Abstract
Now colorectal cancer is the second most common cancer in males and the fourth most common cancer in females in Korea. Since most of colorectal cancers occur after the prolonged transformation of adenomas into carcinomas, early detection and removal of colorectal adenomas are one of the most effective methods to prevent colorectal cancer. Considering the increasing incidence of colorectal cancer and polyps in Korea, it is very important to establish Korean guideline for colorectal cancer screening and polyp detection. The guideline was developed by the Korean Multi-Society Take Force and we tried to establish the guideline by evidence-based methods. Parts of the statements were draw by systematic reviews and meta-analyses. Herein we discussed epidemiology of colorectal cancers and adenomas in Korea and optimal methods for screening of colorectal cancer and detection of adenomas including fecal occult blood tests, radiologic tests, and endoscopic examinations.
According to the statistical yearbook of the Ministry of Health and Welfare, crude colorectal cancer incidence rates in Korea in 2008 were 54.7 and 36.9 per 100,000 among males and females, respectively. Colorectal cancer is thus the second most common cancer in males and the fourth most common cancer in females.1 The mortality rates (the number of deaths per 100,000 people, %) of colorectal cancer in 2008 were 15.4% among males and 12.1% among females. Colorectal cancer is thus the fourth most common cause of cancer death among Korean males and the second most common cause of cancer death among Korean females. The age-standardized mortality rates of colorectal cancer continue to increase, unlike those of other common cancers, including lung cancer, liver cancer and stomach cancer, whose mortality rates have decreased in recent years. Increases in the incidence of colo-rectal cancer may be partly due to Westernization of many Koreans' lifestyles. Greater public awareness of colorectal cancer and the addition of colorectal cancer in 2004 to the national cancer screening program are likely also responsible in part for the increased incidence rates. Participation rates in the national colorectal screening program increased from approximately 10% in 2004 to over 20% in 2008. In 2009, the participation rate was 25.9%, and more than 1.1 million patients were screened.2
Because most cases of colorectal cancer occur after the prolonged transformation of adenomas into carcinomas, early detection and removal of colorectal adenomas are effective methods of secondary prevention of colorectal cancer. Advanced adenomas are clearly precancerous lesions and serve as surrogate markers of colorectal cancer (the ultimate target of secondary prevention).3 Survival rates of colorectal cancer in Korea have increased in recent years due to higher rates of screening and improved colorectal cancer treatment. Before 2000, the survival rate was approximately 50%, the rate increased to 66.3% between 2001 and 2005 and to 70.1% between 2004 and 2008. These results are consistent with data from other countries indicating that the early detection of colorectal cancer by screening in asymptomatic, average-risk adults has reduced mortality rates from this disease.4-6 Considering the increasing incidence of colorectal cancer and polyps, it is important to establish policies on colorectal cancer screening and polyp detection that are suitable for the Korean population.
In this report, we discuss methods of preventing colorectal cancer by detecting advanced adenomas based on the concept of the adenoma-carcinoma sequence. The report will discuss the use of fecal occult blood testing (FOBT) for large-scale colorectal cancer screening and the use of endoscopic and radiologic tests to identify polyps and other structural changes in the colorectal mucosa that occur at the early stages of carcinogenesis.
The guidelines outlined in this report were established for asymptomatic, average-risk adults without a personal history of colorectal cancer, clinical signs and symptoms suspicious for colorectal cancer or a family history suggesting a high risk of colon cancer. Systematic reviews of existing colorectal cancer screening guidelines in Western countries and of the published domestic and foreign literature regarding colorectal cancer screening were performed. Meta-analyses were conducted in some cases to evaluate the timing, methods, benefits and limitations of the tests for colorectal cancer screening and polyp detection. The ultimate goal of this report is to aid practicing physicians. People with symptoms or signs suggestive of the presence of colorectal cancer or polyps do not fall within the scope of these guidelines; such individuals should undergo appropriate diagnostic testing. Although epidemiologic data have been obtained through Korean multi-center studies over the past decade, these studies alone were not felt to provide sufficient information for the establishment of colorectal cancer screening and polyp detection guidelines. To better reflect the reality of medical care in Korea, opinions of domestic experts and endoscopic specialists responsible for colorectal cancer screening were collected to evaluate the levels of evidence on the screening of colorectal cancer and detection of polyps.
The Korean literature on colorectal cancer screening and polyp detection is quite limited. Therefore, most of the evidence used in this report comes from Western guidelines and systematic reviews. Although the results of major studies performed since 2006 were reviewed, the quality of evidence (even among similar studies) based on the grade assessment method was quite low. This was generally due to heterogeneity among the different trials regarding important elements such as the risk of colorectal cancer, demographic differences among patients, qualitative and quantitative differences among screening tests and a lack of standardized test methods. To overcome these limitations and reflect the different approach to polyp care and the different health care environment in Korea, web-based questionnaire surveys were conducted. Furthermore, using the Delphi method, the extent of agreement regarding the guidelines was determined by asking a number of domestic experts to participate in a series of round-table discussion to formulate a consensus on policies regarding colorectal cancer screening and polyp detection.
In May 2010, a committee tasked with the development of clinical practice guidelines for colorectal cancer screening and polyp detection was organized. The committee consisted of nine practice committee members and two consultants from the three major Korean gastroenterology societies: the Korean Society of Gastroenterology (KSG), the Korean Society of Gastrointestinal Endoscopy (KSGE) and the Korean Association for the Study of Intestinal Diseases (KASID). The consultants were Professor Hyo Jong Kim (Kyung Hee University School of Medicine), representing the KSGE and the KASID, and Professor Suk-Kyun Yang (University of Ulsan College of Medicine), representing the KSG. At the first meeting in June 2010, the Development Committee appointed a chairman, Hyun-Soo Kim (Yonsei University Wonju College of Medicine), and a secretary, Dong-Hoon Yang (University of Ulsan College of Medicine). The committee was divided into three teams: one associated with colorectal cancer screening and colorectal polyp detection (Team leaders: Hyun-Soo Kim from Yonsei University Wonju College of Medicine; Bo In Lee from The Catholic University of Korea College of Medicine; Seong-Eun Kim from Ewha Womans University School of Medicine; and Sung Pil Hong from Yonsei University College of Medicine), one associated with surveillance (Team leaders: Young-Ho Kim from Sungkyunkwan University School of Medicine; Sung Noh Hong from Konkuk University School of Medicine; and Dong-Hoon Yang from University of Ulsan College of Medicine), and one associated with treatment (Team leaders: Dong Il Park from Sungkyunkwan University School of Medicine; Suck Ho Lee from Soonchunhyang University College of Medicine; and Sung Jae Shin from Ajou University School of Medicine). Between June and July 2010, during the first and second workshops, the committee members learned methodologies for guideline development from various experts, including Professor Hyeong-Sik Ahn, the chairman of the Korean Medical Guideline Advisory Committee of the Korean Academy of Medical Science. The committee members shared experiences in the process of clinical practice guideline development with Professor Joong-Wonk Park (Department of Internal Medicine, National Cancer Center), Professor Eun Sook Lee (Department of Surgery, National Cancer Center) and Professor Byong Duk Ye (Department of Gastroenterology, University of Ulsan College of Medicine). Thereafter, the methods, scope, schedule and direction of the clinical practice guideline development were discussed. It was decided to adapt evidence-based foreign guidelines for screening and surveillance to avoid unnecessary duplication of effort. Revisions were made to fit our practice situation, and some topics were subject to meta-analysis and systematic review using the newest data. Because there were no relevant foreign guidelines for endoscopic trea-tment for colorectal polyps, it was decided to develop new guidelines based on systematic literature reviews and meta-analyses. In September 2010, Professor Hyun Jung Kim (Department of Preventive Medicine, Korea University College of Medicine) was invited to share her opinions on guideline development methodologies, systematic literature review and meta-analysis.
Key questions were identified by the practice committee and were organized, to the extent possible, according to the Patient, Intervention, Comparison and Outcome format. Each question was investigated by performing a literature search, and evidence tables for each key question were made. The screening test team selected clinical practice guidelines or recommendations for adaptation. The team considered whet-her the guidelines had been written in English and took into account the American or European society who developed them. Evidence tables were included and evaluated with the Appraisal of Guidelines for Research & Evaluation II tool. From this analysis, 10 recommendations were extracted. In December 2010, Professor Se Hyung Kim (Department of Radiology, Seoul National University College of Medicine) and Professor Hae Jeong Jeon (Department of Radiology, Konkuk University School of Medicine), who are experts in computed tomography (CT) colonography and the use of double-contrast barium enemas (DCBEs) for colorectal cancer screening, joined the committee as a team member and a consultant representing the Korean Society of Abdominal Radiology, respectively. To investigate the screening, surveillance and endoscopic treatment of polyps in Korea, questionnaire surveys were conducted between January and February 2011 among 263 members of the KASID. The results of the questionnaire can be utilized as a comparative indicator of future adherence to the new guidelines. In April 2011, the results of the surveys were presented at the spring conference of the KASID. In addition, keypad voting was conducted in April 2011 during the spring symposium of the Korean Societies of Gastroenterology Association. The voting was performed before and after presenting evidences and foreign guidelines on various aspects of screening, surveillance, and endoscopic treatment to assess the influence of education on clinicians' decisions regarding the management of polyps. In July 2011, drafts of key phrases were completed with the help of external experts, and 45 experts gathered to determine the extent of agreement using the Delphi method. The expert panels consisted primarily of councilors and current members of the KSG, the KSGE and the KASID, as well as 11 members of the Korean Society of Abdominal Radiology. Final key phrases for the developed guidelines were chosen when over 50% agreement was obtained. The determination of 50% agreement was made when the sum of responses of 'completely agree,' 'mostly agree' and 'partially agree,' based on the five-level Likert scale, was greater than 50%. The draft of the report obtained official approval from the multiple societies involved in polyp management after a public hearing that was held in August 2010. The evidence bases of the key phrases were presented in a seminar of the KSGE. The final report was announced at the autumn conference of the KSG in November 2011. There was no conflict of interest among any of the committee members participating in the development process of these clinical practice guidelines.
