Abstract
Background/Aims
Benign colon 18F-fluorodeoxyglucose (FDG) uptake is frequently observed in asymptomatic individuals. Aims of this study were to investigate the benign colon uptake by whole body FDG-positron emission tomography (PET) in asymptomatic adults and to correlate those results with colonoscopic and histologic findings.
Methods
Among 3,540 subjects who had undergone FDG-PET, 43 subjects who were diagnosed to have benign colon uptake in FDG-PET and underwent colonoscopy were retrospectively reviewed. Subjects were classified as diffuse or focal groups based on their FDG uptake patterns. PET results were analyzed together with colonoscopic and histologic findings.
Results
Forty-three subjects showed benign colon uptake in FDG-PET; 28 of them were shown as the diffuse group, while other 15 subjects were classified as the focal group. Five subjects among those showed diffuse uptake were diagnosed as adenoma. Seven among 15 subjects who showed focal uptake were diagnosed as adenocarcinoma (n=2), adenoma (n=3), or non-neoplastic polyp (n=2). Positive predictive values were 25% in the diffuse group and 47% in the focal group.
According to statistics of Korean Central Cancer Registry colon cancer was the third most incident cancer among overall cancers with 24,968 patients per 100,000 populations in 2009, and the fourth most common cause of cancer mortality with 7,701 deaths per 100,000 in 2010.1 As the incidence of cancers, such as colon cancer, increases, 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) is becoming widely used for cancer diagnosis, staging work-up and follow-up.
About 1.3% to 3% of patients show strong focal FDG uptake on PET/computed tomography (CT) image.2 FDG uptake by colon on FDG-PET indicates physiologic lesion; inflammation such as inflammatory bowel disease, benign lesion such as benign polyp, or malignant lesion.3-5 It is crucial, therefore, to differentiate whether the uptake was by phy-siologic or benign lesion or by malignant lesion.
There have been many studies to elucidate differentiation between benign and malignant disease by FDG-PET. We aimed to investigate and compare the frequency, pattern and intensity of benign colon FDG uptake with those of colonoscopic and histologic findings to identify clinical meanings of colon FDG uptake on FDG-PET.
Among 3,540 patients who had undergone FDG-PET for cancer diagnosis, staging, follow-up or screening at Ewha Womans University Medical Center between September 2009 and August 2010, we enrolled 43 patients who were 18 years or more and received colonoscopy with benign colon FDG uptake on FDG-PET, retrospectively.
PET scan was obtained with a PET scanner (Phillips Allegro, Eindhoven, Netherlands) after 6 hours of fasting. Each patient was injected with 370 MBq of F-18-FDG. After 60 minutes, transmission scan was performed for 1 minute per frame from the base of skull to the proximal femoral area, and then emission scan was performed for 3 minutes per frame. PET images were reconstructed with ordered subset expectation maximization algorithm (4 iteration and 8 subsets).
A nuclear medicine physician, who was blind to the endoscopic findings, evaluated the intensities and patterns of colon uptake of FDG-PET, by referring transaxial, sagittal and coronal slice images and projection images, simultaneously. When colon FDG uptake was observed, it was defined as benign based on its anatomical location, intensity and pattern, which was classified into two categories; diffuse group, when the uptake was increased consistently at some length along the colon, and focal group, when the focal increased uptake appeared as a definite nodal pattern (Fig. 1). We also measured the maximum standardized uptake value (SUV) of colon area with the highest uptake in every image.
