Abstract
Self expandable metal stent can be used both as palliative treatment for malignant colorectal obstruction and as a bridge to surgery in patients with potentially resectable colorectal cancer. Here, we report a case of successful relief of malignant stomal obstruction using a metal stent. A 56-year-old man underwent loop ileostomy and was given palliative chemotherapy for ascending colon cancer with peritoneal carcinomatosis. Eight months after the surgery, he complained of abdominal pain and decreased fecal output. Computed tomography and endoscopy revealed malignant stomal obstruction. Due to his poor clinical condition, we inserted the stent at the stomal orifice, instead of additional surgery, and his obstructive symptoms were successfully relieved. Stent insertion is thought to be a good alternative treatment for malignant stomal obstruction, instead of surgery.
Malignant colonic obstruction is managed by endoscopic colon stent insertion, removal of obstructive lesion followed by reconnecting sections of the large intestine, or creation of a diverting colostomy/ileostomy. Surgery for stoma correction has also been used for malignant stomal obstruction.1 However, surgery might increase mortality and morbidity in patients with advanced cancer or poor performance status; as a result, there has been no established strategy for the management of malignant stomal obstruction.2 In such cases, stent insertion might be a reasonable alternative. We report a case of successful relief of malignant stomal obstruction using a metal stent and a review of the literature.
A 56-year-old man presented with right lower quadrant pain and abdominal distention for 2 months. Colonoscopy showed an ulcerofungating mass lesion in the ascending colon and the scope could not be passed through it. Abdominal computed tomography (CT) showed asymmetric enhancing wall thickening in the right side colon and multiple lymph node enlargements in the right side mesentery and mesenteric root. In addition, ascites were observed in the pelvis. He was diagnosed as ascending colon cancer with peritoneal carcinomatosis (stage IVb). He was initially treated by inserting self expandable metallic stent (SEMS) for colonic obstruction. Two days after the stent insertion, abdominal distention and pain were re-developed and follow-up CT showed near total obstruction at the proximal portion of the stent, suggesting stent migration. Thus, he underwent loop ileostomy and palliative chemotherapy was started after the operation.
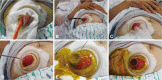
After 12 cycles of chemotherapy with oxaliplatin, 5-fluorouracil and leucovorin, disease progression was noted and the patient developed abdominal pain with decreased stool output. Physical examination showed mildly distended abdomen with decreased bowel sounds. On palpation, there was tenderness over the peristomal region. Abdominal CT scan showed a peritoneal metastasis surrounding the stoma and diffuse dilatation of the small bowel (Fig. 1). Because a conventional colonoscope could not be passed through the stoma, we used Olympus scope GIF-XQ 260 (9.8 mm diameter; Olympus, Tokyo, Japan). Endoscopy showed obstruction of the ileostomy site by a mass (Fig. 2). The lesion was hard and it had some ulcers covered with exudates, compatible with stomal obstruction arising from carcinomatosis. Based on the patient's poor condition, surgery for stoma correction deemed inappropriate due to high risk of complication. Therefore, after the informed consent was obtained, a 60 mm length, 24 mm diameter self expandable metal stent (Niti-S colonic non TTS uncovered stent; Taewoong Medical Inc., Seoul, Korea) was implanted in the stoma under fluoroscopic guidance (Figs. 3, 4). Upon release of the stent, fecal materials poured through the stent. An anchoring suture was performed in order to prevent migration of the stent. One week later, he was discharged without a complaint of bowel obstruction, but he died one and half months after the stent placement due to the progression of the colon cancer, without clinical signs of re-obstruction.
Malignant colon obstruction is common in patients with advanced cancer, usually colorectal cancer. Acute colorectal obstruction usually requires rapid bowel decompression, such as emergency surgery, which is associated with relatively high mortality and morbidity rates. Recently introduced SEMS, however, can be used both as a palliative treatment for unresectable malignant colorectal obstruction and as a bridge to surgery in patients with potentially resectable colorectal cancer. In the bridge to surgery setting, insertion of SEMS can decompress the obstruction, provide the opportunity for bowel preparation, and make one-stage surgical resection possible, which is known to be associated with decreased morbidity, mortality, and stoma formation rate compared with emergency surgery.3-6
Adenocarcinoma may develop at a colostomy or ileostomy site as a primary tumor, a metachronous lesion, or a carcinomatosis and disseminated disease.7-9 Malignant stomal obstruction has traditionally been treated with surgery, and specific surgery has been selected based on the clinical characteristics of each patient. For example, a patient with advanced cancer could be considered as a candidate for a limited local resection, while a patient with an isolated stoma recurrence as a candidate for a broad local resection, including the abdominal wall.10 However, there is no appropriate alternative management established yet for cases where the limited local resection is technically difficult or where there is a risk of increasing the rate of resection-related complication due to the patient's poor performance status. In these settings, stent insertion might be a good therapeutic option instead of palliative surgery in malignant stomal obstruction, considering the poor prognosis and high mortality and morbidity rate of palliative surgery.
When life expectancy is short, stent migration is thought to be the more serious complication than stent re-obstruction. Therefore, to prevent stent migration, the uncovered stent was more favorable than covered stent in our patient, and anchoring suture in the distal portion of the stent, such as anchoring clips, would be also helpful to prevent the stent migration.11,12
In conclusion, SEMS insertion for malignant stomal obstruction could be an alternative treatment, instead of surgery, in patients with inoperable colon cancer or poor performance status. Further research is needed to determine the validity of SEMS in palliating obstructive symptoms compared with operative management in malignant stomal obstruction.
References
1. Colwell J. Colwell J, Goldberg M, Carmel J, editors. Stomal and peristomal complications. Fecal and Urinary Diversions: Management Principles. 2004. St. Louis: Mosby;p. 308–325.
2. De Angelo DJ. Chang AE, Hayes DF, Pass HI, editors. Metabolic emergencies in oncology. Oncology: an Evidence-Based Approach. 2006. 1st ed. New York: Springer-Verlag;p. 1321–1331.

