Abstract
Bezoars are concretions of undigested material and are most often observed in the stomach. They can occur at any site in the gastrointestinal tract; however, duodenal localization is very rare. We report the case of a 71-year-old male who had undergone subtotal gastrectomy with gastroduodenostomy and experienced severe epigastric discomfort, abdominal pain, and vomiting for a few days. An approximately 7×8 cm-sized mass was found on an abdominal computed tomography scan. On following endoscopy, a large bezoar was revealed in the duodenum and was removed using an endoscopic removal technique, assisted by a large amount of Coca-Cola infusion.
Go to : 
A bezoar is a ball of swallowed foreign material usually composed of hair or fiber and located anywhere in the gastrointestinal tract. The incidence is low in humans and has been reported as 0.4% in the general population.1 They are found more often in patients who have altered gastrointestinal motility and/or anatomy due to previous gastric surgery. Despite the low incidence, bezoars are associated with a high mortality because they can cause gastrointestinal bleeding or perforation.2 Therefore, it is very important to remove a bezoar using endoscopic or surgical removal, in order to prevent further complications. Recently, nasogastric lavage or endoscopic infusion of Coca-Cola has been used as efficient methods to dissolve bezoars in some patients.3
Large bezoars are generally retained in the stomach, most likely due to the presence of the pyloric sphincter; however, patients who have undergone gastric surgery are sometimes exceptions. We report a case of duodenal bezoar in a 71-year-old male who had a history of surgery due to gastric cancer presenting with intestinal obstructive symptoms.
Go to : 
A 71-year-old male, who 8 years previously had undergone subtotal gastrectomy with gastroduodenostomy because of early gastric cancer, came to the Department of Emergency with severe epigastric discomfort, abdominal pain and vomiting of 3 days' duration. He had a history of diabetes mellitus for 14 years and was using 12 IU of insulin daily. Despite using insulin, his blood glucose level was not strictly controlled, usually ranging from 250 to 300 mg/dL. The latest hemoglobin A1c level checked 6 months earlier was 7.3%. He had also been diagnosed with end-stage renal disease (ESRD) 6 years previously and had hemodialysis three times a week since then.
On clinical examination, he was drowsy with disorientation. His vital signs were within the normal range. Chest and cardiac findings were unremarkable. The abdomen was not distended, and no mass was palpable. Laboratory test results showed a hemoglobin concentration of 10.4 g/dL, a leukocyte count of 6.4×103 g/µL, and a platelet count of 85×103/µL. His serum creatinine was 8.48 mg/dL and urea nitrogen was 45 mg/dL, which had not increased since the previous lab results obtained 1 month earlier. Amylase and lipase were increased up to 848 and 272 U/L, respectively. The serum glucose level was only 38 mg/dL. After immediate intravenous glucose solution infusion, his mental status improved. The rest of his biological examination results were normal.
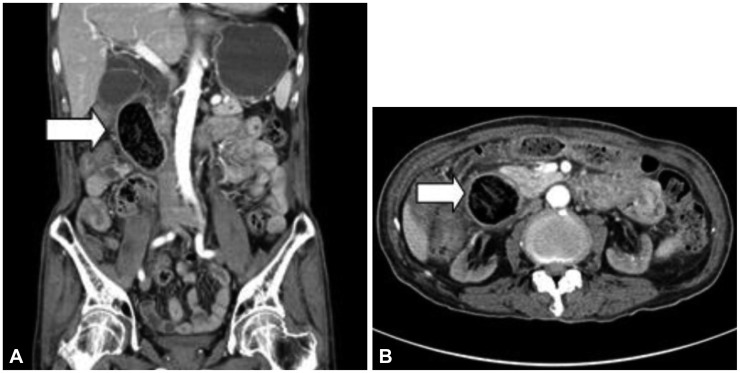
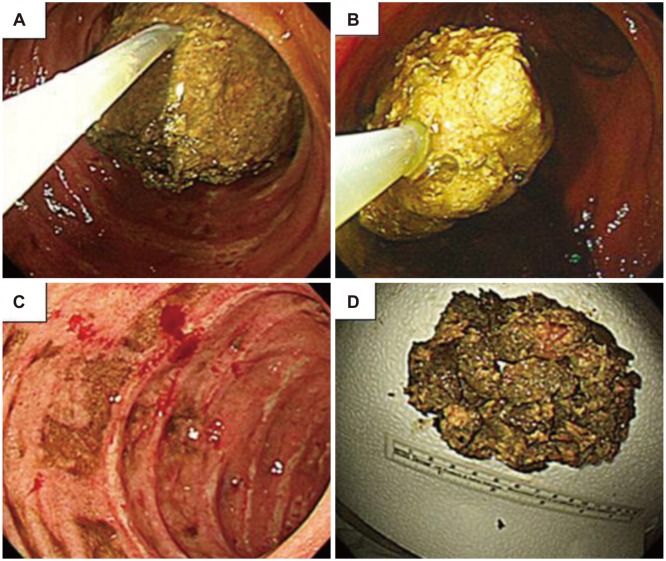
Abdominal radiography showed a normal bowel gas pattern and no significant abnormalities. The patient underwent an abdominal pelvic computed tomography (CT) scan to evaluate the cause of his gastrointestinal symptoms. The CT scan revealed 7×8 cm-sized well-defined duodenal mass including gas bubble inside (Fig. 1). Mild pancreatic duct dilatation was also observed. An esophagogastroduodenoscopy was then performed to obtain accurate diagnosis. The anastomosis site was intact without any stricture; however, directly under the anastomosis site, a huge, dark greenish bezoar was confirmed in the duodenum (Fig. 2). There were also many small ulcers on the periphery of the bezoar. We attempted to pull the bezoar out into the gastric cavity for fragmentation by lithotripsy, which was failed because it was tightly adhering to the lumen of the duodenum. Therefore, we injected 50 mL of Coca-Cola directly to the bezoar in order to reduce its size and soften its consistency. Thirty minutes after the Coca-Cola injection, we attempted to move the bezoar using an alligator forceps (FG-47L-1; Olympus, Tokyo, Japan) and a snare (MTW Endoskopie, Wesel, Germany), which failed again. The patient was admitted to the General Ward from the Emergency Room for further treatment. Three nasogastric lavages were performed using 1.5 L of Coca-Cola every 12 hours with a proton pump inhibitor injection and glucose control by insulin. The next endoscopy demonstrated that the bezoar had become smaller and softer. It could finally be pulled out into the gastric cavity using an alligator forceps and was broken into small pieces by lithotripsy (Lithotriptor handle; Medi-globe, Hachenmuhle, Germany) (Fig. 3A, B). The fragmented pieces were successfully removed using a snare and a basket (MTW Endoskopie). Inspection demonstrated that the removed bezoar was a phytobezoar (Fig. 3D).