Colonoscopy was performed by a gastroenterologist, without blinding to the FDG-PET findings, in patients who consented to colonoscopy among those referred to the department of gastroenterology with benign colon uptake on FDG-PET imaging. Lesion's location, size and pathologic results were described, when applicable.
Analysis was performed in 43 patients who had shown benign colon FDG uptake on FDG-PET and received colonoscopy. Additionally, in order to evaluate the difference of maximal SUV values by histologic findings when diagnosed as malignant lesion on histology, 10 patients with benign FDG uptake and malignant lesion were compared with 50 patients who had shown malignant colon FDG uptake on FDG-PET and received histological examination during the same period.
SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Chi-square test was performed to compare difference of endoscopic results by the pattern of colon uptake on FDG-PET scan. Mann-Whitney test or Kruskal-Wallis test was performed to compare the estimated maximal SUV and the size of adenoma of each group. A p-value of 0.05 or less was considered significant.
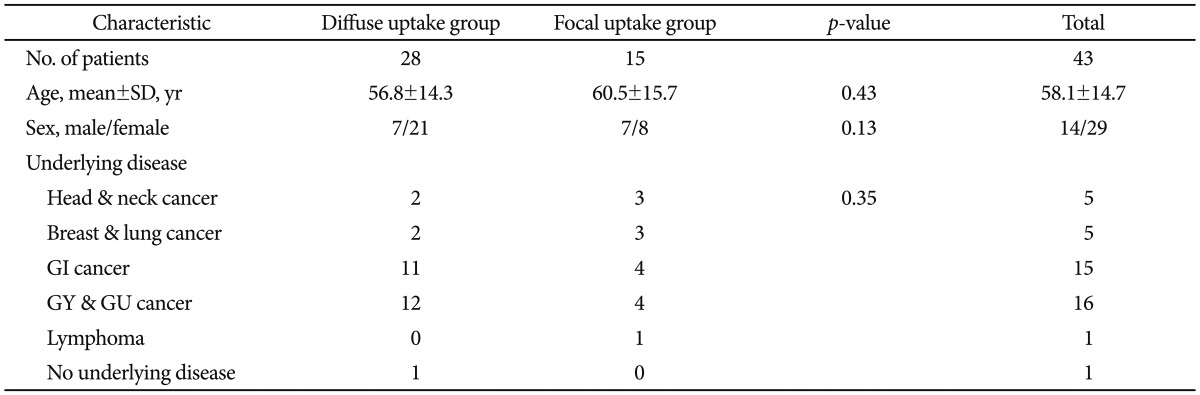
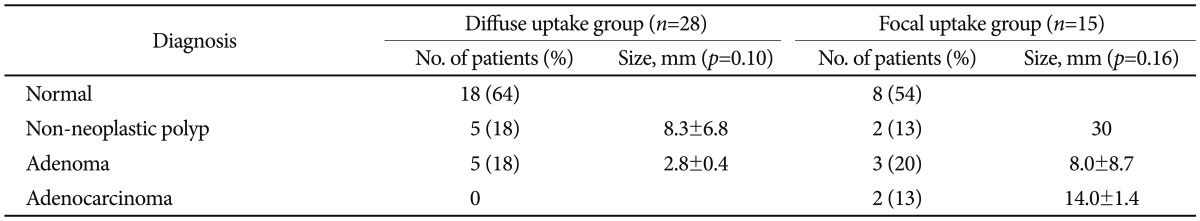
The mean age of 43 patients with benign colon FDG uptake were 58 years, 14 of them male and 29 female. Twenty-eight patients among them were diffuse group and 15 were focal group (Table 1). There wasn't a difference either in their mean age (57 years vs. 61 years, respectively; p=0.43) or in sex distribution (p=0.15). The underlying diseases in the diffuse group included squamous cell carcinoma in the oral cavity (n=1), thyroid cancer (n=1), breast cancer (n=2), pancreatic cancer (n=1), colorectal cancer (n=10), ovarian cancer (n=3), endometrial cancer (n=4), uterine cervical cancer (n=3), renal cell carcinoma (n=1), bladder cancer (n=1), and CA-125 increase without underlying disease (n=1). The underlying diseases in the focal group included nasopharyngeal cancer (n=1), thyroid cancer (n=2), lung cancer (n=3), colorectal cancer (n=4), ovarian cancer (n=3), prostate cancer (n=1), and lymphoma (n=1).
Among 28 patients in the diffuse group, lesions were detected in 10 patients by colonoscopy; 9 of them were being followed for malignancy and 1 was examined due to the increase in CA-125. According to the results of these 10 patients, 7 of them had concordance between the locations of FDG uptake and the colonoscopic lesions.
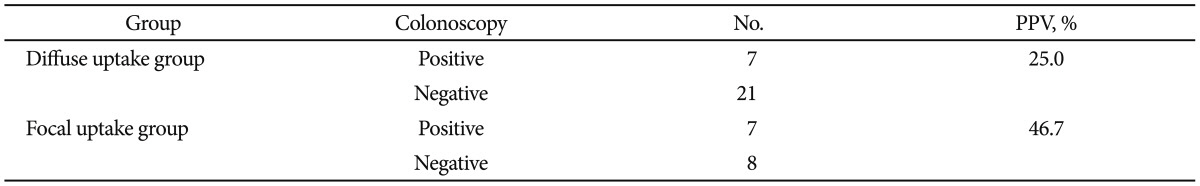
Among 15 patients in the focal group, lesions were detected in 7 patients by colonoscopy. Five patients (71.4%) had FDG uptake in the left side colon and 2 patients (28.6%) in the right side colon; all of them had concordance between the locations of FDG uptake and the colonoscopic lesions. Seven among 28 patients in the diffuse group and 7 among 15 patients in the focal group had colonoscopic lesions concordant with the FDG uptake, with positive predictive values of FDG-PET scan being 25% and 47%, respectively (Table 2).
FDG-PET uptake patterns were compared with the colonoscopic and pathologic findings (Table 3), and were classified as normal, non-neoplastic polyp, adenoma, or adenocarcinoma. In the diffuse group, 5 patients (18%) were diagnosed as non-neoplastic polyps and another 5 patients (18%) as adenomas, without size difference between the detected non-neoplastic polyps and adenoma lesions (p=0.10). In the focal group, 5 patients (33%) had neoplastic lesions and 2 of them (13%) were diagnosed as adenocarcinomas, without size difference between the diagnosed non-neoplastic polyps, adenomas and adenocarcinoma lesions (p=0.16).
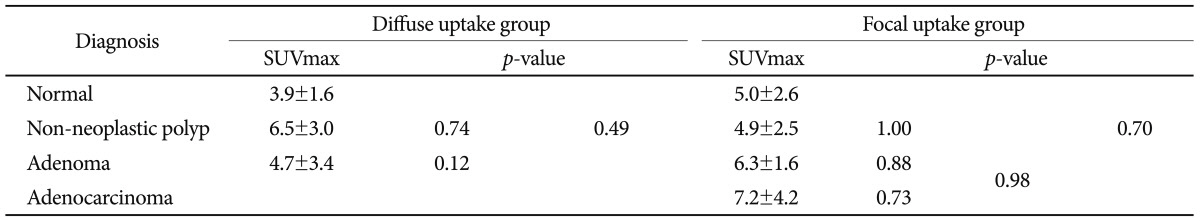
