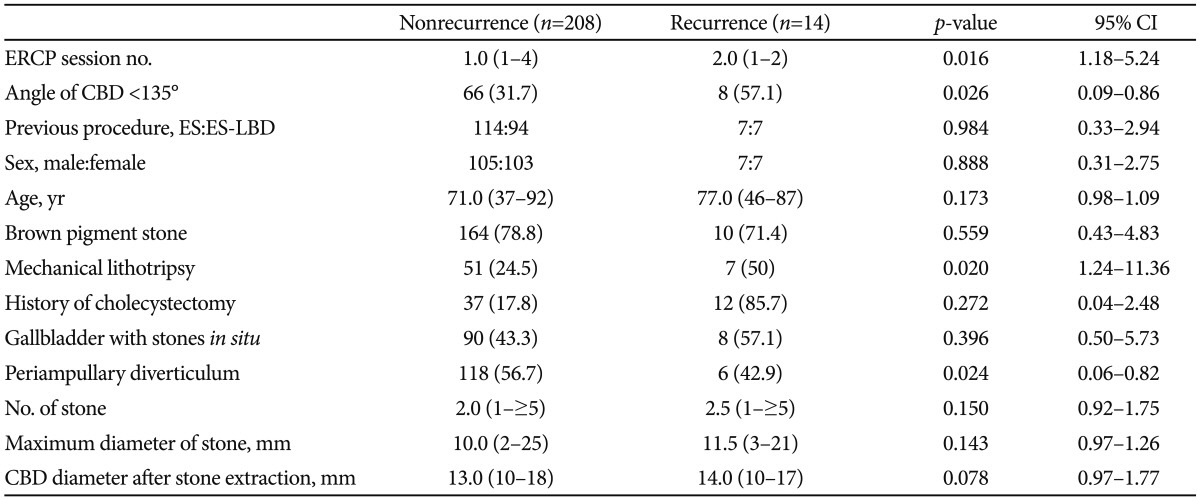
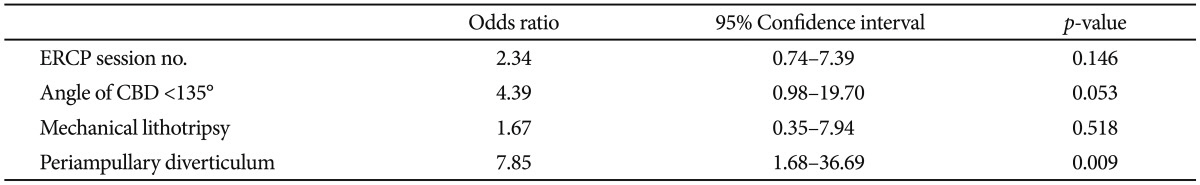
Because there was no significant difference between the ES-alone and ES-LBD groups in respect to potential risk factors for bile duct stone recurrence, risk factors for bile duct stone recurrence in the entire study subjects were investigated. In univariate analysis, the risk factors for bile duct stone recurrence were number of ERCP sessions to clear CBD stones, CBD angle of <135°, need for mechanical lithotripsy, and presence of periampullary diverticulum (Table 3). Multivariate analysis showed that presence of periampullary diverticulum was the only independent risk factor for bile duct stone recurrence (odds ratio, 7.85; 95% confidence interval, 1.68 to 36.69; p=0.009) (Table 4).
Go to : 
In this study, the long-term outcome of ES-LBD in patients with CBD stones was not significantly different from that of ES alone with regard to recurrent cholangitis, cholecystitis, and bile duct stone recurrence. This finding may be explained by possible permanent disruption of sphincter function by ES-LBD. Preservation of sphincter function is a well-known advantage of EPBD9,10 and has been the basis for lower rate of late biliary complications after EPBD. However, an ex vivo animal study demonstrated that balloons with diameters of ≥12 mm disrupt integrity of the bile duct wall and sphincter function.6 Because of differences between the ex vivo animal model and humans in clinical practice (i.e., compliance of the bile duct, thickness of the fibromuscular layer, and different anatomy), findings of the animal study may not be directly applicable to clinical practice.6 Nevertheless, irreversible loss of sphincter function by ES-LBD may result in duodenobiliary reflux similar to that by ES alone. This reflux of duodenal contents into the biliary system may be associated with bacterial colonization and can cause recurrent bile duct stones, ascending cholangitis, and acute cholecystitis.11 Also, long-term outcome of ES-LBD may have been affected by older age and greater prevalence of gallbladder stone and periampullary diverticulum in this group. Older age and periampullary diverticulum are known risk factors of bile duct stone recurrence.12,13 On the other hand, these factors may prompt the use of ES-LBD for stone removal. Gallbladder stone is a known risk factor for bile duct stone recurrence.14,15 Cholecystectomy is usually recommended to prevent bile duct stone recurrence. However, the bile duct stone recurrence rate did not differ between the ES-alone and ES-LBD groups with regard to the presence of gallbladder or gallbladder stones. This may result from predominance of brown pigment stones in the study subjects. Also, there have been concerns about papillary stricture in ES-LBD.16 In this study, there was no papillary stricture during the follow-up.
Bile duct stone recurrence rate after ES-LBD was 6.9%, which was similar to that of previous studies that evaluated ES-EPBD or EPBD alone.4,5,14 There was no significant difference in potential risk factors for bile duct stone recurrence between the ES alone and the ES-LBD group. Therefore, the risk factors for bile duct stone recurrence in the entire study subjects were evaluated. Multivariate analysis showed that presence of periampullary diverticulum was the only independent risk factor for bile duct stone recurrence. This finding was not much different from known risk factors. A previous study showed that the risk factors for CBD stone recurrence after ES only include older age, dilation of the CBD (≥13 mm), previous open or laparoscopic cholecystectomy, presence of periampullary diverticulum, and more acute CBD angulation (≤145°).17 Known risk factors for recurrent stones after ES and EPBD vary from study to study and include presence of a periampullary diverticulum, gallbladder stones left in situ, dilated CBD, previous cholecystectomy, no confirmation of a clean duct on intraductal ultrasonography, and mechanical lithotripsy.5,14,15,18 Risk factors for recurrent stones after ES-LBD are less well studied. One recent study reported that a dilated bile duct (≥22 mm) predicted stone recurrence in patients who underwent ES-LBD.19 Although acute CBD angle did not reach statistical significance in multivariate analysis, this may result in bile stasis and stone recurrence. The number of ERCP sessions needed to clear CBD stones implies multiplicity and difficulty in removing all the stones. To decrease the number of ERCP sessions needed to clear bile duct stones and prevent stone recurrence, intraductal ultrasonography, or direct peroral cholangioscopy may be useful for documenting the complete clearance of bile duct stones, but it is not universally available.20-22 On the other hand, the presence of periampullary diverticulum and an acute CBD angle are risk factors that cannot be modified. Still, these are useful in predicting bile duct stone recurrence and in educating patients at high risk.
Limitations of this study are its retrospective, single-center design and the small number of patients with bile duct stone recurrence. Further prospective, randomized controlled studies with a longer follow-up period and a greater number of patients are needed to overcome these limitations.
In conclusion, ES-LBD for bile duct stones showed similar complete stone removal rate, long-term complication rate, and stone recurrence rate compared with ES alone. The independent risk factor for stone recurrence was presence of periampullary diverticulum.
Go to : 
Acknowledgments
This study was supported by a grant from the Korea Ministry of Health and Welfare, Republic of Korea (project no. A084177).
Go to : 
References
1. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003; 57:156–159. PMID: 12556775.

