Abstract
Endoscopic ultrasound (EUS) is a useful diagnostic tool for evaluation of esophagogastric varices and guidance of endoscopic therapy. EUS can visualize not only collateral veins around the esophagus but also perforating veins that connect esophageal varices with collateral veins. They are associated with high risk of bleeding and early recurrence after initial variceal eradication. Isolated gastric varices can be easily diagnosed using EUS that mimic thickened gastric folds or subepithelial tumors. EUS-guided endoscopic therapy is a challenging field of variceal bleeding. It has a potential role for assistance of interventions and evaluation of treatment outcome.
Endoscopy has a critical role in acute esophageal variceal bleeding.1 Endoscopic injection sclerotherapy and band ligation has been proven to be effective in prevention and control of acute variceal bleeding. Recently, endoscopic ultrasound (EUS) has shown its potential for evaluation of gastroesophageal varices.2 During endoscopy, EUS with a miniaturized ultrasonography can be performed. EUS with conventional echoendoscope equipped with doppler can also be performed before endoscopic therapy. EUS shows a cross-section of esophageal varices and the changes in collateral veins around the esophagus. Perforating veins connect the varices with collateral veins through the esophageal wall. These veins are associated with early recurrence or bleeding of esophageal varices.3,4 Prediction of variceal recurrence or aggravation after variceal eradication would be improved, if EUS might be used for evaluation of the perforating veins.
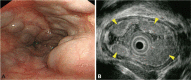
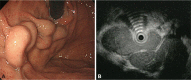
Increased portal pressure can develop collateral veins around the distal esophagus and stomach. EUS can detect vascular changes of these areas in an early stage. A high-frequency (20 MHz) endoluminal miniature probe facilitated greater resolution of submucosal vessels and esophageal varices.5 During conventional endoscopy, EUS can be performed easily by introduction of the miniature probe through a biopsy channel. Endoscopic view of esophageal varices is well correlated with EUS finding (Fig. 1). Miller et al.6 showed EUS can measure the severity of esophageal varices by summing the cut-surface area with digitized image. The measured area was well correlated with risk of bleeding. EUS allows detection of early changes in submucosal veins in the cardia and fundus of the stomach (Fig. 2). Small gastric varices that mimic thickened gastric folds can be easily differentiated. The thickness of the variceal wall and hematocystic spots can be evaluated with EUS.7 Duodenal varices or isolated gastric varices other than the fundus are rare. The diagnosis of rare gastrointestinal varices can be difficult but EUS can make it easy revealing hypoechoic tortuous tubular structures in the submucosal layer.8
Peri-esophageal collateral veins (peri-ECVs) are small veins adjacent to esophageal wall. Para-ECVs are larger veins located on the outer side of esophageal wall, which are connected to the superior vena cava through the azygos vein (Fig. 3).2 Large collateral veins were associated with higher risk of variceal bleeding and recurrence of varices following endoscopic treatment.3,9,10 EUS can visualize and evaluate these collateral veins around the esophagus in patients with portal hypertension. EUS also allows visualization of the left gastric vein. The diameter of the left gastric vein is associated with variceal size.11 The azygos vein drains blood from the esophagus to the superior vena cava and may become enlarged due to aggravated portal hypertension.12 With EUS, azygos vein diameter and valuable quantitative and qualitative data including blood flow volume index can be obtained.13
Perforating veins connect esophageal varices to collateral veins outside of the esophageal wall (Fig. 3). Although ECVs could be visualized by computed tomography or magnetic resonance imaging, small perforating veins can be detected only by EUS. Large esophageal varices with high risk of bleeding have correlation with the number and size of perforating veins.14 Large perforating veins were more frequent in large varices. When blood flow in a perforating vein was studied using color doppler, 45% to 88% of perforating veins exhibited inflow from the collateral veins into the varices.4,15 Most perforating veins, particularly in large esophageal varices, seem to be associated with aggravation or recurrence of the varices.
Before endoscopic therapy, knowledge of the inflow pattern of the varices might be useful to make a treatment plan. Esophageal varices drain portal blood flow from the cardiac submucosal veins or perforating veins. If the varices receive blood from only the cardiac veins, endoscopic treatment should be focused in the cardia and esophagogastric junction. This cardiac inflow pattern of esophageal varices was seen in 60% of cirrhotic patients.16 Large collateral veins and perforating veins might be connected to the esophageal varices. Previous studies showed large para-ECVs (>5 mm) were associated with high rates of variceal recurrence and rebleeding.17,18 The increased risk of bleeding seems to be associated with large perforating veins. Therefore, the high-risk patients need more intensive treatment and close follow-up.3,19 The anterior branch of left gastric vein was associated with poor response to endoscopic treatments.20 The morphology and blood flow of the vein can be evaluated with color Doppler EUS.
Under EUS guidance, injection of sclerosant can be done confidently into esophageal varices. This procedure might decrease the recurrence rate of esophageal varices after the endoscopic therapy.21 A randomized controlled study showed EUS-guided injection sclerotherapy is safe and effective as compared with injection therapy alone in the treatment of esophageal varices.2,22
Endoscopic therapy is not easy to perform in patients with bleeding gastric varices. EUS can guide injection of cyanoacrylate into gastric varices and evaluate the success of the treatment. Transesophageal EUS-guided coil and cyanoacrylate glue treatment of gastric fundal varices was successful in a report.23 Remnant varices are easily visualized by EUS. Recently, successful EUS-guided glue injection was reported.24,25
EUS can be used for evaluation of not only gastroesophageal varices but also perforating and collateral veins outside of the esophagus. Perforating veins might be associated with large varices, early recurrence, or rebleeding. Evaluation of perforating veins and detailed imaging of collateral veins increased our understanding of esophageal varices. EUS is useful for early diagnosis of varices, assessment of the risk of bleeding, and prediction of early recurrence in patients with portal hypertension. EUS guided variceal treatment deserves further study to determine if it can improve safety and efficacy over conventional endoscopic injection therapy.
Further studies are also required to demonstrate conclusively the role of EUS in improving the survival of patients with esophageal varices.
References
1. Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases. Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007; 46:922–938. PMID: 17879356.

