Abstract
Biliary strictures can be caused by various diseases. Intrahepatic duct (IHD) strictures are usually related to IHD stones and cholangitis. However, focal IHD strictures without IHD stones often create diagnostic problems. Parasitic diseases such as clonorchiasis can be a rare cause of an IHD stricture. Human clonorchiasis (Clonorchis sinensis infection) is an endemic parasitic disease in Eastern Asia, including Korea, and patients acquire the infestation by eating raw fish. On radiological examinations, clonorchiasis shows typically diffuse, minimal, or mild dilatation of the small IHD, particularly in the periphery, without dilatation of the extrahepatic duct. However, diagnosis of clonorchiasis can sometimes be difficult when radiological changes are atypical. We report a case of focal left IHD dilatation caused by clonorchiasis that was confused with a malignancy.
Intrahepatic duct (IHD) strictures are usually caused by IHD stones or cholangitis.1,2 Focal IHD strictures unrelated to IHD stones often create diagnostic problems, though. Bile duct strictures are caused by various inflammatory diseases and benign or malignant bile duct tumors. Parasitic diseases could also rarely cause IHD strictures.1
Clonorchis sinensis is a trematode inhabiting chronically in the biliary tract. The incidence of clonorchiasis is decreasing in Korea, but there are still some endemic areas around the basins of the 5 largest rivers due to the habit of eating a raw freshwater fish.3-5 Clonorchiasis generally shows normal extrahepatic duct and diffuse dilatation of small IHD on radiologic test.6-9 But diagnosis of clonorchiasis can sometimes be difficult when those characteristic findings are not detected.
Now, we report a literature review and our experience of a 53-year-old female case who was first suspected of cholangiocarcinoma on radiologic examination of focal IHD dilatation but later was diagnosed as clonorchiasis and treated by percutaneous transhepatic cholangioscopy (PTCS).
A 53-year-old woman visited our hospital with upper abdominal pain started a week ago. The abdominal ultrasonography (US) and computed tomography (CT) performed at another hospital revealed focal dilatation of left IHD and multiple gallstones (Fig. 1). She did not have any history of alcohol drinking or smoking and any abnormality in the past medical and family histories. She was alert without fever or acute illness at admission. Conjunctivae and sclerae were normal at physical examinations. There was slight tenderness on the right upper quadrant without rebound tenderness, and the liver, spleen, or mass was not palpable at physical examinations. Vital signs at admission were measured as blood pressure 120/80 mm Hg, pulse rate 88/min, respiration rate 20/min, and body temperature 36.6℃ . Laboratory tests showed white blood cell count 7,870/mm3 (6% eosinophils), AST 25 IU/L, ALT 12 IU/L, alkaline phosphatase 202 IU/L, total bilirubin 0.6 mg/dL, direct bilirubin 0.14 mg/dL, serum amylase 53 IU/L, total protein 7.6 g/dL, and albumin 4.5 g/dL. The viral markers for hepatitis were all negative and the levels of tumor markers (α-FP, CA19-9, CEA) were normal. Magnetic resonance cholangiopancreatography (MRCP) was performed after hospitalization for exclusion of stricture by malignancy. Marked dilatation and stricture of the left IHD and multiple gallstones were found on MRCP without any evidence of apparent mass (Fig. 2). PTCS was performed for differential diagnosis and targeted biopsy, since it was decided that endoscopic retrograde cholangiopancreatography (ERCP) was not suitable for easy accessibility to proximal of left IHD and accurate biopsy (Fig. 3A). A 8.5 Fr catheter (Wilson-Cook Co., Winston-Salem, NC, USA) was first inserted in the right bile duct through the percutaneous transhepatic route guided by a sonographic probe, and the sinus tract was dilated using a 18 Fr catheter twice in 2-3 days interval. PTCS was performed 2 weeks later and found a dark brown, soft mass obstructing the lumen of bile duct at the stricture site on radiologic examinations (Fig. 4A). After removal of sludge-like materials by basket, flat leaf-shaped, brownish worm was observed. It was identified as Clonorchis sinensis (Fig. 4B). It was found that the IHD was obstructed by Clonorchis worms, which were removed by endoscopic forcep. After removal of adult worms, there was not the stricture segment of IHD and no abnormalities of proximal to stricture site or adjacent bile duct (Fig. 4C). Cholangioscopy of the stricture segment did not find any abnormal tumor vessels, surface irregularities, or tumor invasion of bile duct wall suggesting malignancy, and the histopathological examination also revealed no abnormality except for the inflammatory cells. It was concluded that the focal IHD stricture and dilatation on radiologic examinations were actually bile duct obstruction by Clonorchis worms and bile sludge (Fig. 3B). Stool examination was negative and serologic test (enzyme-linked immunosorbent assay, ELISA) for Clonorchis sinensis was positive. Praziquantel (25 mg/kg, three times a day) was administered and the patient was discharged without any problem.