2. Stefanidis G, Viazis N, Pleskow D, et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011; 106:278–285. PMID: 21045816.

3. Youn YH, Lim HC, Jahng JH, et al. The increase in balloon size to over 15 mm does not affect the development of pancreatitis after endoscopic papillary large balloon dilatation for bile duct stone removal. Dig Dis Sci. 2011; 56:1572–1577. PMID: 20945093.
4. Yasuda I, Fujita N, Maguchi H, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010; 72:1185–1191. PMID: 20869711.

5. Ohashi A, Tamada K, Wada S, et al. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009; 21:73–77. PMID: 19691777.

6. Hisatomi K, Ohno A, Tabei K, Kubota K, Matsuhashi N. Effects of large-balloon dilation on the major duodenal papilla and the lower bile duct: histological evaluation by using an ex vivo adult porcine model. Gastrointest Endosc. 2010; 72:366–372. PMID: 20674625.

7. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393. PMID: 2070995.

8. Kim HJ, Choi HS, Park JH, et al. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007; 66:1154–1160. PMID: 17945223.

9. Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001; 49:686–691. PMID: 11600473.

10. Sato H, Kodama T, Takaaki J, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: evaluation from the viewpoint of endoscopic manometry. Gut. 1997; 41:541–544. PMID: 9391256.

11. Tsujino T, Isayama H, Ito Y, et al. Long-term outcomes (mean follow-up period > 10 years) of endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2008; 67:AB163–AB164.
12. Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc. 2006; 20:1594–1599. PMID: 16858527.

13. Ueno N, Ozawa Y, Aizawa T. Prognostic factors for recurrence of bile duct stones after endoscopic treatment by sphincter dilation. Gastrointest Endosc. 2003; 58:336–340. PMID: 14528204.

14. Kojima Y, Nakagawa H, Miyata A, et al. Long-term prognosis of bile duct stones: endoscopic papillary balloon dilatation versus endoscopic sphincterotomy. Dig Endosc. 2010; 22:21–24. PMID: 20078660.

15. Tsujino T, Kawabe T, Komatsu Y, et al. Endoscopic papillary balloon dilation for bile duct stone: immediate and long-term outcomes in 1000 patients. Clin Gastroenterol Hepatol. 2007; 5:130–137. PMID: 17234559.
16. Lee JH. Is combination biliary sphincterotomy and balloon dilation a better option than either alone in endoscopic removal of large bileduct stones? Gastrointest Endosc. 2007; 66:727–729. PMID: 17905014.

17. Keizman D, Ish Shalom M, Konikoff FM. Recurrent symptomatic common bile duct stones after endoscopic stone extraction in elderly patients. Gastrointest Endosc. 2006; 64:60–65. PMID: 16813804.

18. Yasuda I. Management of the bile duct stone: current situation in Japan. Dig Endosc. 2010; 22(Suppl 1):S76–S78. PMID: 20590777.

19. Kim KH, Rhu JH, Kim TN. Recurrence of bile duct stones after endoscopic papillary large balloon dilation combined with limited sphincterotomy: long-term follow-up study. Gut Liver. 2012; 6:107–112. PMID: 22375179.

20. Ang TL, Teo EK, Fock KM, Lyn Tan JY. Are there roles for intraductal US and saline solution irrigation in ensuring complete clearance of common bile duct stones? Gastrointest Endosc. 2009; 69:1276–1281. PMID: 19249039.

21. Chen YK, Parsi MA, Binmoeller KF, et al. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc. 2011; 74:805–814. PMID: 21762903.

22. Moon JH, Ko BM, Choi HJ, et al. Direct peroral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol. 2009; 104:2729–2733. PMID: 19623165.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download