1. Vincent M, Smith LE. Management of perforation due to colonoscopy. Dis Colon Rectum. 1983; 26:61–63. PMID:
6600423.

2. Lo AY, Beaton HL. Selective management of colonoscopic perforations. J Am Coll Surg. 1994; 179:333–337. PMID:
8069431.
3. Jentschura D, Raute M, Winter J, Henkel T, Kraus M, Manegold BC. Complications in endoscopy of the lower gastrointestinal tract. Therapy and prognosis. Surg Endosc. 1994; 8:672–676. PMID:
8059305.
4. Iqbal CW, Chun YS, Farley DR. Colonoscopic perforations: a retrospective review. J Gastrointest Surg. 2005; 9:1229–1235. PMID:
16332478.

5. Raju GS, Saito Y, Matsuda T, Kaltenbach T, Soetikno R. Endoscopic management of colonoscopic perforations (with videos). Gastrointest Endosc. 2011; 74:1380–1388. PMID:
22136781.

6. Fujishiro M, Yahagi N, Nakamura M, et al. Endoscopic submucosal dissection for rectal epithelial neoplasia. Endoscopy. 2006; 38:493–497. PMID:
16767585.

7. Onozato Y, Kakizaki S, Ishihara H, et al. Endoscopic submucosal dissection for rectal tumors. Endoscopy. 2007; 39:423–427. PMID:
17354181.

8. Tamegai Y, Saito Y, Masaki N, et al. Endoscopic submucosal dissection: a safe technique for colorectal tumors. Endoscopy. 2007; 39:418–422. PMID:
17516348.

9. Saito Y, Uraoka T, Matsuda T, et al. Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissections (with video). Gastrointest Endosc. 2007; 66:966–973. PMID:
17524403.

10. Tanaka S, Oka S, Kaneko I, et al. Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc. 2007; 66:100–107. PMID:
17591481.

11. Byeon JS, Yang DH, Kim KJ, et al. Endoscopic submucosal dissection with or without snaring for colorectal neoplasms. Gastrointest Endosc. 2011; 74:1075–1083. PMID:
21663905.

12. Zhou PH, Yao LQ, Qin XY. Endoscopic submucosal dissection for colorectal epithelial neoplasm. Surg Endosc. 2009; 23:1546–1551. PMID:
19263116.

13. Nishiyama H, Isomoto H, Yamaguchi N, et al. Endoscopic submucosal dissection for colorectal epithelial neoplasms. Dis Colon Rectum. 2010; 53:161–168. PMID:
20087091.

14. Kim ES, Cho KB, Park KS, et al. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy. 2011; 43:573–578. PMID:
21448852.

15. Lee EJ, Lee JB, Choi YS, et al. Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg Endosc. 2012; 26:1587–1594. PMID:
22179462.

16. Yang DH, Byeon JS, Lee KH, et al. Is endoscopic closure with clips effective for both diagnostic and therapeutic colonoscopy-associated bowel perforation? Surg Endosc. 2010; 24:1177–1185. PMID:
19915907.

17. Swan MP, Bourke MJ, Moss A, Williams SJ, Hopper A, Metz A. The target sign: an endoscopic marker for the resection of the muscularis propria and potential perforation during colonic endoscopic mucosal resection. Gastrointest Endosc. 2011; 73:79–85. PMID:
21184872.

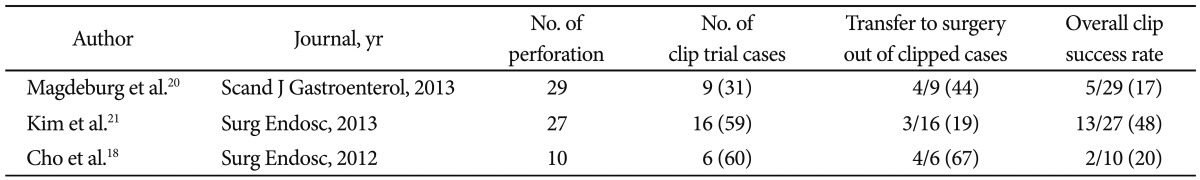
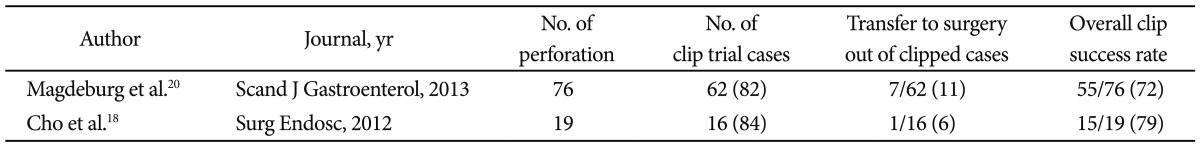
18. Cho SB, Lee WS, Joo YE, et al. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc. 2012; 26:473–479. PMID:
21938583.

19. Yoshikane H, Hidano H, Sakakibara A, et al. Endoscopic repair by clipping of iatrogenic colonic perforation. Gastrointest Endosc. 1997; 46:464–466. PMID:
9402126.

20. Magdeburg R, Sold M, Post S, Kaehler G. Differences in the endoscopic closure of colonic perforation due to diagnostic or therapeutic colonoscopy. Scand J Gastroenterol. 2013; 48:862–867. PMID:
23697700.

21. Kim JS, Kim BW, Kim JI, et al. Endoscopic clip closure versus surgery for the treatment of iatrogenic colon perforations developed during diagnostic colonoscopy: a review of 115,285 patients. Surg Endosc. 2013; 27:501–504. PMID:
22773239.

22. Mocciaro F, Curcio G, Tarantino I, et al. Tulip bundle technique and fibrin glue injection: unusual treatment of colonic perforation. World J Gastroenterol. 2011; 17:1088–1090. PMID:
21451724.
23. Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos). Gastrointest Endosc. 2010; 72:881–886. PMID:
20646699.

24. Gubler C, Bauerfeind P. Endoscopic closure of iatrogenic gastrointestinal tract perforations with the over-the-scope clip. Digestion. 2012; 85:302–307. PMID:
22614286.

25. Yoon JY, Kim JH, Lee JY, et al. Clinical outcomes for patients with perforations during endoscopic submucosal dissection of laterally spreading tumors of the colorectum. Surg Endosc. 2013; 27:487–493. PMID:
22806523.








 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download