The developed guidelines will be co-published in the journals of the KSG, the KSGE, the KASID and the journal of the Korean Society of Radiology. The guidelines will also be published through the websites of the relevant societies and in major medical newspapers. Additionally, the contents will be widely distributed through summary guidebooks to training hospitals.
After a certain amount of time has passed after the distribution and implementation of the guidelines, adherence to the guidelines in clinical practice will be assessed. Furthermore, the contents will be periodically revised to reflect the latest clinical knowledge.
To support the need for establishing Korean clinical practice guidelines, key questions regarding the epidemiology of colorectal cancer and polyps in Korea were chosen. Key questions also included whether FOBT, CT colonography, DCBE or colonoscopies are appropriate colorectal cancer screening and colorectal adenoma detection methods. Information regarding risk factors for colorectal cancer and polyps is contained in the appendix.
Literature regarding screening tests was sought using two search databases, Medline's PubMed and the National Guideline Clearinghouse (NGC), and one secondary literature search engine, Trip. Because NGC is a database where only guidelines have been collected, three key terms (colorectal cancer, screening and diagnosis) were searched together, and links that included all three search terms were investigated to review major guidelines, including those of the USA and the European Union. In PubMed, clinical trials published in English from January 2006 to June 2010 were searched using the following sets of key words: 1) "colon adenoma," "colon neoplasm," "colon polyp" or "colorectal cancer"; 2) "screening," "asymptomatic" or "average risk"; and 3) key words for each screening test method. The terms "colonoscopy" or "sigmoidoscopy" were searched separately to compare each screening method. Regarding epidemiology investigations, the key word, "Korean" was used; for FOBT tests, "fecal occult blood test," "FOBT," "FIT," and "fecal immunochemical test" were used; for CT colonography, "CT colonography," "CTC," "virtual colonoscopy," "VC," and "colonography, computed tomographic" were used; and for double-contrast barium enema (DCBE), "double contrast barium enema," "barium study," and "DCBE" were used. Limits based on the study design and the quality of each paper were excluded based on opinions collected from the practice committee.
A total of 6,304 papers from the world literature (1,409 on epidemiology, 833 on FOBT, 201 on CT colonography, 45 on DCBE, 2,743 on sigmoidoscopy and 1,073 on colonoscopy) were identified. Overlapping papers were excluded, and papers that did not meet the selection criteria were excluded by reviewing the paper titles or the full texts of abstracts. When necessary, the suitability of the materials was judged by reviewing the full texts of the papers. Finally, 148 papers (26 on epidemiology, 24 on FOBT, 32 on CT colonography, 18 on DCBE, 29 on sigmoidoscopy and 19 on colonoscopy) were chosen. Literature search methods by subtitle are shown in Fig. 1, and standardized evidence tables were prepared to extract data corresponding to individual key questions from the selected pieces of literature.
Meta-analyses were conducted on FOBT and CT colonography. All studies included in the analyses were observational studies. To minimize clinical heterogeneity among the studies, studies with similar groups of enrolled subjects and test methods were selected.
The sensitivity and specificity of FOBT for colorectal cancer and advanced colorectal adenomas compared to colonoscopy were calculated. Meta-analyses were conducted to compare detection rates for colorectal cancer and polyps between the traditional guaiac FOBT and the FIT and between one-time and two-time FIT methods. To minimize heterogeneity am-ong studies, analyses were limited to studies that were similar in terms of the enrolled subjects, state of rehydration, sampling methods, number of tests and positive thresholds. For these meta-analyses, the odds ratios (OR) of polyp detection rates were calculated for the two test methods and for the number of tests conducted. For CT colonography, 9 papers published since 2,000 describing studies only among asymptomatic, average-risk patients were selected through literature searches, and meta-analyses were conducted on these papers. Details of the literature search methods, literature assessments and development of the evidence table are presented in the appendix (Supplementary Table 1).
The sensitivity and specificity of each test method were calculated from papers in which the true positive, false positive, true negative and false negative rates for polyp detection compared with colonoscopies could be calculated. Papers that did not present the individual values were excluded from the analyses. When the I2 value of the analysis was over 50% or when the results of Cochran's Q-test showed p-values <0.1, the results for sensitivity and specificity were assessed as having statistical heterogeneity. The tool used to analyze the diagnostic accuracy of each test was Meta-disc 1.4 (The Ramón y Cajal Hospital, Madrid, Spain); for other meta-analyses, Review Manager version 5.1 (The Cochrane Collaboration, Oxford, UK) was used.
Recommendations are presented based on a systematic review of the selected literature and meta-analyses. The quality of evidence, indicating the degree of scientific evidence that each recommendation has, and the strength of the recommendation were determined following the methodology proposed by the Grading of Recommendations Assessment, Development and Evaluation Working Group (Table 1).7,8
The quality of evidence was assessed to be "high" when the evidence consisted of randomized controlled trials and "low" when evidence included observational studies. However, in cases where studies used as evidence had limitations in the study design or execution, inconsistent results, indirect evidence, imprecise results or publication bias, the quality of evidence was adjusted downward. In cases of observational studies where large effects were observed, where reported effects might have been reduced due to confounding variables or where dose-response gradients existed, the quality of evidence was adjusted upward. The strength of each recommendation was assessed as "strong" or "weak" by considering the balance of desirable and undesirable consequences, the quality of the evidence, the confidence in the values and the references and the effective allocation of medical expenses and resources. That is, in cases where it was judged that following a specific recommendation would lead to significant health benefits or losses for most patients, the strength of the recommendation was classified as "strong." The strength of the recommendation was classified as "weak" in cases where it was judged that following the recommendation would lead to important benefits or loss in terms of the quality of the health of patients but where differences existed among patients, thus leading to the need to consider individual environments, preferences and values.7,8
Colorectal cancer has historically been one of the most common cancers in Western countries. However, the incidence rate has recently been increasing in some Asian countries due to the Westernization of lifestyles and increases in the obese population. The prevalence rates of colorectal cancer are rapidly increasing in Korea, too. According to 2002 data, the age-standardized incidence rates of colorectal cancer had rapidly increased in Asian countries to 49.3 per 100,000 in Japan, 24.7 in Korea and 35.1 in Singapore. For comparison, colorectal cancer rates are 44.4 per 100,000 in North America and 42.9 in Europe. In East Asian countries, colorectal cancer was the third most common cancer among both males and females.9 According to the Korea Central Cancer Registry, the age-standardized incidence rate of colorectal cancer in 1999 was 21.2 per 100,000 and has been increasing every year by 6.3% to 31.7 in 2005 and 35.1 in 2008.1,2,10-12 Among males, the age-standardized incidence rate of colorectal cancer has been increasing every year by 6.9% from 27.0 per 100,000 in 1999 to 47.0 in 2008. Among females, the incidence of colorectal cancer has been increasing every year by 5.2% from 17.1 in 1999 to 25.6 in 2008. In 2008, colorectal cancer thus became the second and fourth most common cancer among males and females, respectively. Whereas cancer mortality rates have been decreasing for stomach and liver cancer, the cancer mortality rate has been increasing for colo-rectal cancer. Colorectal cancer corresponded to the third most common cause of cancer death among males and the fourth among females in Korea.
In Korea, the incidence rate of colorectal adenomas is also increasing in proportion to the rapid increase in colorectal cancers. According to a previous retrospective study, among 2,435 adults aged 50 or more who underwent a screening colonoscopy between 1998 and 2004, colorectal adenomas were found in 30.2% and advanced adenomas in 4.1% of patients. 13 Among males, adenomas and advanced adenomas were found in 35.9 and 5.1% of patients, respectively. Adenomas and advanced adenomas were found in 18.7 and 2.0% of female patients, respectively. The prevalence rates of colorectal adenomas were therefore higher among males. In a recent prospective multicenter study conducted among 2,307 adults aged 50 or more who underwent a screening colonoscopy during 2003 or 2004, colorectal adenomas and advanced adenomas were found in 40.5 and 2.5% of patients, respectively.14 Adenoma prevalence rates in Korea were similar to the Western rates of 25% to 38%, whereas advanced adenoma prevalence rates were lower than the Western rates of 6.1% to 10.5%.15,16 When corrected for age, however, the prevalence rates of advanced adenomas were similar to those in the West.13
It is recommended to begin colorectal cancer screening test and colorectal adenoma detection test from the age of 50 in average-risk groups. However, those who have symptoms or signs that lead to the suspicion of colorectal cancers should receive appropriate diagnostic tests regardless of age.
The incidence rates of colorectal cancer and colorectal adenoma increase with age. According to the 2008 statistics of the Korea Central Cancer Registry, the incidence rates of colorectal cancers by age group were 28.8 per 100,000 in people aged 40 to 49, 82.5 in those aged 50 to 59, 174.5 in those aged 60 to 69 and 245.7 in those aged 70 or more. Thus, the incidence rates rapidly increased in people aged 50 or more.1 Compared to those aged 40 to 49, the risk of advanced adenomas increased in people aged 50 to 54 by a factor of 1.82 (95% confidence interval [CI], 1.38 to 2.40), in people aged 55 to 59 by a factor of 2.38 (95% CI, 1.81 to 3.14) and in people aged 60 to 66 by a factor of 2.91 (95% CI, 2.21 to 3.83). The detection rates of advanced adenomas were therefore high when sc-reening colonoscopies were conducted in populations aged 50 or more.17 According to a prospective study of colonoscopy screenings conducted in 11 Asian countries, the prevalence rates of colorectal neoplasia and advanced neoplasia were 23.9 and 5.8%, respectively, in people older than 50, while the rates were 11.2 and 2.0%, in groups aged less than 50, indicating that the prevalence rates of colorectal neoplasia rapidly increase in individuals aged 50 or older. In Korea, whereas the prevalence rates of colorectal adenomas and advanced adenomas were 14.3% to 22.6% and 1.1% to 1.6%, respectively, in asymptomatic, average-risk people under 50, the rates were 29.8% to 40.5% and 2.5% to 3.7% in those aged 50 or more.13,14 Based on the aforementioned evidences, the colorectal cancer screening and polyp detection tests are generally recommended in individuals with average risk at the age of 50 or more. However, those who have symptoms or signs that lead to the suspicion of colorectal cancers or polyps should receive appropriate diagnostic tests, including a colonoscopy, regardless of age.
