Abstract
Background/Aims
Patients undergoing Billroth II (B II) gastrectomy are at higher risk of perforation during endoscopic retrograde cholangiopancreatography (ERCP). We assessed the success rate and safety of forward-viewing endoscopic biliary intervention in patients with B II gastrectomy.
Methods
A total of 2,280 ERCP procedures were performed in our institution between October 2008 and June 2011. Of these, forward-viewing endoscopic biliary intervention was performed in 46 patients (38 men and 8 women with B II gastrectomy). Wire-guided selective cannulations of the common bile duct using a standard catheter and guide wire were performed in all patients.
Results
The success rate of afferent loop entrance was 42 out of 46 patients (91.3%) and of biliary cannulation after the approach of the papilla was 42 out of 42 patients (100%). No serious complications were encountered, except for one case of small perforation due to endoscopic sphincterotomy site injury.
Conclusions
When a biliary endoscopist has less experience and patient volume is low, ERCP with a forward-viewing endoscope is preferred because of its ease and safety in all patients with prior B II gastrectomies. Also, forward-viewing endoscope can be used to improve the success rate of biliary intervention in B II patients.
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II (B II) gastrectomy poses a special challenge to the beginners in ERCP because diagnostic and therapeutic ERCPs are rated grade 2 and 3, respectively, based on the ERCP procedure difficulty scale.1 The altered anatomy causes technical difficulties in afferent loop intubation and selective cannulation of the bile duct, thus hampering the procedure and resulting in a lower success rate of biliary cannulation and a higher incidence of complications compared to patients with normal anatomy.2,3 Most expert endoscopists recommend using a duodenoscope since it has an elevator and large accessory channel, and the endoscopic manipulation of B II ERCP is not different from that of normal anatomy.4 However, we recommend the forward-viewing gastroscope for endoscopists inexperienced with ERCP because the lack of an elevator is only a slight disadvantage, and if the endoscope reaches the papilla, selective bile duct cannulation is possible because the endoscope and the catheter are in line with the common bile duct (CBD).5 Here, we present our technique and experiences of 46 cases of ERCP in patients with B II.
A total of 2,280 ERCP procedures were performed at our institution from October 2008 to June 2011. Patients were excluded from the analysis if they had undergone endoscopic sphincterotomy (EST) previously or if the anatomy of the papilla was normal despite having undergone B II. One endoscopist performed all procedures, and written informed consent was obtained from all patients. This study was approved by the Institutional Review Board of Yonsei University Wonju College of Medicine.