The maximum SUV values of 43 patients with benign FDG uptake ranged from 2 to 11, and the mean values of diffuse group and focal group were 4.5±2.3 and 5.5±2.5, respectively, without significant between-group difference (p=0.20). Also, there wasn't a significant difference in the maximum SUV value according to the diagnosed disease in both groups (diffuse group, p=0.14; focal group, p=0.70) (Table 4). When comparing histologic findings and maximal SUV values between 50 patients with malignant uptake in the colon and 10 patients with benign uptake as diagnosed neoplastic lesion, however, patients with neoplastic lesion had significantly increased maximal SUV value (p=0.009) (Fig. 2). High grade dysplasia had greater maximal SUV value among adenomas (p=0.02), while there was no statistically significant difference in the maximal SUV value according to differentiation of adenocarcinoma (p=0.20).
The first case was a 62-year-old male being followed for prostate cancer. He showed benign FDG uptake of 4.2 maximal SUV in the left lower abdomen on FDG-PET and 13-mm size of polyp in the descending colon on colonoscopy, with villotubular adenoma with focal adenocarcinoma involving mucosa (Fig. 3).
The second case was a 70-year-old male being followed for nasopharyngeal cancer. He showed benign FDG focal uptake of 10.1 maximal SUV in the left upper abdomen on FDG-PET and 15-mm size of focal well differentiated adenocarcinoma with coexisting villotubular adenoma in the distal transverse colon on colonoscopy (Fig. 4).
In this study comparing benign FDG uptake on FDG-PET with colonoscopic findings, most cases with diffuse uptakes were normal; few adenomas with small size were detected and malignant lesions were not detected. Among patients with focal uptake, colonoscopic lesions were detected in 45%; all of them were concordant with the locations of uptakes on FDG-PET with bigger size than those detected in the diffuse group (p=0.05). There was no difference in size between the diagnosed non-neoplastic polyps, adenomas and adenocarcinoma lesions (p=0.16). Some patients in the focal group were diagnosed as adenocarcinomas.
The FDG-PET is known to have 92.3% to 100%1,2,6,7 sensitivity and 40% to 60%5,8 specificity in diagnosing colorectal cancer. Benign uptake, including physiological uptake, of FDG is the reason of low specificity. Physiological uptake includes physiological accumulation of FDG inside the intestinal wall, FDG uptake by reactive lymphocyates in the terminal ileum and cecum, uptake by secretions in the intestine and enterobacteria. Adenoma and inflammatory bowel diseases, such as pseudomembranous colitis, Crohn's disease and ulcerative colitis, may also induce benign FDG uptake.3 The incident FDG uptake in colon has reported to 1.3% to 2.7% with increase of prevalence of various cancers and subsequently increased use of FDG-PET scan for diagnosis, staging and post-treatment follow-up of cancers.3,9,10 Diffuse FDG uptake is more frequently associated with physiological uptake,11-13 while focal uptake may be associated with malignant and pre-malignant lesion.13,14
Focal uptake in colon on FDG-PET scan is highly sensitivity to diagnosing pre-malignant lesion. Gutman et al.9 performed colonoscopy in patients with incident FDG focal uptake in colon on FDG PET/CT and found lesions in 66.7%; 81% of the detected lesions were advanced adenomas. Among 3,210 asymptomatic patients who received FDG-PET scan for screening, 20 patients showed FDG focal uptake in the colon and their colonoscopy revealed villous adenoma in 12 patients, tubular adenoma in 2 patients, and adenocarcinoma in 6 patients.15 In a study of 1,000 patients who had been diagnosed as malignancy and received FDG-PET,16 20 FDG focal uptakes were detected in 16 patients; 2 lesions were diagnosed as adenocarcinoma, 6 as villotubular adenoma and 1 as tubular adenoma, among 14 lesions of 10 patients who were available for pathological examinations by surgery or endoscopy. While these previous studies focused on incident benign and malignant focal FDG uptakes, this study aimed to determine clinical meanings of suspected benign focal uptake excluding definite malignant uptake based on FDG uptake pattern and appearance. When colonoscopy was performed in cases suspected of benign focal uptake on FDG-PET, lesions were detected in 46% of patients and neoplastic lesions such as adenoma and adenocarcinoma were diagnosed in 33% of patients. We confirmed concordance between the locations of focal uptakes and colonoscopic lesions, suggesting that even the cases suspected of benign focal FDG uptake may be diagnosed as pre-malignant lesion or early adenocarcinoma.