Abdominal radiography performed just after the complete endoscopic removal showed no evidence of bowel obstruction. With appropriate intravenous nutritional support using insulin, the patient's serum glucose level was maintained within the normal range. Three days after the complete endoscopic removal, the patient was examined again through second-look endoscopy. No residual bezoar was seen, although small ulcers caused by local pressure on the duodenal wall were observed (Fig. 3C). The patient was discharged with instructions to maintain sufficiently soft diet. Since his discharge, he has had no subsequent episode of abdominal pain or vomiting. On follow-up endoscopy performed 3 months later, no recurrence of a bezoar was noted and his ulcers were completely healed (Fig. 4).
Go to : 
Bezoars grow due to the ingestion and accumulation of undigested material. Bezoars can be classified into four types based on their components: phytobezoars caused by vegetable and fruit fiber; trichobezoars caused by hair; lactobezoars caused by milk curd and others caused by medications, tissue paper, tar, sand, fungus, etc.4 Phytobezoars are currently the most common type of bezoars, and our patient was also diagnosed as having a phytobezoar located in the duodenum after having undergone gastroduodenostomy. The patient did not follow diabetic diet or dialysis diet and usually had lots of fruits including persimmon.
Bezoars may occur in individuals with normal gastrointestinal anatomy and motility; however, patients with altered anatomy and/or motility have a higher risk for bezoar formation. The most common predisposing factor for the formation of bezoar is previous gastric surgery. Vagotomy with pyloroplasty is the surgery type which showed the highest incidence of bezoar, ranging from 65% to 80%, whereas only 20% of those patients who had antrectomy developed bezoars.5 Diabetes mellitus is one of the most common comorbidities with bezoar formation. Diabetic patients develop degenerative neuropathy which impairs their interdigestive migrating motor complex and thus causing delayed gastric emptying and food stasis.6 ESRD requiring dialysis is also an important cause of bezoar formation.5,7 Even though most bezoars are located in the stomach, they can be found anywhere in the gastrointestinal tract. Small intestinal obstruction usually occurs due to the migration of a gastric bezoar, although bezoars formed primarily in the small bowel can also be an obstructive cause.8 Bezoars may rarely extend through the pylorus into the small intestine forming a tail, which is known as Rapunzel syndrome. Duodenal bezoar, such as found in our patient, is a very rare disease and one study showed that superior mesenteric syndrome can also be a cause of duodenal bezoar.9 In the present case, our patient had a history of gastric surgery, diabetes and ESRD. With these risk factors, a large-sized bezoar could be found in the rare site of the gastrointestinal tract in our patient.
The gold standard diagnostic procedure for bezoar detection is gastrointestinal endoscopy, which can provide direct visualization and therapeutic intervention. Other helpful diagnostic methods include abdominal radiography with or without barium, abdominal ultrasound, and CT scanning, where bezoars may be seen as a mass of a filling defect. In a fragmented, bezoar colescense-related intestinal obstruction, serial abdominal radiographies showing a calcified lesion offer useful information.4 In our case, the first diagnosis was performed by abdominal pelvic CT scanning.
Bezoars need to be removed because, if left untreated, they are related to significant morbidity and high mortality rates up to 30%.2 Some small phytobezoars are treated conservatively with nasogastric lavage; however, endoscopic fragmentation is the treatment of choice for most gastroduodenal bezoars. Various endoscopic methods and instruments have been reported, including biopsy forceps, lithotripsy with a basket, polypectomy snare, and argon plasma beam.3 Some recent studies have reported that Coca-Cola infusion directly to a bezoar or nasogastric lavage with Coca-Cola make bezoars soften and shrink. After using Coca-Cola, endoscopic fragmentation can be easily performed.10 Many patients can be successfully treated using an endoscopic procedure and conservative management; however, in patients with gastric outlet obstruction, early surgery is required because they rarely improve with conservative management.2 After endoscopic or surgical treatment, patients are recommended to avoid a high-fiber diet or foods such as persimmon. In our patient, surgery was indicated as near total duodenal obstruction occurred. However, the patient's condition was not appropriate for surgery due to his underlying diseases and general health condition. Therefore, we attempted to treat him using nonsurgical procedures such as endoscopic treatment and Coca-Cola infusion.
In conclusion, the bezoar described here is unusual because of its location and size. Reports of bezoars located in the duodenum are very rare, and our patient was asymptomatic until the bezoar had grown to a relatively large size. Thus, huge bezoars in the duodenum can be successfully treated by endoscopic-guided fragmentation assisted by Coca-Cola infusion.
Go to : 
References
1. McKechnie JC. Gastroscopic removal of a phytobezoar. Gastroenterology. 1972; 62:1047–1051. PMID: 5029071.