Routine endoscopic examination was first performed to identify the opening of the afferent loop and papilla in most patients except for those experiencing an emergent situation such as severe cholangitis. We divided our patients into two categories according to B II reconstruction;6 isoperistaltic type, which has the afferent limb along the greater curvature, and antiperistaltic type, which has the afferent limb connected to the lesser curvature. ERCP with forward viewing gastroscope was performed under fluoroscopic guidance. ERCP procedures were performed under conscious sedation with midazolam or propofol and pethidine. The patients were placed in the prone position and their blood pressure, heart rate, and pulse oximetry were monitored. Antibiotics were routinely given as prophylaxis. All endoscopic procedures were carried out with a forward-viewing endoscope (Olympus GIF-Q260; Olympus Optical, Tokyo, Japan).
The afferent loop was intubated with minimal air insufflation. Most papillae were situated at the 10 or 11-o'clock position. When the endoscope reached the papilla, the papilla was turned to face the endoscope and then the tip of the catheter was properly located to access the CBD at the 4 to 5 o'clock position. After minimal insertion (2 to 3 mm) of the catheter in the ampulla, the guidewire was carefully advanced through the CBD under fluoroscopy until it was seen to enter the bile duct. Pushing the catheter against the duodenal wall at the 9 to 10 o'clock position or bending the tip of the endoscope led the tip of the catheter to the correct access to the CBD (Fig. 1).7 This wire-guided selective cannulation of the CBD was achieved using a standard catheter (Triple Lumen ERCP cannula, Tapered Tip, 5.5 F; Boston Scientific, Natick, MA, USA) and guide wires. We used either Tracer hybrid (Wilson-Cook Medical, Winston-Salem, NC, USA) or Jagwire (Boston Scientific) 0.035-inch hydrophilic guide wires.
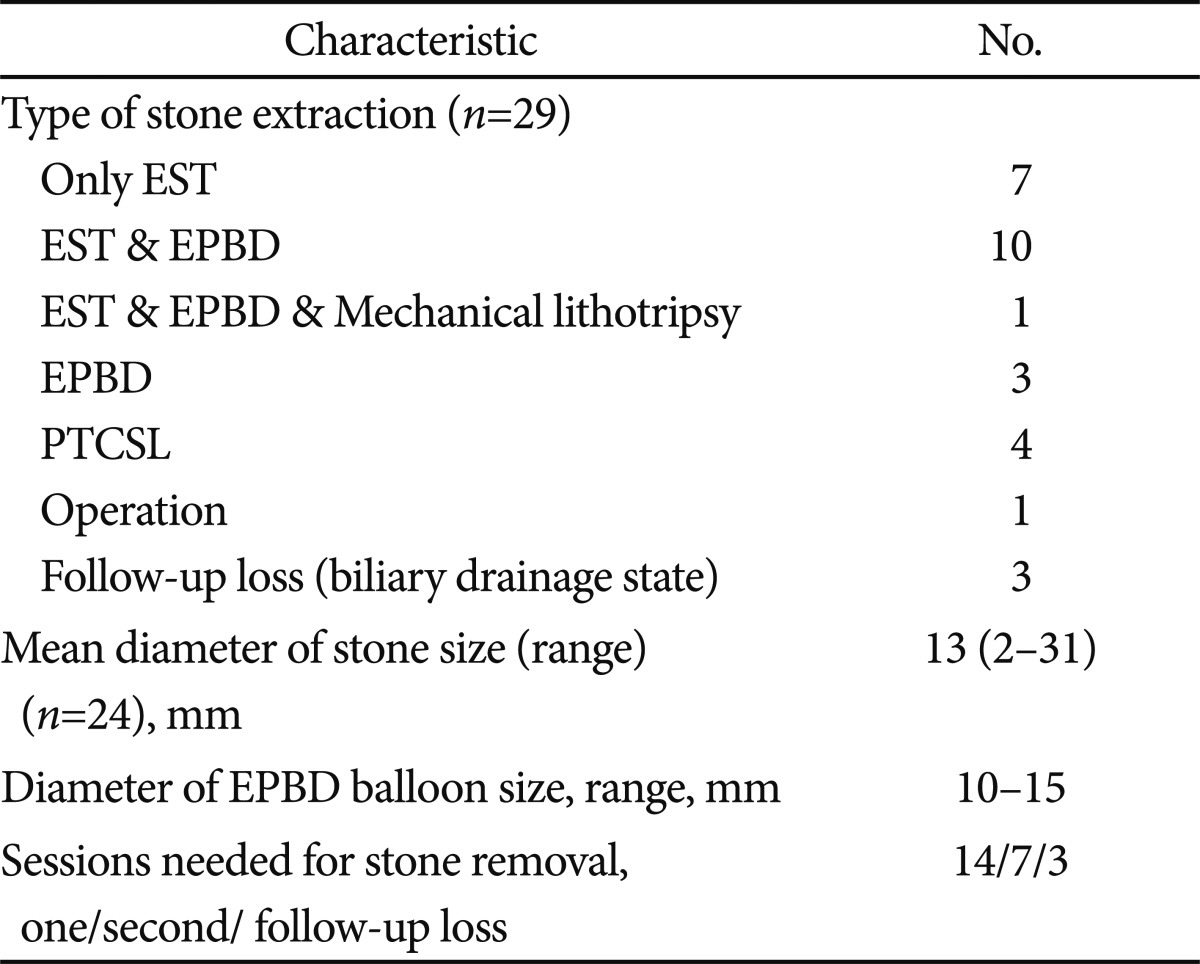
The procedure time of selective biliary cannulation was defined as the time between reaching the papilla and securing the guidewire on the CBD. The time to reaching the papilla was not analyzed, however, because the intubation of the afferent loop was easily performed in most cases. EST was performed using a Sohendra B II sphincterotome (Double Lumen Wire Guided; Wilson-Cook Medical) or rotatable sphincterotome (Autotome Rx cannulating sphincterotome, 4.4 F; Boston Scientific) (Fig. 2). If these techniques failed to achieve selective biliary cannulation, needle-knife fistulotomy was performed on the inverted roof of the papilla with a needle knife papillotome (Microtome; Boston Scientific) (Fig. 3). After biliary cannulation was successfully performed, a controlled radial expansion balloon dilation catheter (7.5 Fr to 5.5 cm length of balloon; Boston Scientific) was used for endoscopic papillary balloon dilatation (EPBD) in patients with CBD stones (Fig. 2). The balloon dilatation catheter was placed across the papilla, and the balloon was inflated slowly with dilute contrast medium until the waistline was obliterated under fluoroscopic monitoring. An extraction balloon (Retrieval Balloon Catheter 12/15 mm, 7 F; Boston Scientific or Extraction Balloon Catheter, 15 mm; Wilson-Cook Medical) or lithotripsy basket (four-wire, StoneBuster Basket; Medi-Globe, Achenmühle, Germany) was used for retrieval of biliary stones after papillary dilation. If complete stone removal was not achieved in one session, biliary drainage was performed, such as endoscopic retrograde biliary drainage (Biliary Drainage Stent 7 Fr, 10 cm; Boston Scientific), and the stones were removed during an additional session. The sizes of stones were evaluated on cholangiograms taken during the initial bile duct filling phase and after optimal opacification.