Focal FDG uptakes on FDG-PET scan is determined as suspected benign or malignant uptake based on its pattern, intensity or its relationship with adjacent structures. A lot of studies have been performed on deciding benignancy or malignancy of focal uptake or on criteria of additional tests for patients suspected of benign uptake, many of them using maximal SUV value. Strauss et al.17 found SUV values of 22 colorectal cancer lesions were significantly higher than 15 normal tissues (7.85±4.89 vs. 1.72±0.49, p=0.00), but the SUV values of colorectal cancer lesions varied widely from 1.76 to 19.45. In a comparison study of SUVs between recurrent lesions of rectal cancer and benign lesions by FDG-PET scan among patients followed for rectal cancer, the malignant lesions had significantly higher SUV values than benign lesions, which were all below 3.5.6 The malignancies had increased SUV values than adenoma (p=0.05) and normal tissues (p=0.03) and the difference was statistically significant.18 In a study of PET scan in 968 patients on follow-up for lung cancer, however, 8 patients were diagnosed as colorectal cancer without significant difference in their SUV values with benign lesions and normal tissues.19
When benign lesions and malignant lesions were compared, in this study, based on the histopathologic findings, maximal SUV values were raised in cases with malignant uptakes. Maximal value of up to 12 was measured in benign lesion, however, suggesting that maximal SUV value may not be available as an independent indicator for diagnosing benign and malignant lesions. But considering 90.7% of sensitivity and 68.4% of specificity of predicting neoplastic lesions, with a cut-off value of 4.95 in maximal SUV, higher values may be presumed as higher possibility of being a malignant lesion. When comparing adenoma, high grade dysplastic adenoma, well differentiated adenocarcinoma and poorly differentiated adenocarcinoma, maximal SUV value was the highest in high grade dysplastic adenoma (p=0.009), followed by well differentiated adenocarcinoma, poorly differentiated adenocarcinoma and low grade dysplastic adenoma in descending order. Although there are not many studies on difference of SUV values according to the degree of differentiation in colon, our results are in line with those of Gutman et al.9
In conclusion, by comparing patterns and intensities of benign colon uptake on FDG-PET with endoscopic and pathologic findings, we confirmed that patients showing benign FDG uptake in the colon should be further evaluated by colonoscopy, especially for patients with focal FDG uptake.
References
1. National Cancer Information Center. [Internet]. c2011. cited 2011 Dec 20. Goyang: National Cancer Information Center;Available from: http://www.cancer.go.kr/ncic/cics_f/02/022/index.html.
2. Kantorová I, Lipská L, Bêlohlávek O, Visokai V, Trubaĉ M, Schneiderová M. Routine (18)F-FDG PET preoperative staging of colorectal cancer: comparison with conventional staging and its impact on treatment decision making. J Nucl Med. 2003; 44:1784–1788. PMID: 14602860.
3. Israel O, Yefremov N, Bar-Shalom R, et al. PET/CT detection of unexpected gastrointestinal foci of 18F-FDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med. 2005; 46:758–762. PMID: 15872347.
4. Jadvar H, Schambye RB, Segall GM. Effect of atropine and sincalide on the intestinal uptake of F-18 fluorodeoxyglucose. Clin Nucl Med. 1999; 24:965–967. PMID: 10595478.