2. El-Saadany M, Jalil S, Irisawa A, Shibukawa G, Ohira H, Bhutani MS. EUS for portal hypertension: a comprehensive and critical appraisal of clinical and experimental indications. Endoscopy. 2008; 40:690–696. PMID: 18609464.

3. Irisawa A, Saito A, Obara K, et al. Endoscopic recurrence of esophageal varices is associated with the specific EUS abnormalities: severe periesophageal collateral veins and large perforating veins. Gastrointest Endosc. 2001; 53:77–84. PMID: 11154493.

4. Sato T, Yamazaki K, Toyota J, et al. Perforating veins in recurrent esophageal varices evaluated by endoscopic color Doppler ultrasonography with a galactose-based contrast agent. J Gastroenterol. 2004; 39:422–428. PMID: 15175939.

5. Miller LS, Schiano TD, Adrain A, et al. Comparison of high-resolution endoluminal sonography to video endoscopy in the detection and evaluation of esophageal varices. Hepatology. 1996; 24:552–555. PMID: 8781323.

6. Miller L, Banson FL, Bazir K, et al. Risk of esophageal variceal bleeding based on endoscopic ultrasound evaluation of the sum of esophageal variceal cross-sectional surface area. Am J Gastroenterol. 2003; 98:454–459. PMID: 12591068.

7. Schiano TD, Adrain AL, Vega KJ, Liu JB, Black M, Miller LS. High-resolution endoluminal sonography assessment of the hematocystic spots of esophageal varices. Gastrointest Endosc. 1999; 49(4 Pt 1):424–427. PMID: 10202053.

8. Wu CS, Chen CM, Chang KY. Endoscopic injection sclerotherapy of bleeding duodenal varices. J Gastroenterol Hepatol. 1995; 10:481–483. PMID: 8527718.

9. Faigel DO, Rosen HR, Sasaki A, Flora K, Benner K. EUS in cirrhotic patients with and without prior variceal hemorrhage in comparison with noncirrhotic control subjects. Gastrointest Endosc. 2000; 52:455–462. PMID: 11023560.

10. Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Akaike J. Endoscopic ultrasonographic evaluation of hemodynamics related to variceal relapse in esophageal variceal patients. Hepatol Res. 2009; 39:126–133. PMID: 19208033.

11. Hino S, Kakutani H, Ikeda K, et al. Hemodynamic assessment of the left gastric vein in patients with esophageal varices with color Doppler EUS: factors affecting development of esophageal varices. Gastrointest Endosc. 2002; 55:512–517. PMID: 11923763.

12. Salama ZA, Kassem AM, Giovannini M, Hunter MS. Endoscopic ultrasonographic study of the azygos vein in patients with varices. Endoscopy. 1997; 29:748–750. PMID: 9427495.

13. Kassem AM, Salama ZA, Zakaria MS, Hassaballah M, Hunter MS. Endoscopic ultrasonographic study of the azygos vein before and after endoscopic obliteration of esophagogastric varices by injection sclerotherapy. Endoscopy. 2000; 32:630–634. PMID: 10935792.

14. Irisawa A, Obara K, Sato Y, et al. EUS analysis of collateral veins inside and outside the esophageal wall in portal hypertension. Gastrointest Endosc. 1999; 50:374–380. PMID: 10462659.

16. Nakamura S, Murata Y, Mitsunaga A, Oi I, Hayashi N, Suzuki S. Hemodynamics of esophageal varices on three-dimensional endoscopic ultrasonography and indication of endoscopic variceal ligation. Dig Endosc. 2003; 15:289–297.

17. Leung VK, Sung JJ, Ahuja AT, et al. Large paraesophageal varices on endosonography predict recurrence of esophageal varices and rebleeding. Gastroenterology. 1997; 112:1811–1816. PMID: 9178670.

18. Lo GH, Lai KH, Cheng JS, Huang RL, Wang SJ, Chiang HT. Prevalence of paraesophageal varices and gastric varices in patients achieving variceal obliteration by banding ligation and by injection sclerotherapy. Gastrointest Endosc. 1999; 49(4 Pt 1):428–436. PMID: 10202054.

19. Suzuki T, Matsutani S, Umebara K, et al. EUS changes predictive for recurrence of esophageal varices in patients treated by combined endoscopic ligation and sclerotherapy. Gastrointest Endosc. 2000; 52:611–617. PMID: 11060184.

20. Hino S, Kakutani H, Ikeda K, et al. Hemodynamic analysis of esophageal varices using color Doppler endoscopic ultrasonography to predict recurrence after endoscopic treatment. Endoscopy. 2001; 33:869–872. PMID: 11571684.

21. Lahoti S, Catalano MF, Alcocer E, Hogan WJ, Geenen JE. Obliteration of esophageal varices using EUS-guided sclerotherapy with color Doppler. Gastrointest Endosc. 2000; 51:331–333. PMID: 10699783.

22. de Paulo GA, Ardengh JC, Nakao FS, Ferrari AP. Treatment of esophageal varices: a randomized controlled trial comparing endoscopic sclerotherapy and EUS-guided sclerotherapy of esophageal collateral veins. Gastrointest Endosc. 2006; 63:396–402. PMID: 16500386.
23. Binmoeller KF, Weilert F, Shah JN, Kim J. EUS-guided transesophageal treatment of gastric fundal varices with combined coiling and cyanoacrylate glue injection (with videos). Gastrointest Endosc. 2011; 74:1019–1025. PMID: 21889139.

24. Iwase H, Suga S, Morise K, Kuroiwa A, Yamaguchi T, Horiuchi Y. Color Doppler endoscopic ultrasonography for the evaluation of gastric varices and endoscopic obliteration with cyanoacrylate glue. Gastrointest Endosc. 1995; 41:150–154. PMID: 7721004.

25. Lee YT, Chan FK, Ng EK, et al. EUS-guided injection of cyanoacrylate for bleeding gastric varices. Gastrointest Endosc. 2000; 52:168–174. PMID: 10922086.

Fig. 1
Esophageal varices. (A) Endoscopic image shows large esophageal varices. (B) Endoscopic ultrasound image shows esophageal varices (arrowheads) using a miniature probe (20 MHz) in the same patient.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download