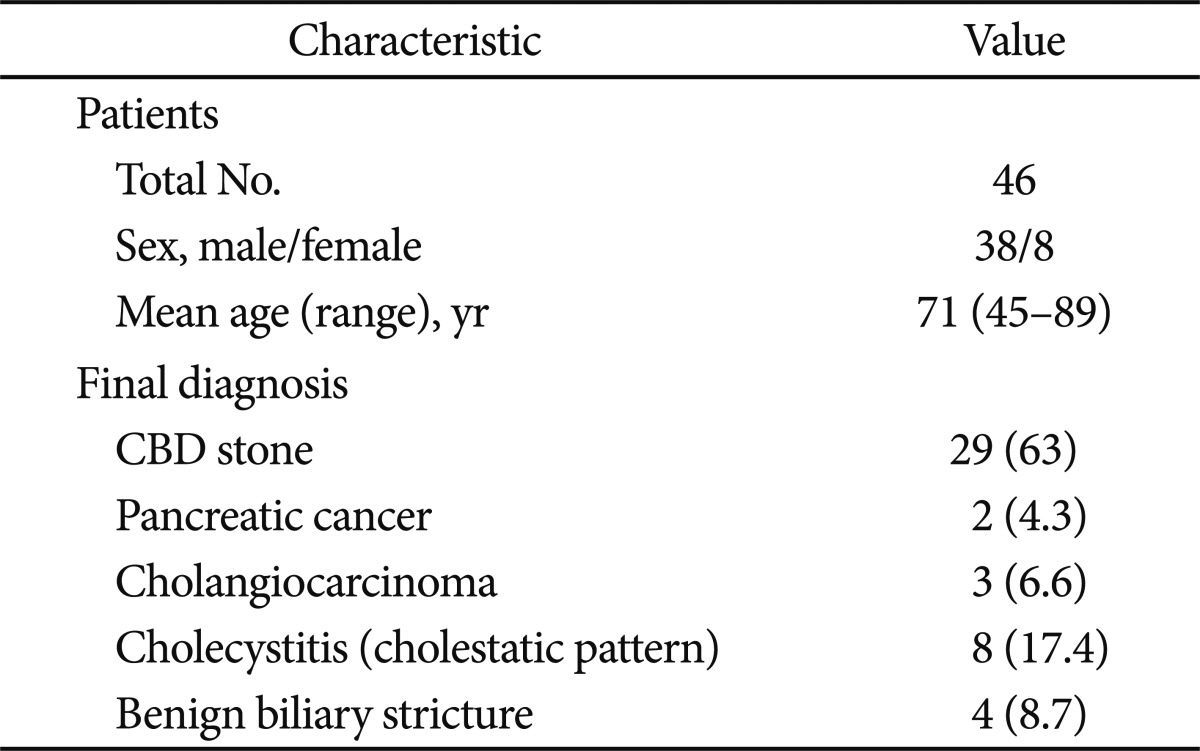
A total of 57 forward-viewing endoscopic biliary cannulations were performed in 46 patients (38 men and 8 women with B II gastrectomy) by one endoscopist. The mean age was 71 years (range, 45 to 89). Patients who underwent B II reconstruction included 34 patients with isoperistaltic, eight patients with antiperistaltic, and four patients with unknown types. There was no case of Braun's anastomosis in our successful 42 cases except for the four failed cases which were not ascertained. The indications for ERCP were obstructive jaundice because of stones (n=29), cancer (n=5), elevated liver enzymes due to cholecystitis (n=8) and benign biliary strictures (n=4) (Table 1). The overall success rates of reaching the papilla and selective cannulation of the bile duct was 42 of 46 (91.3%) and 42 of 42 patients (100%), respectively. The first attempts of biliary cannulation were not successful in two patients, but the second attempts after medical therapy in these patients were successful. The procedures performed in our series were mostly stone removal (n=29), and the others included plastic biliary stent insertion due to cancer such as pancreatic cancer, bile duct cancer, and metastatic lymphadenopathy or benign biliary stricture such as chronic pancreatitis or Mirizzi syndrome (n=6), diagnostic approach for liver enzyme elevation such as cholecystitis or cholangitis (n=10), and metal stent insertion due to Klastkin's tumor (n=1) (Table 2).
ERCP using a forward-viewing endoscope was unsuccessful in 4 patients. The failures to reach the papilla were due to a long afferent loop (n=1) or incapability to achieve afferent loop intubation because of sharp angulation (n=3). Of the four failed patients, one patient underwent surgery to treat CBD and intrahepatic bile duct stones, and the other three patients underwent percutaneous transhepatic choledochoscopic lithotripsy (PTCSL). One patient with a successful cannulation underwent PTCSL because he had a sharp angulation and stricture due to CBD stones (Fig. 4). EST and needle knife fistulotomy were successful in 35 of 42 (76%) and 11 of 42 (24%) patients, respectively. The mean time to selective biliary cannulation after reaching the ampulla of Vater was 6.54 (range, 1.27 to 24.04) minutes in successful patients. Thirty-six patients, except for six patients with longer procedure time, were successfully cannulated in less than 10 minutes (Table 2). The mean diameter of the CBD stone size was 13 (range, 2 to 31) mm in our cases. Complete stone removal in a single endoscopic session was achieved in 14 of 29 patients and in two sessions in seven of 29 patients. In the other eight patients, stone removal was performed in non-endoscopic method, such as PTCS or operation, of five patients and follow-up loss occurred in three patients. Except for the three patients who were lost to follow-up, stones were removed in the following manners: EST only in 11 patients, both EST and EPBD in eight patients, EST and EPBD