5. Abdel-Nabi H, Doerr RJ, Lamonica DM, et al. Staging of primary colorectal carcinomas with fluorine-18 fluorodeoxyglucose whole-body PET: correlation with histopathologic and CT findings. Radiology. 1998; 206:755–760. PMID: 9494497.

6. Keogan MT, Lowe VJ, Baker ME, McDermott VG, Lyerly HK, Coleman RE. Local recurrence of rectal cancer: evaluation with F-18 fluorodeoxyglucose PET imaging. Abdom Imaging. 1997; 22:332–337. PMID: 9107663.
7. Huebner RH, Park KC, Shepherd JE, et al. A meta-analysis of the literature for whole-body FDG PET detection of recurrent colorectal cancer. J Nucl Med. 2000; 41:1177–1189. PMID: 10914907.
8. Falk PM, Gupta NC, Thorson AG, et al. Positron emission tomography for preoperative staging of colorectal carcinoma. Dis Colon Rectum. 1994; 37:153–156. PMID: 8306836.

9. Gutman F, Alberini JL, Wartski M, et al. Incidental colonic focal lesions detected by FDG PET/CT. AJR Am J Roentgenol. 2005; 185:495–500. PMID: 16037527.

10. Kamel EM, Thumshirn M, Truninger K, et al. Significance of incidental 18F-FDG accumulations in the gastrointestinal tract in PET/CT: correlation with endoscopic and histopathologic results. J Nucl Med. 2004; 45:1804–1810. PMID: 15534047.
11. Prabhakar HB, Sahani DV, Fischman AJ, Mueller PR, Blake MA. Bowel hot spots at PET-CT. Radiographics. 2007; 27:145–159. PMID: 17235004.