The FOBT is a method of detecting blood in the stool, a finding that may suggest the presence of tumors in the large intestine. The advantage of FOBT is that it is relatively simple, cheap and non-invasive. Thus, this test has been adopted as an effective mass screening test for colorectal cancer in most foreign guidelines. Prior to the development of immunochemical methods in the 1970s and their commercialization in the 1980s,4 guaiac-based tests were the most common types of FOBTs. Although many studies have examined the usefulness of the FOBT for colorectal cancer screening, the detection rates have varied due to differences in test methods, including whether diets are restricted before testing, the number of samples collected per test, and whether the stool specimen is rehydrated.
In average-risk adults aged 50 and older, FOBT is recommended as a large-scale colorectal cancer screening test. This is based on the premise that any positive test should be followed up with colonoscopy.
The sensitivity for diagnosing colorectal cancer in asymptomatic, average-risk groups ranged from 12.9% to 37.1% for one-time testing with an unrehydrated Hemoccult II test, a traditional guaiac based FOBT (gFOBT), to 79.4% for Hemoccult SENSA testing, a high-sensitivity gFOBT.18-21 However, the specificity for diagnosing colorectal cancer tends to be lower for the Hemoccult SENSA test than for the traditional gFOBT. According to a study that compared the results of gFOBT with those of sigmoidoscopy, specificity for colorectal cancer was 97.7% for Hemoccult II and 86.7% for Hemoccult SENSA.21 The integrated sensitivity of high-sensitivity gFOBT for colorectal cancer calculated through a meta-analysis was 74.5% (61.0% to 85.3%), and the specificity was 88.1% (87.6% to 88.7%).18,21-23 Meanwhile, when FITs was used as a colorectal cancer screening test in asymptomatic, average-risk groups, the integrated sensitivity calculated by meta-analysis was 73.0% (63.4% to 80.8%), and the specificity was 94.8% (94.6% to 95.1%) (Fig. 2, Supplementary Fig. 1).18,23-25
The sensitivity can be increased by repeating the gFOBT. Based on the results of a meta-analysis of three observational studies on FITs, the diagnostic accuracy for colorectal advanced neoplasia, including colorectal cancer and advanced adenomas, was significantly higher in cases where the test was repeated two times than in cases where the test was perfor-med only once (OR, 1.46; 95% CI, 1.34 to 1.60; p<0.01).25-28
Fig. 2 show details of this analysis.
Despite the fact that the sensitivity and specificity of the gFOBT for colorectal cancer are low compared to those of colonoscopy, the gFOBT is a useful population screening test for colorectal cancer. According to studies in which patients were followed for 8 to 13 years, the gFOBT reduced colorectal cancer mortality by 15% to 30%.29-31 According to a cohort study that tracked patients for 18 years, the gFOBT increases the rate of colonoscopies, removal of adenomas, and detection of precancerous lesions of colorectal cancer. Consequently, the FOBT is associated with an up to 20% decrease in colorectal cancer incidence rates.32 Although on a relatively small scale, a cohort study in 42,150 subjects followed for 13 years showed that FITs reduced colorectal cancer mortality by 70% and significantly reduced progressive colorectal cancer incidence rates.33 All of these studies are based on the important premise that when fecal guaiac tests show positive results, colonoscopies are performed. That is, any positive FOBT should be followed up with colonoscopy to allow early diagnosis and treatment of the lesions and reduce colorectal cancer mortality.
The sensitivity of FOBT for colorectal adenomas is very low compared to that of colonoscopies. In asymptomatic average-risk groups, the sensitivity for advanced adenomas was 44% (35.5% to 52.0%)18,23 for the Hemoccult SENSA test, a highly sensitive guaiac test, and 24% (21.6% to 27.5%)18,23-25 for FITs. The specificities for advanced colorectal adenomas were 90% (89.5% to 91.1%) for the Hemoccult SENSA test and 95% (94.9% to 95.4%) for FIT, respectively. Therefore, FOBT is not appropriate for colorectal adenoma detection.
In average-risk adults aged 50 and older, FIT is recommended as a colorectal cancer screening test prior to traditional gFOBT.
To judge whether FIT is superior to traditional gFOBT as a colorectal cancer screening test in average-risk groups, the diagnostic sensitivity, convenience and patient compliance associated with the tests should be examined. Although many studies have been conducted to determine the relative accuracy of different tests for colorectal cancer, there are difficulties in comparing these studies because most of them are observational, and subject characteristics and test methods are heterogeneous. In a meta-analysis that compared detection rates between traditional gFOBT and FIT in asymptomatic average-risk groups, the diagnostic accuracy for colorectal cancer was higher for FIT (OR, 1.88; 95% CI, 1.04 to 3.40; p=0.04) (Fig. 3).23,25,34 However, fewer studies have compared colorectal cancer detection rates between high-sensitivity FOBT (Hemoccult SENSA) and FIT. According to a study in 2,351 subjects, the results of the two tests were not significantly different (OR 1.75, 95% CI 0.73 to 4.19, p=0.21).4,23 For evaluating the superiority between high-sensitivity FOBT and FIT, additional studies are needed.
The issue of which FOBT test method is the most useful should also be considered in terms of test convenience and compliance. Guaiac tests measure blood peroxidase in stool and the results are influenced by diet, drugs taken and rehydration of stool specimens. To increase diagnostic accuracy, the test should be repeated 2 to 3 times. In guaiac tests, false positive results may be produced if aspirin or non-steroidal anti-inflammatory drugs have been taken within 7 days before testing and if meat or fish has been ingested within 3 days before testing. False-negative results may be produced if vitamin C has been taken because vitamin C interrupts peroxidase reactions. Thus, vitamin C preparations of 250 mg or more, fruits and juices should be avoided for three days before the test. Rehydration consists of adding a drop of water to the slide containing the stool sample before the test. Although rehydration increases sensitivity, it is generally not recommended because it can raise the number of false-positive results and lead to unnecessary additional tests.4,35
FITs measure antibodies specific to the globin moiety of human hemoglobin, and results are not affected by diet or drug ingestion. Furthermore, because globin is degraded by digestive enzymes in the upper gastrointestinal tract, FITs are more specific for lower gastrointestinal hemorrhage, thereby enhancing the accuracy of the test for colorectal cancer.35,36 Diverse commercialized FITs are available, and the optimal number of stool samples, sample methods, cutoff values, and other specifications should be followed according to the manufacturers' recommendations. Although FIT is relatively more expensive than traditional gFOBT, compliance with FIT is 52.7%. This is significantly higher than compliance with traditional gFOBT at 43.9%,22 which may be due to the advantages listed above, particularly due to the increased convenience.
CT colonography, also known as "virtual colonoscopy," has rapidly evolved along with significant advances in CT imaging technologies. The fundamental elements of CT colonography include fecal and fluid tagging, bowel preparation, colonic distention, CT scanning, interpretation and reporting. The aforementioned elements are important for successful CT colonography. Before the CT colonography examination, the patient should take laxatives for proper cleansing of the colon, and radioopaque contrast media should be given to label the residual fluid and fecal material. The importance of proper colonic distention during CT colonography cannot be overstated. Both supine and prone scans should be routinely obtained. The CT colonography usually takes approximately 10 minutes at the CT scanner. No sedation is required, and patients have the capability to return to work the same day. Recently, research has been performed regarding non-cathartic approaches to minimize the inconvenience of bowel preparation, but these techniques are not yet sufficiently validated.
In average-risk groups aged 50 and older, CT colonography is recommended as one of the colorectal cancer screening and polyp detection methods.
For the detection of colon cancer and advanced adenoma, which is the primary goal of screening for colorectal cancer, recent data suggest that CT colonography is comparable to colonoscopy when state-of-the-art techniques are applied.37-47 According to a study of 1,233 asymptomatic average-risk adults, the per-patient sensitivity of CT colonography for adenomas of 10 mm or larger was 94%. The specificity was 96%, which was higher than the 88% sensitivity of colonoscopy.37 However, in two later trials, the diagnostic sensitivities of CT colonography in patients with adenomas of 10 mm or larger were 55 and 59%, which were much lower than those demonstrated in the earlier studies.48,49 These two studies are limited, however, because they did not evaluate screening in an asymptomatic population, nor did they use the latest CTC techniques. According to 2005 and 2009 meta-analyses that included 33 and 47 prospective studies, respectively,38,39 on a per-patient basis, the pooled sensitivity and specificity of CT colonography for large polyps (≥10 mm) were 83% to 85% and 92% to 97%, respectively, and 60% to 70% and 90% to 93% for 6 to 9 mm polyps. Thereafter, a trial was initiated by the American College of Radiology (ACR) Imaging Network to assess the performance of CT colonography in an asymptomatic average-risk group. This study was conducted in a large screening cohort of 2,531 patients at 15 leading institutions in the USA. State-of-the-art techniques used for almost all cases in the trial included oral contrast tagging, colonic distention with automated CO2 insufflators, multi-detector CT (≥16 slices) and 3D polyp detection on a dedicated CT colonography software system.40 Based on the results, the per-patient sensitivity and specificity for detecting 10 mm or larger adenomas were 90% and 86%, respectively. The corresponding rates for 6 mm or larger adenomas were 78% and 88%, respectively. The diagnostic performance of CT colonography can be greatly affected by the techniques used, and results improved when multi-detector row CT with thinner slice collimation and the 3D fly-through were used.38 In this respect, the ACR recommends using appropriate bowel preparation, optimized imaging and interpretation techniques for CT colonography.50 The prerequisites for facilitating quality implementation of and patient safety with CT colonography in Korea include proper bowel preparation, adequate insufflation, appropriate use of a multi-detector row CT scanner and low-dose CT colonography technical parameters, and a dedicated software system for CT colonography. Interpretation of CT colonography must be performed by adequately trained radiologists on endoscopically confirmed CT colonography cases.
According to the results of a meta-analysis of data from nine studies conducted only in asymptomatic average-risk groups after 2000,37,40-47 the per-patient diagnostic sensitivity of CT colonography for polyp detection was 78% to 100%, and the sensitivity increased as polyps became larger. The pooled sensitivity was 91.3% for 10 mm or larger polyps and 82.2% for 6 mm or larger polyps. The per-polyp sensitivity of CT colonography was 60% to 100%, which was also enhanced as polyps became larger. The pooled per-polyp sensitivity was 87.2% for 10 mm or larger polyps and 75.4% for 6 mm or larger polyps. The per-patient diagnostic specificity of CT colonography was 80% to 99% for 6 mm or larger polyps. Specificity was similar regardless of polyp size. The results of the meta-analysis are described in detail in Fig. 4.