including emergent lithotripsy in one patient, EPBD only in one patient, PTCS in four patients and operation in one patient. Emergent lithotripsy was used only in one patient due to insufficient EPBD balloon size (Table 3). Only one patient with CBD stones suffered mild pancreatitis after dye injection into the pancreatic duct, and recovered after a pancreatic stent was inserted as a rescue therapy. There was a perforation in one patient with asymptomatic CBD dilatation due to inadequate direction of catheter insertion and subsequent injury. This patient recovered after conservative medical therapy. One patient with a Klatskin's tumor suffered acute cholecystitis after a metal stent was inserted in the CBD. This patient recovered after performing percutaneous transhepatic gallbladder drainage. There were no deaths related to the procedures in any patients (Table 2).
ERCP in patients with B II places a large burden on inexperienced biliary endoscopists. For expert endoscopists, the procedure has the same level of difficulty as in a patient with normal anatomy, so they usually recommend using a side-viewing duodenoscope because the endoscope has an elevator and large accessory channel.8,9 Of course, the skill of the experienced endoscopist is an important factor in the safety of the procedure and complication rates for diagnostic or therapeutic ERCP.3,8,10-12
We initially used a forward-viewing endoscope in all of our cases, because perforations may occur when the straightening maneuver is performed with a duodenoscope within the afferent loop while trying to reach the papillary area. Some studies have suggested using a forward-viewing endoscope to prevent perforation.13,14 Our success rate of reaching the papilla was 91.3%, and that of selective cannulation of the bile duct was 100%.
Although there is a general belief that a more en face view can be obtained by a duodenoscope and that the power of the elevator is necessary,15 it is easier to cannulate the CBD with a forward-viewing endoscope because the en face position with the papilla is easily achieved, and access to the CBD with a straight catheter is possible using wire-guided selective cannulation method.7,11,16 In some studies, the ERCP with a capfitted forward-viewing endoscope was successful without difficulty in the afferent loop intubation and selective CBD cannulation in patients with a prior B II gastrectomy, even though the forward-viewing endoscope doesn't have an elevator and has small size of working channel.17,18 In our study, we didn't use cap-fitted method, but we think that this method can be useful and will improve our results when our approach has failed in the course of afferent loop intubation and selective CBD cannulation. However, 42 out of 46 cases in our study were successful in the insertion of the afferent loop and selective CBD cannulation, even without the cap-fitted method.
The success rates of selective ductal cannulation and complication rates related to the procedure in B II patients are variable depending on differences in techniques and the experience of the endoscopist who performs the procedure. Hesitant, fearful and half-hearted attempt at cannulation invariably leads to failure of the procedure. We used the wire-guided selective cannulation method in all cases, and the success rate of selective cannulation was 100% including the two cases which succeeded at the second trial. We primarily used needle knife fistulotomy in 11 patients; this procedure is not difficult, because the incision can be made under the en face approach.
