Abstract
Amyloidosis is characterized by extracellular deposition of insoluble protein fibrils that stain with Congo red application and appear apple green under polarized light. The presenting symptoms result from the involvement of many affected, nonspecific and generalized organ systems. Our patient was an 80-year-old woman with no medical history. She presented with a 2-week history of nausea and vomiting. An esophagogastroduodenoscopy showed erythematous and edematous mucosa on the antrum with pyloric stenosis. Histopathologic examination of the biopsy specimen showed the deposition of amorphous, homogeneous, and acidophilic material in the gastric mucosa. Amyloidal protein was proven by positive Congo red stain. A serum and urine immunfixation electrophoresis showed lambda light chain band. She developed symptoms of repeated greenish color vomiting. A follow-up esophagogastroduodenoscopy showed progressed antral obstruction. However, she refused further evaluation and treatment and was managed conservatively. She later died of disease progression after 34 hospital days.
The term amyloidosis refers to a group of disorders characterized by the extracellular accumulation of insoluble, fibrillar proteins in various organs and tissues.1,2 The fibrils, composed of low-molecular-weight subunits of serum proteins, may be recognized microscopically by their ability to bind to Congo red, resulting in a characteristic green birefringence under polarized light.3 Pathologically, amyloidoses were classified as either systemic (amyloid A, amyloid light-chain [AL], amyloid transthyretin, amyloid β2 microglobulin) or localized (AL, amyloid, β2 microglobulin) diseases.2 Systemic amyloidoses include primary, secondary/reactive, and heredofamilial amyloidosis, while localized amyloidoses includes several diseases with specific targeted organs. The gastrointestinal tract is one of the regions commonly involved with the systemic amyloidosis. However, systemic amyloidosis that presents with gastric outlet obstruction is a rare occurrence.4 We report a case of gastric outlet obstruction manifested by systemic AL amyloidosis.
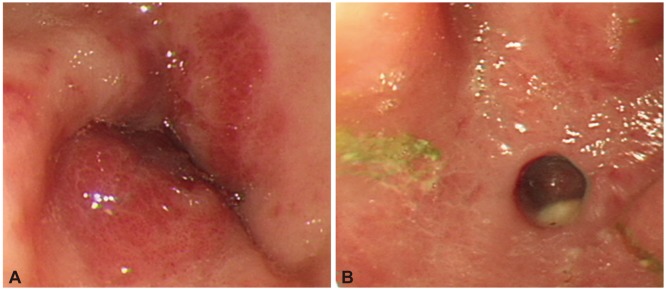
An 80-year-old female presented to Division of Gastroenterology, Department of Internal Medicine, Chung-Ang Medical Center with a complaint of a 2-week history of vomiting. She was a nonsmoker, did not consume alcohol and had no previously diagnosed disease. The patient complained of epigastric pain and had mild epigastric tenderness. She was admitted to the hospital for evaluation and treatment. Laboratory data revealed anemia (9.5 g/dL), but she had a white blood cell and a platelet count within normal ranges. Serum chemistry indicated a hypoproteinemia and hypoalbuminemia (total protein, 5 g/dL; albumin, 1.7 g/dL), but without abnormal liver or renal function. An esophagogastroduodenoscopy showed erythematous and edematous mucosa on the antrum with pyloric stenosis (Fig. 1A). A computed tomography scan with contrast revealed diffuse wall thickening in the antrum of the stomach with partial gastric outlet obstruction, and without either perigastric fat infiltration or regional lymphadenopathy (Fig. 2). Histopathologic examination showed the deposition of amorphous, homogeneous, and acidophilic material in the gastric mucosal. The amyloidal protein was proven by a positive Congo red stain result (Fig. 3). Immunohistochemistry performed on biopsy results was C-kit (-), SMA (-), CD34 (-), S-100 (-), and Ki-67 (<1%).
The existence of a gastric amyloid tumor suggested systemic amyloidosis. Therefore, we did blood examinations, rapid plama reagin, rheumatoid factor, urinalysis, chest-abdominal simple X-ray examinations, skull and pelvic series, rectal biopsy with sigmoidoscopy, electrocardiography, and cardiac ultrasonography. A serum and urine immunfixation electrophoresis showed abnormal band of restriction in lambda light chain, suggesting monoclonal component. The cardiac ultrasonography had shown a small amount of pericardial effusion and diastolic dysfunction grade I. Small amounts of both pleural effusion and ascites were noted on the computed tomography scan. Other examinations revealed no specific finding. She was diagnosed with AL type systemic amyloidosis that presented as gastric outlet obstruction.
During her admission, she developed symptoms, repeated bile color vomiting, malabsorption, systemic edema, dyspnea, and melena. On hospital day 14, a follow-up esophagogastroduodenoscopy showed progressed infiltration type gastric outlet obstruction and a single hole was noted on the antrum of nasogastric tube insertions site (Fig. 1B). During the esophagogastroduodenoscopy, the scope did not pass through the pylorus. She refused further evaluation and treatment such as chemotherapy or surgery. Instead, she was managed conservatively with total parenteral nutrition therapy and intravenous proton pump inhibitor. She died of disease progression after 34 hospital days.
Amyloidosis was categorized according to the tissue distribution of amyloid (e.g., systemic vs. localized amyloidosis) and the presence or absence of the identifiable predisposing factors (e.g., secondary vs. primary amyloidosis). A diagnosis of AL amyloidosis may be suspected on clinical grounds. The presenting symptoms include: weight loss, fatigue, edema, pain or numbness due to peripheral neuropathy, and purpura, and patients occasionally have hepatosplenomegaly, enlarged lymph nodes or carpal tunnel syndrome.5 Multisystem organ involvement is typical, affecting the kidney, heart, peripheral nerves, and gastrointestinal tract.5,6
Gastrointestinal disease in amyloidosis may result from mucosal infiltration, neuromuscular infiltration, or from autonomic neuropathy.3 In a study of intestinal pseudo-obstruction resulting from amyloidosis, extensive infiltration and replacement of the muscularis propria by amyloid deposits was found in two patients with AL amyloidosis.7 In a case involving the stomach, endoscopic features may be nonspecific. In stomach erosions, hemorrhagic spots on the antral folds and ulcers resulting from occlusion of submucosal vessels which follows amyloid deposits are characteristic.8 Systemic amyloidosis of the stomach simulating an obstructing gastric cancer is rarely reported.9 In patients with systemic amyloidosis presenting with gastric outlet obstruction, regional amyloid deposits are difficult to diagnose due to nonspecific symptoms and the endoscopic findings. First of all, this is due in part to very rare disease of gastric outlet obstruction with extensive infiltration by an amyloidosis being difficult to diagnose. Therefore, active biopsy is necessary in the differential diagnosis from other more common diseases such as ulcer or carcinoma.
References
1. Enqvist S, Sletten K, Stevens FJ, Hellman U, Westermark P. Germ line origin and somatic mutations determine the target tissues in systemic AL-amyloidosis. PLoS One. 2007; 2:e981. PMID: 17912358.