Furthermore, because the risk for colonic perforation or bleeding is extremely low, CT colonography is also a safe and noninvasive method.37,40,44,47,51-54 It has been reported that if CT colonography is used for screening, the risk of perforation among asymptomatic subjects is very low. Based on analyses of eight studies regarding perforation after CT colonography,37,40,44,47,51-54 only 2 cases (0.009%) and 7 cases (0.06%) of perforation were reported in two multicenter studies from 11 and 16 institutions, respectively.53,54 The frequency of major perforation is therefore lower than that of colonoscopies (0.1%).4 Among the total 9 cases of colorectal perforation, only one case occurred in an asymptomatic adult undergoing a screening test, indicating that complications rarely occur in CT colonography. In particular, colonic distention with low-pressure carbon dioxide delivery may be safer than manual insufflation of room air.55
Because CT colonography produces CT images not only of the colon but also of the upper and lower abdomen, there is a chance that incidental extracolonic findings will be detected. The results of 11 CT colonography studies, where lesions outside the colon were mentioned,37,40,44,47,56-63 show that the rate of detection of extracolonic lesions in CT colonography ranges from 18 to 98% and that the incidence of lesions with 'high' clinical significance ranged from 2% to 35%. The incidence of clinically significant extracolonic lesions in the asymptomatic, average-risk population is approximately 4.5%.57 Patients may benefit from early detection and treatment of 5.5-cm-or-larger aortic aneurysms or extracolonic malignant neoplasms. In many other cases, CT colonography may lead to increased costs associated with additional examinations, added radiation exposure, and unnecessary additional tests. Accordingly, conducting CT colonography using doses of 50 mAs or lower is becoming common.
CT-related radiation exposure may be one of the limitations of CT colonography. According to a recent report issued by the Health Physics Society in the USA, the health effects of low-dose radiation exposure (defined as below 50 to 100 mSv) were considered to be "either too small to be observed or are nonexistent."64 However, due to the rapid increase in imaging technologies, the frequency of radiographic examinations during a typical individual's lifetime has increased. Multiple radiation exposures can be sufficiently high to be of concern. If a 50-year-old individual undergoes a CT colonography test with an estimated dose of 7 to 13 mSv, his or her lifetime risk of colorectal cancer will be 0.044%, and the risk of the occurrence of cancer in any site will be 0.14%.65 Recently, as low-dose CT colonography has become common, it has been reported that if tests are conducted using a four-channel multi-detector CT at a dose of 50 mAs, the radiation dose can be reduced to 5 to 8 mSv. Low-dose tests are therefore strongly recommended.66
As mentioned above, due to its good diagnostic performance and safety profile, CT colonography was suggested as a screening test for colorectal cancer and polyps in the 2008 revised colorectal screening guidelines jointly published by the American Cancer Society (ACS), the US Multi-Society Task Force on Colorectal Cancer (USMSTF), and the ACR.4 In Korea, limitations in the facilities have thus far prevented the implementation of CT colonography as a population-based screening method. However, because CT colonography is a minimally invasive, whole-colon structural examination with high diagnostic performance, it will likely rapidly expand in Korea as it has in the rest of the world.
There is consensus that all patients with one or more polyps larger than 1 cm or with three or more 6 to 9-mm lesions identified on CT colonography should be referred for colonoscopy.4,67 However, the management of patients with two or fewer 6 to 9 mm indeterminate polyps remains controversial. Variable prevalence rates of advanced adenomas among patients with 6 to 9 mm polyps have been reported. Recent studies conducted in a screening population reported the prevalence of advanced adenomas to be 2.7% to 5.3%, lower than the 10 % prevalence found among the high-risk population. 68 Regarding the natural history of 6 to 9 mm polyps, many pre-1990 studies that used colonoscopy or DCBE reported that only some of the 6 to 9 mm polyps grew during surveillance. In general, the size did not change and even decreased in some cases.69-72 In a recent study using CT colonography, when 128 cases of 6 to 9 mm polyps were followed for an average of 1.4 years, only 12 polyps (9.4%) became larger. The remaining polyps did not change in size, became smaller or disappeared.73 However, a limited number of studies have evaluated the natural history of polyps in this size range, and additional large population-based studies are necessary. In conclusion, based on the results from previous studies and until further evidence is available to provide additional guidance, a reasonable approach at this time for patients with 6 to 9 mm polyps identified on CT colonography is to recommend colonoscopy. Patients who decline colonoscopy or who are not good candidates for colonoscopy should be offered follow-up surveillance with CT colonography or colonoscopy.
There are limited studies on surveillance periods in patients with negative CT colonography results. Furthermore, the optimal management of patients with 5 mm or smaller polyps detected on CT colonography is controversial, and experts have thus recommended different policies.67,74,75 The risk of advanced adenoma in 5 mm or smaller polyps is very low. In a recent study of a screening cohort, the prevalence of advanced adenoma in patients with 5 mm or smaller polyps was 1.7%. Given the low risk of 5 mm or smaller polyps and the high sensitivity (at least 80%) of CT colonography for 6 mm or larger polyps,11,37,40-47 5 year surveillance using CT colonography or colonoscopy is recommended.
DCBE is an imaging technique that evaluates the entire colon by coating the mucosal surface with high-density barium and distending the colon with air introduced through a thin, flexible catheter that is inserted into the rectum. Multiple radiographic images are obtained from various positions during direct fluoroscopic evaluation. The test takes approximately 10 to 20 minutes. Although patients may experience discomfort during or after the examination, sedation is not necessary, and the patient can return to daily life immediately after the examination.
In average-risk groups aged 50 and older, DCBE is recommended as one of the colorectal cancer screening tests.
Much of the literature describing the diagnostic performance of DCBEs is limited by a retrospective study design and lack of results from an asymptomatic, average-risk group.76-88 Many studies assessing the detection rate of colon cancer using DCBE analyzed all patients in an institution- or population-based database who had been diagnosed with colon cancer and had been assessed with a prior DCBE within a certain period of time. In most studies, the sensitivity for DCBE in detecting colon cancer was reported as 85% to 97%.76-88 However, a recent study showed a rate of new or missed colon cancer after DCBE of 22.4%, demonstrating that the diagnostic performance of DCBE was affected by several factors, including the quality of the study or the person who performed the study.89 Comparing different studies regarding the performance of DCBE in diagnosing polyps is more difficult owing to heterogeneous study designs. In particular, thresholds of target lesion size, morphologic classification, and histopathologic correlation often varied across the studies. According to the two studies performed in asymptomatic patients under surveillance due to a history of prior polypectomy, the sensitivity of DCBE was 48% for 10 mm or larger adenomas and 53% for 6 to 9 mm adenomas.90,91 In one study, DCBE detected six out of eight polyps that were pathologically shown to be advanced adenomas (75% sensitivity).92 Among 470 patients without polyps on colonoscopy, 83 had positive findings on DCBE, yielding a specificity of 82.3%.91 Given the low sensitivity of DCBE to polyps, DCBE is not appropriate as a polyp screening method. Furthermore, because the diagnostic performance of DCBE in diagnosing colorectal cancer and polyps can be affected by many factors, appropriate quality control should precede the test. That is, patients should be educated regarding adequate bowel preparation. During the examination, patients should be imaged both in the prone and supine positions. The entire colon should be evaluated in the absence of any retained barium or collapse of segments of the colon. The examination should be performed by radiologists or radiology residents and trained technicians under the supervision of a radiologist.
Colorectal perforation related to DCBE is very rare. Out of 1,987 patients who underwent DCBE, no cases of colorectal perforation occurred.93 In a large survey conducted among board-certified radiologists in the UK, the rate of colorectal perforation was one per 25,000 cases (0.004%), and the rate of perforation was around one per 10,000 cases.94 These rates are lower than that of perforation after colonoscopy (0.1%).4 Therefore, DCBE is advantageous in that it can be conducted even in patients where colonoscopies are contraindicated or have failed. DCBE can also be used to evaluate the entire large intestine. Thus, DCBE can provide a full colonic examination for patients in whom colonoscopy has failed or is contraindicated.
DCBE was adopted as a colorectal cancer screening test method in 1997 by the ACS based on its high sensitivity for colorectal cancer, accessibility and non-invasiveness.95 It is still used as one of the colorectal cancer screening test methods in many revised guidelines.4,96 However, the use of DCBE for colon cancer screening continues to decline, and it is time to reconsider its role in the future.4,96 At present, DCBE can be regarded as a screening option, particularly in areas where colonoscopy resources are limited or when colonoscopy is contraindicated or unsuccessful.
Studies regarding the management of colorectal lesions detected by DCBE are limited. According to the 2008 revised colorectal screening guidelines jointly published by the ACS, the USMSTF and the ACR, in cases where one or more 6 mm or larger polyps are found by DCBE, an additional colonoscopy is recommended.4 Furthermore, no direct evidence exists (except with respect to the use of stool guaiac tests) regarding surveillance periods for colorectal cancer and polyp screening in such patients.97 According to a recent report in a screening population, the probability of advanced adenomas developing from 5 mm or smaller polyps is as low as 1.7%. Given the low sensitivity of DCBE for detecting polyps, in patients without colorectal lesions or who have been found to have 5 mm or smaller polyps, 5 year surveillance using CT colonography or colonoscopy is recommended.
Screening colonoscopy is advantageous because it allows the entire colon to be examined at once, and adenomas or early cancers found during the examination can be removed. Screening colonoscopy also requires bowel preparation, and the quality of preparation significantly affects the quality of the examination. During colonoscopy, conscious sedation is usually performed to minimize pain and discomfort. Perforation may occur during colonoscopy at a frequency of approximately 0.09%,98 mainly in relation to polypectomy.
Although it is clear that colonoscopy can detect colorectal polyps effectively and even remove polyps, it cannot be said to be a perfect test. According to reports, colonoscopy can miss between 6 and 12% of 1 cm or larger adenomas99,100 and up to 5% of colorectal cancers.99,101 In a Korean study, the colonoscopy miss rate for adenomas was 17.7%.102 Thus, qualified colonoscopy is very important to minimize the miss rate.