2. Singh SK, Marupaka SK. Duodenal date seed bezoar: a very unusual cause of partial gastric outlet obstruction. Australas Radiol. 2007; 51 Spec No.:B126–B129. PMID: 17875133.

3. Lee BJ, Park JJ, Chun HJ, et al. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol. 2009; 15:2265–2269. PMID: 19437568.

4. Chen HW, Chu HC. Migration of gastric bezoars leading to secondary ileus. Intern Med. 2011; 50:1993–1995. PMID: 21921383.

5. Feldman M, Friedman L, Sleisenger MH, Fordtran JS. Sleisenger & Fordtran's Gastrointestinal and Liver Disease. 7th ed. London: W.B. Saunders;2002. p. 395–398.
6. Pinto D, Carrodeguas L, Soto F, et al. Gastric bezoar after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2006; 16:365–368. PMID: 16545170.

7. Sanders MK. Bezoars: from mystical charms to medical and nutritional management. Pract Gastroenterol. 2004; 28:37–50.
8. Chung YW, Han DS, Park YK, et al. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006; 38:515–517. PMID: 16330268.

9. Fuhrman MA, Felig DM, Tanchel ME. Superior mesenteric artery syndrome with obstructing duodenal bezoar. Gastrointest Endosc. 2003; 57:387. PMID: 12612525.

10. Matsushita M, Fukui T, Uchida K, Nishio A, Okazaki K. Effective "Coca-Cola" therapy for phytobezoars. Intern Med. 2008; 47:1161. PMID: 18552481.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download