Abstract
Brunner's gland adenoma is a rare benign proliferative lesion developing most commonly in the posterior wall of the duodenum. It is usually small in size and asymptomatic. Depending on its size or location, however, the clinical manifestations of this tumor may be variable from nonspecific symptoms to gastrointestinal bleeding or obstruction. Brunner's gland adenoma in the proximal jejunum is extremely rare. We report a very rare case of giant Brunner's gland adenoma developing in the proximal jejunum which presented as iron deficiency anemia and mimicked intussusceptions on radiologic studies.
Brunner's glands are submucosal glands found in the first portion of the duodenum and in decreased numbers in the distal duodenum. In children, the glands also may present in the proximal jejunum.1 Brunner's gland adenoma is a rare benign proliferative lesion developing most commonly in the posterior wall of the duodenum near the junction of the first and second portions. It is usually asymptomatic. Depending on its size or location, however, the clinical manifestations of this tumor may be variable from nonspecific symptoms to gastrointestinal bleeding or obstruction.2,3 Brunner's gland adenoma in the proximal jejunum is extremely rare. We report a case of giant Brunner's gland adenoma of the proximal jejunum which presented as iron deficiency anemia (IDA) and mimicked intussusceptions on radiologic studies.
A 50-year-old woman presented with abdominal discomfort and general weakness lasting for 2 months. She visited a private clinic and anemia has been detected in her blood tests. She was referred to our hospital for further evaluation of IDA. She had no other medical problems. The physical examination revealed no abdominal tenderness, rebound tenderness, or palpable mass. Her complete blood counts were as follows; hemoglobin 6.3 g/dL, hematocrit 19.2% (mean corpuscular volume 91.4 fL, mean corpuscular hemoglobin 29.9 pg), and platelet 366,000/mm3. The levels of iron and ferritin were 7 µg/dL (normal value, 50 to 130) and 7.5 ng/mL (normal value, 10 to 291), respectively. Liver function tests were within normal limits. Stool occult blood test was negative, and esophagogastroduodenoscopy and colonoscopy revealed no obvious cause of IDA. For the next diagnostic evaluation, abdominal computed tomography (CT) and small bowel follow-through were performed and intussusceptions in the proximal jejunum were suspected (Figs. 1, 2). However, she had no apparent symptoms pertaining to intussusceptions. We performed a double balloon enteroscopy (DBE) for direct inspection of the proximal jejunum and differential diagnosis between intussusception and an intraluminal mass. A polypoid mass with a very long and wide stalk arising from the proximal jejunum was detected. The lesion was more than 9 cm in length, with soft consistency and normal appearing mucosa (Fig. 3). We changed the double balloon enteroscope to push enteroscopy using colonoscope for endoscopic treatment using Endo-Loop (Ethicon, Sommerville, NJ, USA). We first ligated the mid part of stalk for prevention of immediate bleeding using Endo-Loop and then removed the polypoid mass using snare polypectomy. The resected polypoid mass was histologically confirmed a giant Brunner's gland adenoma (Fig. 4). Her hemoglobin was normalized (12.1 g/dL) 3 months after the endoscopic treatment.
Brunner's gland adenoma (also referred to as Brunneroma or Brunner's gland hamartoma) is a rare benign tumor of the duodenum. Cruveilhier4 reported the first case in 1835, describing a Brunner's adenoma causing intussusceptions with lethal outcomes. Brunner's glands are branched and acinotubular structures located in the submucosa and deeper parts of the duodenal wall. The function of Brunner's glands is to secrete alkaline mucoid fluid, which contains glycoproteins forming an adherent layer on the duodenal mucosa, protecting it from the acid chyme of the stomach. In addition, Brunner's glands produce urogastrone, an inhibitor of gastric acid secretion.5,6
Feyrter7 defined three types of Brunner's gland hyperplasia; diffuse nodular hyperplasia, occupying most of the duodenum; circumscribed nodular hyperplasia, the most common type mainly present in the duodenal bulb; and adenomatous hyperplasia (also known as Brunner's gland hamartoma or adenoma), which generally present as a single polypoid lesion. Hyperplasia refers to multiple lesions (usually less than 1 cm) and adenoma refers to lesion larger than 1 cm.7 One that contains mixture of muscular and fatty elements is called hamartoma. Brunner's gland adenomas are mostly benign but malignant transformation has been reported in two cases.8,9 Our case was confirmed as a 9-cm long adenoma, showing no malignant transformation.
Brunner's gland adenoma is usually asymptomatic and detected incidentally. However, the clinical manifestations may be variable depending on its size, type or location. It can cause upper gastrointestinal hemorrhage from ulcer or erosion over the surface of a polyp, biliary obstruction, pancreatitis, or gastric outlet obstruction.2,10 Our patient presented with abdominal discomfort with IDA of unknown origin.
Useful diagnostic tools of Brunner's gland adenoma are barium contrast studies, abdominal CT and endoscopy. Large adenomas may be detected by ultrasonography. Upper gastrointestinal barium studies may reveal multiple small filling defects ('Swiss cheese' appearance) in the cases of Brunner's gland hyperplasia, adenomas, or smooth surfaced polypoid lesions.11 Since Brunner's gland adenomas are most commonly located in duodenal bulb, gastroduodenoscopy is usually helpful for clinical and histological diagnosis. Because it is mainly located in the submucosal layers, however, biopsies often show negative findings with slight changes of inflammation.12
In this patient, we performed a small bowel follow-through and CT for further evaluation of IDA, which suggested intussusceptions in the proximal jejunum. Then we performed DBE because it appeared impossible to reach the lesion using a conventional endoscope. An elongated mass covered with normal looking mucosa was detected in the proximal jejunum. For accurate diagnosis and treatment, we resected the tumor using the push enteroscopy with colonoscope. Push enteroscopy with conventional colonoscope is sometimes very useful for lesions located in the proximal jejunum because it is easier than DBE to handle the scope and to apply various therapeutic devices like Endo-Loop.
Treatment of Brunner's gland adenoma may be conservative as long as it remains asymptomatic. Brunner's gland adenoma has been considered as a benign disorder. Although it is rare, however, malignant transformation was also reported in the literatures.8,9 Surgical or endoscopic resection is indicated for patients with symptoms or signs. Endoscopic resection of Brunner's gland adenoma is less invasive and more cost effective than laparoscopic surgery. Hemoclip assisted polypectomy can be useful for large Brunner's gland adenomas with stalks.13 In our case of a giant Brunner's gland adenoma with a long stalk, we successfully removed the tumor with a snare polypectomy using detachable snare through DBE.
In conclusion, we report a very rare case of giant Brunner's gland adenoma in the proximal jejunum which presented as IDA and mimicked intussusceptions on the radiological studies.
References
1. Sleisenger MH, Feldman M, Friedman LS, Brandt LJ. Sleisenger & Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 2006. 8th ed. Philadelphia: Saunders.
2. Hirasaki S, Kubo M, Inoue A, Miyake Y, Oshiro H. Pedunculated Brunner's gland hamartoma of the duodenum causing upper gastrointestinal hemorrhage. World J Gastroenterol. 2009; 15:373–375. PMID: 19140240.