Colonoscopic withdrawal times should average at least 6 minutes in cases where no biopsy or polypectomy is performed.103 The KSGE's Quality Control and Assessment on National Cancer Screening Program also recommends a mean colonoscopic withdrawal time of 6 minutes or longer.104 According to one study, colonoscopies performed with mean withdrawal times of 6 minutes or more resulted in higher detection rates of advanced neoplasia compared with those with mean withdrawal times of less than 6 minutes (6.4% vs. 2.6%).105 In another study, colonoscopists with higher or lower polyp detection rates could be identified based on their mean withdrawal time around 6 minute.106 In a study conducted in Korea, colonoscopic withdrawal time and polyp detection rates of gastroenterology fellows were also significantly correlated.107
However, because the length, angulations, and degree of bowel preparation can vary by patients and adenoma detection abilities differ by endoscopist, colonoscopic withdrawal time cannot be the only way to assess the quality of a colonoscopy. The most important quality metric is the adenoma detection rate of each endoscopist. In fact, the adenoma detection rate among endoscopists was inversely related with the risk of interval colorectal cancer.108
In average-risk patients aged 50 and older, colonoscopy is recommended with priority for colorectal cancer screening and polyp detection.
Unlike the case of screening sigmoidoscopy, there has been no randomized controlled trial to assess whether screening colonoscopy can reduce colorectal cancer incidence and its related mortality. However, FOBTs and sigmoidoscopy decrease colorectal cancer incidence and its related mortality by removing precancerous lesions or early cancers with colonoscopic. Thus, it can be indirectly assumed that colonoscopy and polypectomy will reduce colorectal cancer incidence and its related mortality.
According to the National Polyp Study of the United States, the colorectal cancer incidence decreased by 76% to 90% in a cohort that underwent colonoscopy and polypectomy compared to three other reference populations.3 Additionally, individuals living in regions where more colonoscopies were performed had lower incidences of colorectal cancer mortality.109 Case-control studies and cohort studies showed that colonoscopy and polypectomy reduced colorectal cancer-related mortality by approximately 65% compared to controls.110,111
However, this effect may be lower in the right colon than in the left colon. The reasons for the decreased rates of colorectal cancer prevention by colonoscopy in the right colon include biological differences between right-sided and left-sided colorectal cancers,112 failure to detect lesions due to poor bowel preparation or inadequate observation.113 Therefore, to visualize lesions in the right colon, adequate preparation and observation technique are very important.
In average-risk patients aged 50 and older, if no colorectal cancer or colorectal adenoma is found at the time of the qualified index colonoscopy, follow-up colonoscopy is recommended five years later. However, in patients with alarming symptoms or with a high risk of interval cancer, surveillance may be performed earlier than 5 years.
Studies regarding the appropriate interval of the follow-up colonoscopy in cases where index colonoscopy is negative are still insufficient. Some of the recommendations are based on indirect evidence from sigmoidoscopy studies.114,115
In many cohort studies and case-control studies, when the index colonoscopy was negative, the incidence of colorectal cancer or advanced adenomas remained low for at least 5 years.116-121 According to the results of a cohort study conducted in Germany,116 among 533 participants with a negative screening colonoscopy, no colorectal cancers occurred during an average surveillance period of 11.9 years, and the incidence of advanced adenoma was significantly lower than in patients who did not undergo colonoscopy for at least 10 years. Therefore, if no colorectal adenomas or colorectal cancers are found during screening colonoscopy among average-risk patients aged 50 and older, it is appropriate to wait for at least five years to perform the next examination. It should be noted that the low rates of colorectal tumors after negative colonoscopy were reported in well-designed prospective cohort studies conducted in several thousand subjects. In these studies, colonoscopies were mainly performed by experts in gastrointestinal endoscopy. However, according to the Canadian colorectal cancer registry, 2% to 9% of the patients with colorectal cancer had a history of colonoscopy during the 7 to 36 months prior to diagnosis, suggesting that colorectal cancer after colonoscopy is not so rare.122,123 Because these results are from retrospective case-control studies where colonoscopy was mainly performed by primary care physicians, the results have important implications in Korea, where a great deal of colorectal cancer screening is performed in primary care institutions. Therefore, considering the incidence of post-colonoscopy colorectal cancer, follow-up colonoscopy may be conducted sooner than 5 years after colonoscopy in patients with alarming symptoms or with a higher risk of interval cancer.
There is still no evidence regarding the appropriate follow-up after screening colonoscopy with suboptimal bowel preparation. Most gastroenterologists tend to advance follow-up rather than to repeat the examination.124 A retrospective study reported high miss rates among 216 patients who had colonoscopy with suboptimal bowel preparation followed by colonoscopy with optimal bowel preparation within 3 years. In this report, the adenoma miss rate was 42%, and the advanced adenoma miss rate was 27%.125 Therefore, in cases where bowel preparation is insufficient, earlier follow-up colonoscopy may be considered.
Sigmoidoscopy is fundamentally similar to colonoscopy but examines less of the colon. It is necessary to inform subjects who are undergoing screening sigmoidoscopy that bowel preparation is required, a certain degree of discomfort can occur during the examination, cancer prevention effects may be limited to the extent of the examination, and positive findings on sigmoidoscopy usually result in a referral for colonoscopy.126
According to currently available study results,127,128 colorectal cancer incidence and its related mortality can be reduced by screening sigmoidoscopy. Sigmoidoscopy can therefore be recommended as one of the possible colorectal cancer screening and polyp detection methods in average-risk groups aged 50 or more.
Standard methods for bowel preparation in screening sigmoidoscopy have not yet been determined. Although oral lavage solutions are more effective than enemas,129,130 1 or 2 sodium phosphate enemas are frequently used based on phy-sician preference.126,131-133 Although the insertion depth may be subjective,134 it is generally recommended to observe at least beyond the splenic flexure or at least 40 cm from the analverge when the endoscope is straightened.126
If any adenomas are identified by sigmoidoscopy, it is necessary to recommend colonoscopy regardless of the adenoma size because the possibility of proximal tumors increases even if the adenoma is small. However, because 2% to 5% of patients may have advanced neoplasms in the proximal colon even without a distal adenoma, colonoscopic examination only in patients with positive sigmoidoscopies may miss advanced neoplasms in the proximal colon.135 If biopsy is not obtained, colonoscopy should be recommended to all patients with one or more polyps >5 mm.136
In cases where screening sigmoidoscopy is negative in average-risk patients aged 50 and older, it is not essential to perform follow-up sigmoidoscopy within 5 years.114,115,137,138 Data are still limited regarding whether the appropriate interval between normal sigmoidoscopy exams should be 5 years or longer, and preexisting guidelines differ.126,139 Although it seems clear that colorectal cancer prevention effects through sigmoidoscopy persist for at least five years, the extent of this examination is limited, and the quality of the examination may be limited due to such problems as insufficient bowel preparation.
In conclusion, because screening sigmoidoscopy has long-term colorectal cancer-preventing effects,114,115 and because colonoscopy has less of a protective effect for right-sided colorectal cancers compared to left-sided cancers,110,140 sigmoidoscopy is considered to be an effective colorectal cancer screening test. However, it is not widely used as a primary test for colorectal cancer screening and polyp detection because it cannot explore the entire colon. Other disadvantages to sigmoidoscopy include the fact that additional examinations such as colonoscopies are required if the sigmoidoscopy is positive and that sigmoidoscopy is less preferred by endoscopists and patients. Finally, colonoscopy is relatively inexpensive in Korea.
Epidemiology of colorectal cancer and colorectal adenomas in Korea
(1) In Korea, the incidence rate of colorectal cancer is increasing.
(2) In Korea, the incidence rate of colorectal adenomas is increasing.
Colorectal cancer screening and polyp detection test guidelines
(1) It is recommended to begin colorectal cancer screening test and colorectal adenoma detection test from the age of 50 in average-risk groups. However, those who have symptoms or signs that lead to the suspicion of colorectal cancers should receive appropriate diagnostic tests regardless of age.
(1) In average-risk adults aged 50 and older, FOBT is recommended as a large-scale colorectal cancer screening test. This is based on the premise that any positive test should be followed up with colonoscopy.
(2) In average-risk adults aged 50 and older, FIT is recommended as a colorectal cancer screening test prior to traditional gFOBT.
(1) In average-risk groups aged 50 and older, CT colonography is recommended as one of the colorectal cancer screening and polyp detection methods.
(2) In the case that a polyp 6 mm or larger is found in CT colonography, a colonoscopy is recommended.
(1) In average-risk groups aged 50 and older, double-contrast barium enema is recommended as one of the colorectal cancer screening tests.
(2) In cases where a 6 mm or larger polyp has been found in double-contrast barium enema, a colonoscopy is recommended.
(1) In average-risk patients aged 50 and older, colonoscopy is recommended with priority for colorectal cancer screening and polyp detection.
(2) In average-risk patients aged 50 and older, if no colorectal cancer or colorectal adenoma is found at the time of the qualified index colonoscopy, follow-up colonoscopy is recommended in five years or later. However, in patients with alarming symptoms or with a high risk of interval cancer, surveillance may be performed earlier than 5 years.
Acknowledgments
We extend profound thanks to Professor Hwang Choi (Department of Internal Medicine, The Catholic University of Korea College of Medicine), Professor Sung-Ae Jung (Department of Internal Medicine, Ewha Womans University School of Medicine) and Professor Seon-Ja Park (Department of Internal Medicine, Kosin University College of Medicine), who gave unsparing advice regarding the development of this guideline for colorectal cancer screening and polyp detection. We express our deep appreciation to Professor So Yeon Kim (Department of Radiology, University of Ulsan College of Medicine) for her great devotion to the completion of this guideline.
We also give great thanks to the Korean Association of Internal Medicine and Korean Physicians Association for their agreement with final version of this guideline.
This study was initiated with the support of the Korean Society of Gastroenterology, the Korean Society of Gastrointestinal Endoscopy, and the Korean Association for the Study of Intestinal Disease. This study was supported by a grant for the Korean Health Technology R&D Project with the Ministry for Health and Welfare of the Republic of Korea (A102065-23).
Notes
References
1. Jung KW, Park S, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011; 43:1–11. PMID: 21509157.