A common complication of ERCP in patients with B II is perforation of the small bowel, especially in the afferent loop. The perforation rate is variably reported in the literature, and perforations that require surgery may be disastrous for both patients and endoscopists.8,12,13,19 Thus, experts recommend that ERCP in B II patients must be performed by experienced endoscopists accustomed to this procedure at institutions that are equipped to treat endoscopy-related complications.20 It would be ideal if only experts performed the procedure. However, less experienced endoscopists need to practice the procedure in order for them to become experts in ERCP in B II patients. Therefore, our results for the use of forward-viewing endoscopes in B II patients should encourage beginners that are faced with complicated clinical scenarios, such as severe cholangitis due to huge CBD stones in patients with B II anastomosis. A forward-viewing endoscope should be the first choice modality for an endoscopist who is not accustomed to B II patients. In our cases, only one perforation occurred, and the patient recovered without surgical therapy because the perforation was sphincterotomy induced injury rather than endoscope induced injury.
Despite the development of new techniques and enhancement of experts' experience, some authors question ERCP's role in B II gastrectomy patients because of low success rates, high perforation rates and subsequent deaths. Therefore, other less invasive modalities like PTCSL are often suggested as rescue interventions in patients with B II gastrectomy in whom ERCPs are difficult to perform.21 However, this opinion is contradicted by our high success rate, low perforation rate, and low rescue PTCSL rate using a forward-viewing endoscope. Of course, huge and multiple stone removal is more difficult with a forward-viewing endoscope than with a side-viewing endoscope because of the small channel size. But this difficulty can be overcome by using EPBD, which appears to be an effective and safe treatment for removal of huge bile duct stones in patients who have undergone B-II gastrectomy.15,22,23 In our study, a total of 14 EPBDs were performed, with only one case of pancreatitis, which developed only after EST was performed. Most EPBDs are performed after EST, which may decrease the risk of pancreatitis because the pancreatic orifice is separated from the biliary orifice after EST, and balloon dilation forces away the pancreatic duct.24,25
We highly recommend the use of forward-viewing endoscope when beginner endoscopists are considering to perform ERCP in B II patients. This can decrease endoscopists' fear of complications such as perforation and allow for repeated uncomplicated procedures, which will increase experience in a short amount of time.
References
1. Baron TH, Petersen BT, Mergener K, et al. Quality indicators for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc. 2006; 63(4 Suppl):S29–S34. PMID: 16564909.