Inflammatory diseases and benign or malignant bile duct tumors may cause focal strictures of IHD. Focal IHD strictures in Asians are usually caused by intrahepatic stones and cholangitis.1,2 The diagnosis may become more difficult when IHD stricture does not accompany IHD stones or mass. Seo et al.1 noted that 70% of the focal IHD strictures without stone are associated with malignancy, emphasizing the importance of differential diagnosis of malignant tumor. Among various radiologic examinations for IHD stricture evaluation, abdominal US and CT are most useful for early diagnosis of ductal stricture. Non-invasive radiologic examinations such as MRCP and endoscopic ultrasonography are recently developed for diagnosis. However, the diagnosis of IHD stricture usually requires tissue biopsy through invasive examinations such as ERCP or cholangioscopy for accurate diagnosis, because such strictures are sometimes difficult to differentiate malignancy only from radiologic findings.
Some patients with focal strictures of IHD are usually asymptomatic or without jaundice, complicating the detection of lesion and its cause.1 Focal strictures of IHD are often detected incidentally in asymptomatic patients on abdominal US or CT for routine medical check-up. South Korea is an endemic area of clonorchiasis, and the possibility of parasitic causes such as clonorchiasis should be considered for cause of IHD strictures.3-5 Clonorchiasis is a parasitic disease caused by chronic infestation of Clonorchis sinensis, mostly when eating an infected freshwater fish without cooking. The ingested egg of Clonorchis sinensis is excysted in duodenum and migrates through common bile duct to the intrahepatic bile duct, where they are matured adult worms.10,11 Clonorchiasis may cause irregular dilatation of bile duct, mucous gland hyperplasia, metaplasia of mucin-producing cell, and periductal fibrosis, and even cholangiocarcinoma in chronic cases.10 Stricture by clonorchiasis is characterized by repeated stricture and dilatation in multiple branches of distal IHD, unlike the focal stricture of bile duct.6-9
Clonorchis worms inside the bile duct are difficult to detect by US or CT, which shows normal extrahepatic duct and diffuse, uniform dilatation of IHD, particularly of peripheral intrahepatic bile duct.9 Pathognomonic finding of ERCP includes round, elliptical, filamentous shaped filling defects by worms in midium- or small-sized IHD, particularly in the periphery.6,7,12 Diffuse, uniform dilatation of IHD and hazy appearance of bile duct wall due to the hyperplasia of bile duct epithelium are also observed.7,13 Extrahepatic bile duct, on the other hand, does not show any abnormality except for minimal or no dilatation and ductal wall irregularity.7
This case showed focal dilatation of left IHD caused by the ductal obstruction of the Clonorchis worms without the peripheral IHD dilatation and stricture normally seen in Clonorchiasis patients, complicating differential diagnosis with strictures by malignancy. Such focal obstructive lesions caused by clonorchiasis in larger bile ducts such as common bile duct or hepatic duct bifurcation, mimics strictures by cholangiocarcinoma, further complicating the diagnosis.14-17 Cholangitis by stones or strictures often requires surgical treatment, while clonorchiasis may be resolved by medical treatment, which is why the differential diagnosis is essential. Tissue diagnosis by invasive examination might be required in the end for differential diagnosis of strictures without definite reason. Cases with ductal stricture without the evidence of mass, as in our patient, are difficult to obtain adequate biopsy specimen.
Percutaneous transhepatic biopsy under the sonographic guidance may not easy to collect accurate specimens in cases without distinct evidence of tumor. ERCP enables the terminal branch view and biopsy or therapeutic intervention could be performed at the same time.7 But, a 'missing duct' finding appears proximal to the stricture site, making the differential diagnosis more difficult. And lesions at proximal portions of right or left main bile duct are difficult to access and collect adequate biopsy specimen.1 PTCS, on the other hand, is suitable for direct visualization of mucosal appearance and accurately targeted biopsy of stricture sites, which are very useful features for diagnosis of focal IHD strictures, although it takes some time to make a percutaneous transhepatic tract.1 In addition, by balloon dilatation the access is also possible at the stricture site and the proximal lesion of stricture, when the stricture is severe. The patient in this study was also deemed difficult to access and perform adequate biopsy by ERCP with the stricture locating at the proximal of left main bile duct. PTCS was performed for differential diagnosis of intrahepatic cholangiocarcinoma. Through the right IHD (opposite side), the stricture lesion and the adjacent bile duct was easily accessible. The approaching strategy through the opposite side is favorable because access could be difficult to the stricture of bile duct when bile duct and endoscope make the acute angulation. Cholangioscopy in this case was very useful for differential diagnosis of causes of the stricture, because it was capable of performing the visualization of the IHD lesion, the targeted biopsy, and the selective cholangiography simultaneously.
We reported here a case of left focal IHD dilatation caused by clonorchiasis mimicking a stricture by malignancy, diagnosed by PTCS and removed by endoscopic procedure followed by medical therapy. Being an endemic area of clonorchiasis, the possibility of stricture by clonorchiasis should be considered when a Korean patient, particularly a patient residing in the vicinity of a river, shows a focal IHD stricture and dilatation.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (20100005190).
References
1. Seo DW, Kim MH, Lee SK, et al. Usefulness of cholangioscopy in patients with focal stricture of the intrahepatic duct unrelated to intrahepatic stones. Gastrointest Endosc. 1999; 49:204–209. PMID: 9925699.