2. Shim JI, Kim Y, Han MA, et al. Results of colorectal cancer screening of the national cancer screening program in Korea, 2008. Cancer Res Treat. 2010; 42:191–198. PMID: 21253320.

3. Winawer SJ, Zauber AG, O'Brien MJ, et al. The National Polyp Study Workgroup. Randomized comparison of surveillance intervals after colonoscopic removal of newly diagnosed adenomatous polyps. N Engl J Med. 1993; 328:901–906. PMID: 8446136.

4. Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008; 58:130–160. PMID: 18322143.

5. U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008; 149:627–637. PMID: 18838716.
6. Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008; 149:638–658. PMID: 18838718.

7. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004; 328:1490. PMID: 15205295.

8. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008; 336:924–926. PMID: 18436948.

9. Sung JJ, Lau JY, Goh KL, Leung WK. Asia Pacific Working Group on Colorectal Cancer. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005; 6:871–876. PMID: 16257795.

10. Shin HR, Won YJ, Jung KW, et al. Nationwide cancer incidence in Korea, 1999-2001: first result using the national cancer incidence database. Cancer Res Treat. 2005; 37:325–331. PMID: 19956367.

11. Jung KW, Won YJ, Park S, et al. Cancer statistics in Korea: incidence, mortality and survival in 2005. J Korean Med Sci. 2009; 24:995–1003. PMID: 19949651.

12. Jung KW, Park S, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010; 25:1113–1121. PMID: 20676319.

13. Choe JW, Chang HS, Yang SK, et al. Screening colonoscopy in asymptomatic average-risk Koreans: analysis in relation to age and sex. J Gastroenterol Hepatol. 2007; 22:1003–1008. PMID: 17608845.

14. Park HW, Byeon JS, Yang SK, et al. Colorectal neoplasm in asymptomatic average-risk Koreans: the KASID prospective multicenter colonoscopy survey. Gut Liver. 2009; 3:35–40. PMID: 20479899.

15. Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000; 343:162–168. PMID: 10900274.
16. Betés M, Muñoz-Navas MA, Duque JM, et al. Use of colonoscopy as a primary screening test for colorectal cancer in average risk people. Am J Gastroenterol. 2003; 98:2648–2654. PMID: 14687811.

17. Regula J, Rupinski M, Kraszewska E, et al. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med. 2006; 355:1863–1872. PMID: 17079760.

18. Allison JE, Sakoda LC, Levin TR, et al. Screening for colorectal neoplasms with new fecal occult blood tests: update on performance characteristics. J Natl Cancer Inst. 2007; 99:1462–1470. PMID: 17895475.

19. Lieberman DA, Weiss DG. Veterans Affairs Cooperative Study Group 380. One-time screening for colorectal cancer with combined fecal occult-blood testing and examination of the distal colon. N Engl J Med. 2001; 345:555–560. PMID: 11529208.

20. Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME. Colorectal Cancer Study Group. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004; 351:2704–2714. PMID: 15616205.

21. Allison JE, Tekawa IS, Ransom LJ, Adrain AL. A comparison of fecal occult-blood tests for colorectal-cancer screening. N Engl J Med. 1996; 334:155–159. PMID: 8531970.

22. Zhu MM, Xu XT, Nie F, Tong JL, Xiao SD, Ran ZH. Comparison of immunochemical and guaiac-based fecal occult blood test in screening and surveillance for advanced colorectal neoplasms: a meta-analysis. J Dig Dis. 2010; 11:148–160. PMID: 20579218.

23. Smith A, Young GP, Cole SR, Bampton P. Comparison of a brush-sampling fecal immunochemical test for hemoglobin with a sensitive guaiac-based fecal occult blood test in detection of colorectal neoplasia. Cancer. 2006; 107:2152–2159. PMID: 16998938.

24. Morikawa T, Kato J, Yamaji Y, Wada R, Mitsushima T, Shiratori Y. A comparison of the immunochemical fecal occult blood test and total colonoscopy in the asymptomatic population. Gastroenterology. 2005; 129:422–428. PMID: 16083699.

25. Park DI, Ryu S, Kim YH, et al. Comparison of guaiac-based and quantitative immunochemical fecal occult blood testing in a population at average risk undergoing colorectal cancer screening. Am J Gastroenterol. 2010; 105:2017–2025. PMID: 20502450.

26. Rozen P, Levi Z, Hazazi R, et al. Quantitative colonoscopic evaluation of relative efficiencies of an immunochemical faecal occult blood test and a sensitive guaiac test for detecting significant colorectal neoplasms. Aliment Pharmacol Ther. 2009; 29:450–457. PMID: 19035980.

27. Rozen P, Comaneshter D, Levi Z, et al. Cumulative evaluation of a quantitative immunochemical fecal occult blood test to determine its optimal clinical use. Cancer. 2010; 116:2115–2125. PMID: 20186820.

28. Grazzini G, Visioli CB, Zorzi M, et al. Immunochemical faecal occult blood test: number of samples and positivity cutoff. What is the best strategy for colorectal cancer screening? Br J Cancer. 2009; 100:259–265. PMID: 19142185.

29. Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996; 348:1472–1477. PMID: 8942775.

30. Kronborg O, Fenger C, Olsen J, Jørgensen OD, Søndergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996; 348:1467–1471. PMID: 8942774.

31. Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999; 91:434–437. PMID: 10070942.

32. Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000; 343:1603–1607. PMID: 11096167.

33. Lee KJ, Inoue M, Otani T, et al. Colorectal cancer screening using fecal occult blood test and subsequent risk of colorectal cancer: a prospective cohort study in Japan. Cancer Detect Prev. 2007; 31:3–11. PMID: 17289293.

34. Wong BC, Wong WM, Cheung KL, et al. A sensitive guaiac faecal occult blood test is less useful than an immunochemical test for colorectal cancer screening in a Chinese population. Aliment Pharmacol Ther. 2003; 18:941–946. PMID: 14616158.

35. Sung JJ, Lau JY, Young GP, et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut. 2008; 57:1166–1176. PMID: 18628378.

36. Lieberman DA. Clinical practice. Screening for colorectal cancer. N Engl J Med. 2009; 361:1179–1187. PMID: 19759380.
37. Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003; 349:2191–2200. PMID: 14657426.

38. Mulhall BP, Veerappan GR, Jackson JL. Meta-analysis: computed tomographic colonography. Ann Intern Med. 2005; 142:635–650. PMID: 15838071.

39. Chaparro M, Gisbert JP, Del Campo L, Cantero J, Maté J. Accuracy of computed tomographic colonography for the detection of polyps and colorectal tumors: a systematic review and meta-analysis. Digestion. 2009; 80:1–17. PMID: 19407448.

40. Johnson CD, Chen MH, Toledano AY, et al. Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 2008; 359:1207–1217. PMID: 18799557.

41. Macari M, Milano A, Lavelle M, Berman P, Megibow AJ. Comparison of time-efficient CT colonography with two- and three-dimensional colonic evaluation for detecting colorectal polyps. AJR Am J Roentgenol. 2000; 174:1543–1549. PMID: 10845478.
42. Macari M, Bini EJ, Jacobs SL, et al. Colorectal polyps and cancers in asymptomatic average-risk patients: evaluation with CT colonography. Radiology. 2004; 230:629–636. PMID: 14739311.

43. Kim YS, Kim N, Kim SH, et al. The efficacy of intravenous contrast-enhanced 16-raw multidetector CT colonography for detecting patients with colorectal polyps in an asymptomatic population in Korea. J Clin Gastroenterol. 2008; 42:791–798. PMID: 18580500.

44. Kim DH, Pickhardt PJ, Taylor AJ, et al. CT colonography versus colonoscopy for the detection of advanced neoplasia. N Engl J Med. 2007; 357:1403–1412. PMID: 17914041.

45. Johnson CD, Fletcher JG, MacCarty RL, et al. Effect of slice thickness and primary 2D versus 3D virtual dissection on colorectal lesion detection at CT colonography in 452 asymptomatic adults. AJR Am J Roentgenol. 2007; 189:672–680. PMID: 17715116.

46. An S, Lee KH, Kim YH, et al. Screening CT colonography in an asymptomatic average-risk Asian population: a 2-year experience in a single institution. AJR Am J Roentgenol. 2008; 191:W100–W106. PMID: 18716076.

47. Graser A, Stieber P, Nagel D, et al. Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut. 2009; 58:241–248. PMID: 18852257.