12. Ahmad Sarji S. Physiological uptake in FDG PET simulating disease. Biomed Imaging Interv J. 2006; 2:e59. PMID: 21614339.

13. Tatlidil R, Jadvar H, Bading JR, Conti PS. Incidental colonic fluorodeoxyglucose uptake: correlation with colonoscopic and histopathologic findings. Radiology. 2002; 224:783–787. PMID: 12202714.

14. Kresnik E, Mikosch P, Gallowitsch HJ, Heinisch M, Lind P. F-18 fluorodeoxyglucose positron emission tomography in the diagnosis of inflammatory bowel disease. Clin Nucl Med. 2001; 26:867. PMID: 11564929.

15. Chen YK, Kao CH, Liao AC, Shen YY, Su CT. Colorectal cancer screening in asymptomatic adults: the role of FDG PET scan. Anticancer Res. 2003; 23:4357–4361. PMID: 14666651.
16. Pandit-Taskar N, Schöder H, Gonen M, Larson SM, Yeung HW. Clinical significance of unexplained abnormal focal FDG uptake in the abdomen during whole-body PET. AJR Am J Roentgenol. 2004; 183:1143–1147. PMID: 15385321.

17. Strauss LG, Klippel S, Pan L, Schönleben K, Haberkorn U, Dimitrakopoulou-Strauss A. Assessment of quantitative FDG PET data in primary colorectal tumours: which parameters are important with respect to tumour detection? Eur J Nucl Med Mol Imaging. 2007; 34:868–877. PMID: 17219134.

18. Weston BR, Iyer RB, Qiao W, Lee JH, Bresalier RS, Ross WA. Ability of integrated positron emission and computed tomography to detect significant colonic pathology: the experience of a tertiary cancer center. Cancer. 2010; 116:1454–1461. PMID: 20143447.
19. Isobe K, Hata Y, Sakaguchi S, et al. The role of positron emission tomography in the detection of incidental gastrointestinal tract lesions in patients examined for lung cancer. Nihon Kokyuki Gakkai Zasshi. 2010; 48:482–487. PMID: 20684209.
Fig. 1
Classification according to benign colon uptake pattern in fluorodeoxyglucose positron emission tomography. (A) Diffuse group. It showed diffuse colon uptake. (B) Focal group. It showed focal colon uptake.
Fig. 2
Per-lesion standardized uptake value intensity (maximum standardized uptake value [SUVmax]) mean and standard deviation for different colonoscopic findings. The neoplastic lesion had significantly increased maximal SUV value (p=0.009) and high grade dysplasia had greater maximal SUV value among adenomas (p=0.02). The SUVmax is 6.1±3.2 for low grade dysplasia adenoma (n=10), 12.9±4.2 for high grade dysplasia adenoma (n=2), 9.6±3.4 for well to moderately differentiated adenocarcinoma (n=44) and 6.6±2.0 for poorly differentiated adenocarcinoma (n=4).
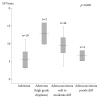
Fig. 3
A 62-year-old male with prostate cancer. (A) Intense focal standardized uptake (maximum standardized uptake value, 4.2) is located in descending colon. (B) A 13-mm polyp is found in colonoscopy. (C) The pathologic diagnosis is villotubular adenoma with focal adenocarcinoma involving mucosa (left, H&E stain, ×40; right, ×200).

Fig. 4
A 70-year-old male with nasopharyngeal cancer. (A) Intense focal standardized uptake (maximum standardized uptake value, 10.1) is located in transverse colon. (B) A 15-mm polyp is found in colonoscopy. (C) The pathologic diagnosis is focal well differentiated adenocarcinoma with coexisting villotubular adenoma (left, H&E stain, ×40; right, ×200).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download