2. Yeh YH, Huang MH, Yang JC, Mo LR, Lin J, Yueh SK. Percutaneous transhepatic cholangioscopy and lithotripsy in the treatment of intrahepatic stones: a study with 5 year follow-up. Gastrointest Endosc. 1995; 42:13–18. PMID: 7557170.

3. Kim TS, Cho SH, Huh S, et al. A nationwide survey on the prevalence of intestinal parasitic infections in the Republic of Korea, 2004. Korean J Parasitol. 2009; 47:37–47. PMID: 19290090.

4. Cho SH, Lee KY, Lee BC, et al. Prevalence of clonorchiasis in southern endemic areas of Korea in 2006. Korean J Parasitol. 2008; 46:133–137. PMID: 18830051.

5. Joo CY, Chung MS, Kim SJ, Kang CM. Changing patterns of Clonorchis sinensis infections in Kyongbuk, Korea. Korean J Parasitol. 1997; 35:155–164. PMID: 9335180.

6. Lee JI, Yoo JH, Lim GS, Lee CH, Min YI, Lim JH. ERCP findings in clonorchiasis. Korean J Gastrointest Endosc. 1981; 1:29–32.
7. Kang DH, Choi SH, Chun KJ, et al. ERCP findings in hepatic clonorchiasis. Korean J Gastrointest Endosc. 1993; 13:121–125.
8. Lim JH. Radiologic findings of clonorchiasis. AJR Am J Roentgenol. 1990; 155:1001–1008. PMID: 2120925.

9. Choi D, Hong ST. Imaging diagnosis of clonorchiasis. Korean J Parasitol. 2007; 45:77–85. PMID: 17570969.

10. Choi BI, Han JK, Hong ST, Lee KH. Clonorchiasis and cholangiocarcinoma: etiologic relationship and imaging diagnosis. Clin Microbiol Rev. 2004; 17:540–552. PMID: 15258092.

11. Song HY, Rhee KS, Lee ST, Kim DK, Ahn DS. Clinical features in clonorchiasis. Korean J Gastroenterol. 1995; 27:64–71.
12. Chan HH, Lai KH, Lo GH, et al. The clinical and cholangiographic picture of hepatic clonorchiasis. J Clin Gastroenterol. 2002; 34:183–186. PMID: 11782616.

13. Jeen YM, Jin SY. Intrahepatic cholangiocarcinoma associated with Clonorchis sinensis infection. Korean J Hepatol. 2009; 15:524–527. PMID: 20037272.

14. Hwang CW, Lim BW, Ryu U, et al. A case of clonorchiasis presenting as common hepatic duct mass. Korean J Gastrointest Endosc. 2005; 31:268–272.
15. Chu DW, Li JC, Lee DW, Rong ZX, Chen XW, Chan AC. Unusual presentations of hepatic clonorchiasis. Gastrointest Endosc. 2003; 58:637–639. PMID: 14520309.

16. Oh JH, Kim HG. A case of clonorchiasis presenting as common bile duct mass. Korean J Gastroenterol. 2010; 56:211–213. PMID: 20962555.

17. Yoon KW, Park CH, Cho S, et al. A case of hemobilia caused by clonorchiasis. Korean J Gastrointest Endosc. 2008; 36:313–317.
Fig. 1
Contrast-enhanced computed tomography scan finding. It shows the dilatation of left intrahepatic bile duct without mass or intrahepatic stone.
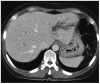
Fig. 2
Magnetic resonance cholangiopancreatography findings. (A) Axial T2 weighted image shows the marked dilatation and stricture (arrow) of left intrahepatic bile duct. (B) Coronal T2 weighted image shows the marked dilatation and stricture (arrow) of left intrahepatic bile duct. There is no evidence of stone and thickeness of duct wall at stricture segment.

Fig. 3
Cholangiographic findings. (A) Cholangioscope is inserted via a percutaneous transhepatic route. Radiograph shows the focal stricture (arrow) and dilatation of left intrahepatic duct (IHD) without abnormality of extrahepatic and right IHD. (B) After removal of the fluke, there is no evidence of filling defect at the left IHD.

Fig. 4
Percutaneous transhepatic cholangioscopy findings. (A) Dark brown, soft obstructive mass is found at stricture site of left intrahepatic duct. (B) Flat, leaf-shaped worm indentified as Clonorchis sinensis is observed after extraction of bile sludge. (C) The fluke is extracted with an endocopic forcep. After removal, there is no obvious stricture and surface irregularity or abnormal tumor vessel is not seen.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download