48. Cotton PB, Durkalski VL, Pineau BC, et al. Computed tomographic colonography (virtual colonoscopy): a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA. 2004; 291:1713–1719. PMID: 15082698.
49. Rockey DC, Paulson E, Niedzwiecki D, et al. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005; 365:305–311. PMID: 15664225.

50. McFarland EG, Fletcher JG, Pickhardt P, et al. ACR Colon Cancer Committee white paper: status of CT colonography 2009. J Am Coll Radiol. 2009; 6:756–772. PMID: 19878883.

51. Benson M, Dureja P, Gopal D, Reichelderfer M, Pfau PR. A comparison of optical colonoscopy and CT colonography screening strategies in the detection and recovery of subcentimeter adenomas. Am J Gastroenterol. 2010; 105:2578–2585. PMID: 20842111.

52. Edwards JT, Mendelson RM, Fritschi L, et al. Colorectal neoplasia screening with CT colonography in average-risk asymptomatic subjects: community-based study. Radiology. 2004; 230:459–464. PMID: 14688402.

53. Pickhardt PJ. Incidence of colonic perforation at CT colonography: review of existing data and implications for screening of asymptomatic adults. Radiology. 2006; 239:313–316. PMID: 16641348.

54. Sosna J, Blachar A, Amitai M, et al. Colonic perforation at CT colonography: assessment of risk in a multicenter large cohort. Radiology. 2006; 239:457–463. PMID: 16543590.

55. Shinners TJ, Pickhardt PJ, Taylor AJ, Jones DA, Olsen CH. Patient-controlled room air insufflation versus automated carbon dioxide delivery for CT colonography. AJR Am J Roentgenol. 2006; 186:1491–1496. PMID: 16714635.

56. Kimberly JR, Phillips KC, Santago P, et al. Extracolonic findings at virtual colonoscopy: an important consideration in asymptomatic colorectal cancer screening. J Gen Intern Med. 2009; 24:69–73. PMID: 18958531.

57. Pickhardt PJ, Hanson ME, Vanness DJ, et al. Unsuspected extracolonic findings at screening CT colonography: clinical and economic impact. Radiology. 2008; 249:151–159. PMID: 18796673.
58. Gluecker TM, Johnson CD, Wilson LA, et al. Extracolonic findings at CT colonography: evaluation of prevalence and cost in a screening population. Gastroenterology. 2003; 124:911–916. PMID: 12671887.

59. Hara AK, Johnson CD, MacCarty RL, Welch TJ. Incidental extracolonic findings at CT colonography. Radiology. 2000; 215:353–357. PMID: 10796907.

60. Ginnerup Pedersen B, Rosenkilde M, Christiansen TE, Laurberg S. Extracolonic findings at computed tomography colonography are a challenge. Gut. 2003; 52:1744–1747. PMID: 14633954.

61. Chin M, Mendelson R, Edwards J, Foster N, Forbes G. Computed tomographic colonography: prevalence, nature, and clinical significance of extracolonic findings in a community screening program. Am J Gastroenterol. 2005; 100:2771–2776. PMID: 16393234.
62. Flicker MS, Tsoukas AT, Hazra A, Dachman AH. Economic impact of extracolonic findings at computed tomographic colonography. J Comput Assist Tomogr. 2008; 32:497–503. PMID: 18664832.

63. Veerappan GR, Ally MR, Choi JH, Pak JS, Maydonovitch C, Wong RK. Extracolonic findings on CT colonography increases yield of colorectal cancer screening. AJR Am J Roentgenol. 2010; 195:677–686. PMID: 20729446.

64. Health Physics Society. Position Statement of the Health Physics Society. Radiation risk in perspective [Internet]. 2012. cited 2011 Dec 11. McLean: Health Physics Society;Available from: http://hps.org/hpspublications/positionstatements.html.
65. Brenner DJ, Georgsson MA. Mass screening with CT colonography: should the radiation exposure be of concern? Gastroenterology. 2005; 129:328–337. PMID: 16012958.

66. Macari M, Bini EJ, Xue X, et al. Colorectal neoplasms: prospective comparison of thin-section low-dose multi-detector row CT colonography and conventional colonoscopy for detection. Radiology. 2002; 224:383–392. PMID: 12147833.

67. Zalis ME, Barish MA, Choi JR, et al. CT colonography reporting and data system: a consensus proposal. Radiology. 2005; 236:3–9. PMID: 15987959.

68. Pickhardt PJ, Kim DH. Colorectal cancer screening with CT colonography: key concepts regarding polyp prevalence, size, histology, morphology, and natural history. AJR Am J Roentgenol. 2009; 193:40–46. PMID: 19542393.

69. Welin S, Youker J, Spratt JS Jr. The rates and patterns of growth of 375 tumors of the large intestine and rectum observed serially by double contrast enema study (Malmoe technique). Am J Roentgenol Radium Ther Nucl Med. 1963; 90:673–687.
70. Hofstad B, Vatn MH, Andersen SN, et al. Growth of colorectal polyps: redetection and evaluation of unresected polyps for a period of three years. Gut. 1996; 39:449–456. PMID: 8949653.

71. Knoernschild HE. Growth rate and malignant potential of colonic polyps: early results. Surg Forum. 1963; 14:137–138. PMID: 14064485.
72. Stryker SJ, Wolff BG, Culp CE, Libbe SD, Ilstrup DM, MacCarty RL. Natural history of untreated colonic polyps. Gastroenterology. 1987; 93:1009–1013. PMID: 3653628.

73. Pickhardt PJ, Kim DH, Cash BD, et al. The natural history of small polyps at CT colonography. In : Meeting for the Society of Gastrointestinal Radiologists; 2008 Feb 17-22; Rancho Mirage, USA.
74. Rex DK, Lieberman D. ACG. ACG colorectal cancer prevention action plan: update on CT-colonography. Am J Gastroenterol. 2006; 101:1410–1413. PMID: 16863539.

75. Rockey DC, Barish M, Brill JV, et al. Standards for gastroenterologists for performing and interpreting diagnostic computed tomographic colonography. Gastroenterology. 2007; 133:1005–1024. PMID: 17678924.

76. Gillespie JS, Kelly BE. Double contrast barium enema and colorectal carcinoma: sensitivity and potential role in screening. Ulster Med J. 2001; 70:15–18. PMID: 11428318.
77. Thomas RD, Fairhurst JJ, Frost RA. Wessex regional radiology audit: barium enema in colo-rectal carcinoma. Clin Radiol. 1995; 50:647–650. PMID: 7554742.

78. Johnson CD, Carlson HC, Taylor WF, Weiland LP. Barium enemas of carcinoma of the colon: sensitivity of double- and single-contrast studies. AJR Am J Roentgenol. 1983; 140:1143–1149. PMID: 6602483.

79. Kelvin FM, Gardiner R, Vas W, Stevenson GW. Colorectal carcinoma missed on double contrast barium enema study: a problem in perception. AJR Am J Roentgenol. 1981; 137:307–313. PMID: 6789638.

80. Thorpe CD, Grayson DJ Jr, Wingfield PB. Detection of carcinoma of the colon and rectum by air contrast enema. Surg Gynecol Obstet. 1981; 152:307–309. PMID: 7466578.
81. Fork FT, Lindström C, Ekelund G. Double contrast examination in carcinoma of the colon and rectum A prospective clinical series. Acta Radiol Diagn (Stockh). 1983; 24:177–188. PMID: 6624520.
82. Reiertsen O, Bakka A, Trønnes S, Gauperaa T. Routine double contrast barium enema and fiberoptic colonoscopy in the diagnosis of colorectal carcinoma. Acta Chir Scand. 1988; 154:53–55. PMID: 3354284.
83. Rex DK, Rahmani EY, Haseman JH, Lemmel GT, Kaster S, Buckley JS. Relative sensitivity of colonoscopy and barium enema for detection of colorectal cancer in clinical practice. Gastroenterology. 1997; 112:17–23. PMID: 8978337.

84. Strom E, Larsen JL. Colon cancer at barium enema examination and colonoscopy: a study from the county of Hordaland, Norway. Radiology. 1999; 211:211–214. PMID: 10189473.

85. McDonald S, Lyall P, Israel L, Coates R, Frizelle F. Why barium enemas fail to identify colorectal cancers. ANZ J Surg. 2001; 71:631–633. PMID: 11736819.

86. Connolly DJ, Traill ZC, Reid HS, Copley SJ, Nolan DJ. The double contrast barium enema: a retrospective single centre audit of the detection of colorectal carcinomas. Clin Radiol. 2002; 57:29–32. PMID: 11798199.

87. Leslie A, Virjee JP. Detection of colorectal carcinoma on double contrast barium enema when double reporting is routinely performed: an audit of current practice. Clin Radiol. 2002; 57:184–187. PMID: 11952311.

88. Tawn DJ, Squire CJ, Mohammed MA, Adam EJ. National audit of the sensitivity of double-contrast barium enema for colorectal carcinoma, using control charts for the Royal College of Radiologists Clinical Radiology Audit Sub-Committee. Clin Radiol. 2005; 60:558–564. PMID: 15851043.
89. Toma J, Paszat LF, Gunraj N, Rabeneck L. Rates of new or missed colorectal cancer after barium enema and their risk factors: a population-based study. Am J Gastroenterol. 2008; 103:3142–3148. PMID: 18853981.

90. Williams CB, Macrae FA, Bartram CI. A prospective study of diagnostic methods in adenoma follow-up. Endoscopy. 1982; 14:74–78. PMID: 7075563.

91. Winawer SJ, Stewart ET, Zauber AG, et al. A comparison of colonoscopy and double-contrast barium enema for surveillance after polypectomy. National Polyp Study Work Group. N Engl J Med. 2000; 342:1766–1772. PMID: 10852998.
92. Glick SN. Comparison of colonoscopy and double-contrast barium enema. N Engl J Med. 2000; 343:1728. PMID: 11185429.

93. Kewenter J, Brevinge H. Endoscopic and surgical complications of work-up in screening for colorectal cancer. Dis Colon Rectum. 1996; 39:676–680. PMID: 8646956.