2. Deniz K, Sari I, Torun E, Patiroglu TE. Localized gastric amyloidosis: a case report. Turk J Gastroenterol. 2006; 17:116–119. PMID: 16830294.
3. Goulding C, O'Hanlon DM, Clarke E, Kennedy M, Lennon J. Primary amyloidosis of the stomach: EUS appearances. Gastrointest Endosc. 2002; 56:305–306. PMID: 12145619.

4. Rotondano G, Salerno R, Cipolletta F, et al. Localized amyloidosis of the stomach: a case report. World J Gastroenterol. 2007; 13:1877–1878. PMID: 17465486.

5. Rihova Z, Merta M, Spicka I, et al. Unusual manifestation of AL amyloidosis: stenosis of inferior vena cava. Nephrol Dial Transplant. 2006; 21:1430–1433. PMID: 16507582.
6. Gertz MA, Merlini G, Treon SP. Amyloidosis and Waldenström's macroglobulinemia. Hematology Am Soc Hematol Educ Program. 2004; 257–282. PMID: 15561687.
7. Tada S, Iida M, Yao T, Kitamoto T, Yao T, Fujishima M. Intestinal pseudo-obstruction in patients with amyloidosis: clinicopathologic differences between chemical types of amyloid protein. Gut. 1993; 34:1412–1417. PMID: 8244111.

8. Rivera RA. Endoscopic findings in gastroduodenal amyloidosis: case report. Gastrointest Endosc. 1971; 17:137–144. PMID: 5087334.
9. Losanoff JE, Antaki F, Salwen WA, et al. Amyloid tumor of the stomach simulating an obstructing gastric carcinoma: case report and review of the literature. Endoscopy. 2009; 41(Suppl 2):E45–E46. PMID: 19288419.

Fig. 1
Gastric outlet obstruction on the esophagogastroduodenoscopy. (A) Erythematous, edematous mucosa was shown at the antrum at the hospital day 1. (B) Antral obstruction was noted at the hospital day 14, due to amyloidosis. A single hole was noted on the antrum of nasogastric tube insertions site. Gastric outlet obstruction had progressed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download