3. Khot UP, Lang AW, Murali K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg. 2002; 89:1096–1102. PMID: 12190673.

4. Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ. Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg. 2007; 246:24–30. PMID: 17592286.
5. Choo IW, Do YS, Suh SW, et al. Malignant colorectal obstruction: treatment with a flexible covered stent. Radiology. 1998; 206:415–421. PMID: 9457194.

6. Law WL, Chu KW, Ho JW, Tung HM, Law SY, Chu KM. Self-expanding metallic stent in the treatment of colonic obstruction caused by advanced malignancies. Dis Colon Rectum. 2000; 43:1522–1527. PMID: 11089586.

7. Shellito PC. Complications of abdominal stoma surgery. Dis Colon Rectum. 1998; 41:1562–1572. PMID: 9860339.

8. Roberts PL, Veidenheimer MC, Cassidy S, Silverman ML. Adenocarcinoma arising in an ileostomy: report of two cases and review of the literature. Arch Surg. 1989; 124:497–499. PMID: 2539068.
9. Carey PD, Suvarna SK, Baloch KG, Guillou PJ, Monson JR. Primary adenocarcinoma in an ileostomy: a late complication of surgery for ulcerative colitis. Surgery. 1993; 113:712–715. PMID: 8506531.
10. Orkin BA, Araghizadeh F. Billingham RP, Kobashi KC, Peters WA, editors. Reoperative surgery for gastrointestinal stomal problems. Reoperative Pelvic Surgery. 2009. 1st ed. New York: Springer-Verlag;p. 289–305.

11. Baron TH, Dean PA, Yates MR 3rd, Canon C, Koehler RE. Expandable metal stents for the treatment of colonic obstruction: techniques and outcomes. Gastrointest Endosc. 1998; 47:277–286. PMID: 9540883.

12. Kim ID, Kang DH, Choi CW, et al. Prevention of covered enteral stent migration in patients with malignant gastric outlet obstruction: a pilot study of anchoring with endoscopic clips. Scand J Gastroenterol. 2010; 45:100–105. PMID: 20030581.

Fig. 1
Computed tomography of the abdomen showed abdominal wall metastasis. Enhancing mass around the ileostomy site resulted in diffuse dilatation of the small bowel.
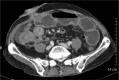
Fig. 2
(A) Conventional endoscopy showed obstruction of the stoma by cancer invasion. (B) The lesion was felt to be hard on palpation and it had shallow, irregular marginated ulcers covered with exudates.
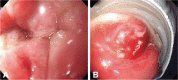
Fig. 3
(A) After removing the rectal tube, (B, C) we inserted a guide wire through the obstructive lumen under endoscopy and fluoroscopic guidance. (D) Then, self expandable metallic stent was inserted over the guide wire. (E, F) The last two pictures showed the fully expanding percutaneous metal stent and fecal materials pouring from the stent's lumen.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download