94. Blakeborough A, Sheridan MB, Chapman AH. Complications of barium enema examinations: a survey of UK Consultant Radiologists 1992 to 1994. Clin Radiol. 1997; 52:142–148. PMID: 9043049.

95. Winawer SJ, Fletcher RH, Miller L, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology. 1997; 112:594–642. PMID: 9024315.

96. Smith RA, Cokkinides V, Eyre HJ. American Cancer Society. American Cancer Society guidelines for the early detection of cancer, 2003. CA Cancer J Clin. 2003; 53:27–43. PMID: 12568442.

97. U.S. Preventive Services Task Force. Screening for colorectal cancer: recommendation and rationale. Ann Intern Med. 2002; 137:129–131. PMID: 12118971.
98. Levin TR, Zhao W, Conell C, et al. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med. 2006; 145:880–886. PMID: 17179057.

99. Rex DK, Cutler CS, Lemmel GT, et al. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology. 1997; 112:24–28. PMID: 8978338.

100. Pickhardt PJ, Nugent PA, Mysliwiec PA, Choi JR, Schindler WR. Location of adenomas missed by optical colonoscopy. Ann Intern Med. 2004; 141:352–359. PMID: 15353426.

101. Bressler B, Paszat LF, Vinden C, Li C, He J, Rabeneck L. Colonoscopic miss rates for right-sided colon cancer: a population-based analysis. Gastroenterology. 2004; 127:452–456. PMID: 15300577.

102. Choi KY, Lee BI, Lee SY, et al. Colonoscopic miss-rate of colorectal polyp and adenoma. Korean J Gastrointest Endosc. 2003; 26:199–204.
103. Rex DK, Petrini JL, Baron TH, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2006; 63(4 Suppl):S16–S28. PMID: 16564908.

104. Lee BI, Hong SP, Kim SE, et al. Korean guidelines for colorectal cancer screening and polyp detection. Korean J Gastroenterol. 2012; 59:65–84. PMID: 22387833.

105. Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006; 355:2533–2541. PMID: 17167136.

106. Simmons DT, Harewood GC, Baron TH, et al. Impact of endoscopist withdrawal speed on polyp yield: implications for optimal colonoscopy withdrawal time. Aliment Pharmacol Ther. 2006; 24:965–971. PMID: 16948808.

107. Ahn SB, Han DS, Bae JH, Byun TJ, Kim JP, Eun CS. The miss rate for colorectal adenoma determined by quality-adjusted, back-to-back colonoscopies. Gut Liver. 2012; 6:64–70. PMID: 22375173.

108. Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010; 362:1795–1803. PMID: 20463339.

109. Rabeneck L, Paszat LF, Saskin R, Stukel TA. Association between colonoscopy rates and colorectal cancer mortality. Am J Gastroenterol. 2010; 105:1627–1632. PMID: 20197758.

110. Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009; 150:1–8. PMID: 19075198.

111. Kahi CJ, Imperiale TF, Juliar BE, Rex DK. Effect of screening colonoscopy on colorectal cancer incidence and mortality. Clin Gastroenterol Hepatol. 2009; 7:770–775. PMID: 19268269.

112. Arain MA, Sawhney M, Sheikh S, et al. CIMP status of interval colon cancers: another piece to the puzzle. Am J Gastroenterol. 2010; 105:1189–1195. PMID: 20010923.

113. Bianco MA, Cipolletta L, Rotondano G, et al. Prevalence of nonpolypoid colorectal neoplasia: an Italian multicenter observational study. Endoscopy. 2010; 42:279–285. PMID: 20235006.
114. Newcomb PA, Storer BE, Morimoto LM, Templeton A, Potter JD. Long-term efficacy of sigmoidoscopy in the reduction of colorectal cancer incidence. J Natl Cancer Inst. 2003; 95:622–625. PMID: 12697855.

115. Selby JV, Friedman GD, Quesenberry CP Jr, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992; 326:653–657. PMID: 1736103.

116. Brenner H, Haug U, Arndt V, Stegmaier C, Altenhofen L, Hoffmeister M. Low risk of colorectal cancer and advanced adenomas more than 10 years after negative colonoscopy. Gastroenterology. 2010; 138:870–876. PMID: 19909750.

117. Imperiale TF, Glowinski EA, Lin-Cooper C, Larkin GN, Rogge JD, Ransohoff DF. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008; 359:1218–1224. PMID: 18799558.

118. Lakoff J, Paszat LF, Saskin R, Rabeneck L. Risk of developing proximal versus distal colorectal cancer after a negative colonoscopy: a population-based study. Clin Gastroenterol Hepatol. 2008; 6:1117–1121. PMID: 18691942.

119. Leung WK, Lau JY, Suen BY, et al. Repeat-screening colonoscopy 5 years after normal baseline-screening colonoscopy in average-risk Chinese: a prospective study. Am J Gastroenterol. 2009; 104:2028–2034. PMID: 19455125.

120. Singh H, Turner D, Xue L, Targownik LE, Bernstein CN. Risk of developing colorectal cancer following a negative colonoscopy examination: evidence for a 10-year interval between colonoscopies. JAMA. 2006; 295:2366–2373. PMID: 16720822.
121. Rex DK, Cummings OW, Helper DJ, et al. 5-year incidence of adenomas after negative colonoscopy in asymptomatic average-risk persons [see comment]. Gastroenterology. 1996; 111:1178–1181. PMID: 8898630.

122. Singh H, Nugent Z, Mahmud SM, Demers AA, Bernstein CN. Predictors of colorectal cancer after negative colonoscopy: a population-based study. Am J Gastroenterol. 2010; 105:663–673. PMID: 19904239.

123. Baxter NN, Sutradhar R, Forbes SS, Paszat LF, Saskin R, Rabeneck L. Analysis of administrative data finds endoscopist quality measures associated with postcolonoscopy colorectal cancer. Gastroenterology. 2011; 140:65–72. PMID: 20854818.

124. Ben-Horin S, Bar-Meir S, Avidan B. The impact of colon cleanliness assessment on endoscopists' recommendations for follow-up colonoscopy. Am J Gastroenterol. 2007; 102:2680–2685. PMID: 17714555.

125. Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, Neugut AI. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc. 2011; 73:1207–1214. PMID: 21481857.

126. Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008; 134:1570–1595. PMID: 18384785.

127. Atkin WS, Edwards R, Kralj-Hans I, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010; 375:1624–1633. PMID: 20430429.

128. Hoff G, Grotmol T, Skovlund E, Bretthauer M;. Risk of colorectal cancer seven years after flexible sigmoidoscopy screening: randomised controlled trial. BMJ. 2009; 338:b1846. PMID: 19483252.

129. Bini EJ, Unger JS, Rieber JM, Rosenberg J, Trujillo K, Weinshel EH. Prospective, randomized, single-blind comparison of two preparations for screening flexible sigmoidoscopy. Gastrointest Endosc. 2000; 52:218–222. PMID: 10922094.

130. Sharma VK, Chockalingham S, Clark V, et al. Randomized, controlled comparison of two forms of preparation for screening flexible sigmoidoscopy. Am J Gastroenterol. 1997; 92:809–811. PMID: 9149190.
131. Underwood D, Makar RR, Gidwani AL, Najfi SM, Neilly P, Gilliland R. A prospective randomized single blind trial of Fleet phosphate enema versus glycerin suppositories as preparation for flexible sigmoidoscopy. Ir J Med Sci. 2010; 179:113–118. PMID: 19655226.

132. Atkin WS, Hart A, Edwards R, et al. Single blind, randomised trial of efficacy and acceptability of oral picolax versus self administered phosphate enema in bowel preparation for flexible sigmoidoscopy screening. BMJ. 2000; 320:1504–1508. PMID: 10834891.
133. Osgard E, Jackson JL, Strong J. A randomized trial comparing three methods of bowel preparation for flexible sigmoidoscopy. Am J Gastroenterol. 1998; 93:1126–1130. PMID: 9672343.

134. Levin TR, Farraye FA, Schoen RE, et al. Quality in the technical performance of screening flexible sigmoidoscopy: recommendations of an international multi-society task group. Gut. 2005; 54:807–813. PMID: 15888789.

135. Lewis JD, Ng K, Hung KE, et al. Detection of proximal adenomatous polyps with screening sigmoidoscopy: a systematic review and meta-analysis of screening colonoscopy. Arch Intern Med. 2003; 163:413–420. PMID: 12588199.
136. Schoen RE, Weissfeld JL, Pinsky PF, Riley T. Yield of advanced adenoma and cancer based on polyp size detected at screening flexible sigmoidoscopy. Gastroenterology. 2006; 131:1683–1689. PMID: 17188959.

137. Doria-Rose VP, Levin TR, Selby JV, Newcomb PA, Richert-Boe KE, Weiss NS. The incidence of colorectal cancer following a negative screening sigmoidoscopy: implications for screening interval. Gastroenterology. 2004; 127:714–722. PMID: 15362026.

138. Burke CA, Elder K, Lopez R. Screening for colorectal cancer with flexible sigmoidoscopy: is a 5-yr interval appropriate? A comparison of the detection of neoplasia 3 yr versus 5 yr after a normal examination. Am J Gastroenterol. 2006; 101:1329–1332. PMID: 16771957.

139. Rex DK, Johnson DA, Anderson JC, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009; 104:739–750. PMID: 19240699.
140. Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010; 102:89–95. PMID: 20042716.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



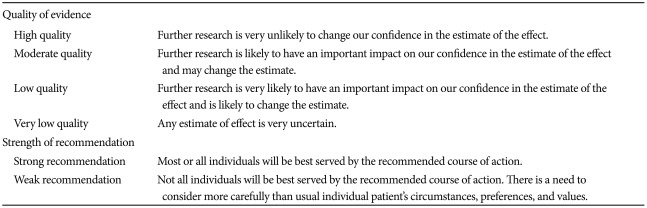



 XML Download
XML Download