3. El Faleh I, Lutz N, Osterheld MC, Reinberg O, Nydegger A. Gastric outlet obstruction by Brunner's gland hyperplasia in an 8-year-old child. J Pediatr Surg. 2009; 44:E21–E24. PMID: 19361619.

4. Cruveilhier J. Anatomie Pathologique du Corps Humain. 1835. Paris: Bailliere.
5. Krause WJ, Stevens R, Palmiter P. The effect of surgical ablation of Brunner's glands on the proximal duodenal mucosa. Anat Anz. 1988; 166:111–115. PMID: 3189825.
6. Stolte M, Schwabe H, Prestele H. Relationship between diseases of the pancreas and hyperplasia of Brunner's glands. Virchows Arch A Pathol Anat Histol. 1981; 394:75–87. PMID: 7336574.

7. Feyrter F. Über wucherungen der brunnerschen drüsen. Virchows Arch Pathol Anat Physiol Klin Med. 1934; 293:509–526.

8. Christie AC. Duodenal carcinoma with neoplastic transformation of the underlying Brunner's glands. Br J Cancer. 1953; 7:65–67. PMID: 13051506.

9. Fujimaki E, Nakamura S, Sugai T, Takeda Y. Brunner's gland adenoma with a focus of p53-positive atypical glands. J Gastroenterol. 2000; 35:155–158. PMID: 10680672.

10. Mayoral W, Salcedo JA, Montgomery E, Al-Kawas FH. Biliary obstruction and pancreatitis caused by Brunner's gland hyperplasia of the ampulla of Vater: a case report and review of the literature. Endoscopy. 2000; 32:998–1001. PMID: 11147953.

11. Henken EM, Forouhar F. Hamartoma of Brunner's gland causing partial obstruction of the ileum. J Can Assoc Radiol. 1983; 34:73–74. PMID: 6841428.
12. Palanivelu C, Rangarajan M, Jategaonkar PA, Annapoorni S, Prasad H. Laparoscopic antrectomy for a proximal duodenal Brunner gland hamartoma. JSLS. 2009; 13:110–115. PMID: 19366555.
13. Chen YY, Su WW, Soon MS, Yen HH. Hemoclip-assisted polypectomy of large duodenal Brunner's gland hamartoma. Dig Dis Sci. 2006; 51:1670–1672. PMID: 16927147.

Fig. 1
Abdominal computed tomography images. (A) Axial image shows suspected intussusception or intraluminal tumor less likely in the proximal jejunum. (B) Coronal reconstruction image also shows suspected intussusceptions or an elongated intraluminal mass with soft tissue attenuation.
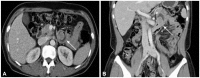
Fig. 2
Small bowel follow-through. It shows a segmental dilatation with the contrast filled along the inner wall of the lumen in the proximal jejunum, which suggests suspected intussusceptions rather than an intraluminal mass as considered with computed tomography findings.
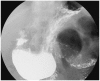
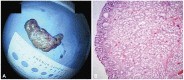
Fig. 3
Enteroscopic findings. (A) It shows a huge intraluminal mass with normal appearing mucosa in the proximal jejunum through double balloon enteroscopy. (B) It has a long stalk and wide base. (C) This tumor is resected by snare polypectomy after snaring Endo-loop through push enteroscopy. (D) After polypectomy, Endo-loop has been left at the base of stalk with no bleeding.

Fig. 4
Pathologic findings. (A) Gross finding right after the endoscopic resection. It shows a giant polypoid mass, 9×2 cm in size. (B) Microscopic finding showing the lobules forming the tumor composed of normal appearing Brunner's gland without unusual mixture of normal tissues including Brunners glands, ducts, adipose tissue, and lymphoid tissue (H&E stain, ×40).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download