2. Nakahara K, Horaguchi J, Fujita N, et al. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009; 44:212–217. PMID: 19214665.

3. Prat F, Fritsch J, Choury AD, Meduri B, Pelletier G, Buffet C. Endoscopic sphincteroclasy: a useful therapeutic tool for biliary endoscopy in Billroth II gastrectomy patients. Endoscopy. 1997; 29:79–81. PMID: 9101143.

4. Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997; 29:69–73. PMID: 9101141.

5. van Buuren HR, Boender J, Nix GA, van Blankenstein M. Needle-knife sphincterotomy guided by a biliary endoprosthesis in Billroth II gastrectomy patients. Endoscopy. 1995; 27:229–232. PMID: 7664700.

6. Feitoza AB, Baron TH. Endoscopy and ERCP in the setting of previous upper GI tract surgery. Part I: reconstruction without alteration of pancreaticobiliary anatomy. Gastrointest Endosc. 2001; 54:743–749. PMID: 11726851.

7. Lee TH, Park do H, Park JY, et al. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest Endosc. 2009; 69(3 Pt 1):444–449. PMID: 19007927.

8. Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999; 31:546–549. PMID: 10533739.

9. Lin CH, Tang JH, Cheng CL, et al. Double balloon endoscopy increases the ERCP success rate in patients with a history of Billroth II gastrectomy. World J Gastroenterol. 2010; 16:4594–4598. PMID: 20857532.

10. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393. PMID: 2070995.

11. Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999; 94:144–148. PMID: 9934745.

12. Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986; 27:1193–1198. PMID: 3781333.

13. Kim MH, Lee SK, Lee MH, et al. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997; 29:82–85. PMID: 9101144.

14. Safrany L, Neuhaus B, Portocarrero G, Krause S. Endoscopic sphincterotomy in patients with Billroth II gastrectomy. Endoscopy. 1980; 12:16–22. PMID: 7353556.

15. Kim GH, Kang DH, Song GA, et al. Endoscopic removal of bile-duct stones by using a rotatable papillotome and a large-balloon dilator in patients with a Billroth II gastrectomy (with video). Gastrointest Endosc. 2008; 67:1134–1138. PMID: 18407269.

16. Maydeo A, Borkar D. Techniques of selective cannulation and sphincterotomy. Endoscopy. 2003; 35:S19–S23. PMID: 12929049.

17. Lee YT. Cap-assisted endoscopic retrograde cholangiopancreatography in a patient with a Billroth II gastrectomy. Endoscopy. 2004; 36:666. PMID: 15243895.

18. Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007; 66:612–615. PMID: 17725957.

19. Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997; 29:74–78. PMID: 9101142.

20. Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007; 22:1210–1213. PMID: 17688662.

21. Jeong EJ, Kang DH, Kim DU, et al. Percutaneous transhepatic choledochoscopic lithotomy as a rescue therapy for removal of bile duct stones in Billroth II gastrectomy patients who are difficult to perform ERCP. Eur J Gastroenterol Hepatol. 2009; 21:1358–1362. PMID: 19282768.

22. Bergman JJ, van Berkel AM, Bruno MJ, et al. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001; 53:19–26. PMID: 11154484.

23. Itoi T, Ishii K, Itokawa F, Kurihara T, Sofuni A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010; 22(Suppl 1):S98–S102. PMID: 20590782.

24. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003; 57:156–159. PMID: 12556775.

25. Attasaranya S, Cheon YK, Vittal H, et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008; 67:1046–1052. PMID: 18178208.

Fig. 1
The technique of wire-guided cannulation of the bile duct. (A) In patients with Billroth II gastrectomy, the ampulla was seen in a reversed position in the gastroscopic view. (B) An en face view of the papilla obtained by controlling the endoscope; a hydrophilic guidewire 0.035-inch in a diameter was preloaded into a triple lumen catheter. After minimal insertion (2 to 3 mm) of the catheter in the ampulla, the guidewire was carefully advanced through the common bile duct (CBD) under fluoroscopy until it was seen to enter the bile duct. Pushing the catheter against the duodenal wall at the 9 to 10 o'clock position or bending the tip of the endoscope (with the protruding tip of the catheter in the orifice of the papilla and upwards bending of the tip of the endoscope) led the tip of the catheter to the correct access to the CBD, i.e., at the 4 to 5 o'clock position. (C) After the catheter was removed, the guidewire was left in the lumen of CBD. (D) Endoscopic sphincterotomy by using a Soehendra Billroth II sphincterotome was performed along the guidewire directed at the 5 o'clock.

Fig. 2
Endoscopic views of common bile duct (CBD) stone removal by using only endoscopic sphincterotomy (EST) or endoscopic papillary balloon dilatation (EPBD) in a patient with Billroth II gastrectomy. (A, B) After only EST of the major papilla was performed, a CBD stone was removed with a stone basket catheter. (C, D) After EPBD followed by EST, relatively large stones were easily extracted out of the bile duct with a balloon catheter.

Fig. 3
Needle knife fistulotomy in two patients with Billroth II gastrectomy. (A, B) After selective biliary cannulation failed, an en face view of the papilla was obtained by controlling the endoscope. After a small and deep incision was performed on the reversed roof of the ampulla by using needle knife, access to the common bile duct was obtained.

Fig. 4
Flow chart of the treatment results of 46 patients with Billroth II gastrectomy. CBD, common bile duct; IHD, intrahepatic bile duct; PTCS, percutaneous transhepatic choledochoscopy.

Table 1
Patient Characteristics and Final Diagnoses after ERCP in Patients Who Had Undergone Billroth II Gastrectomy




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download