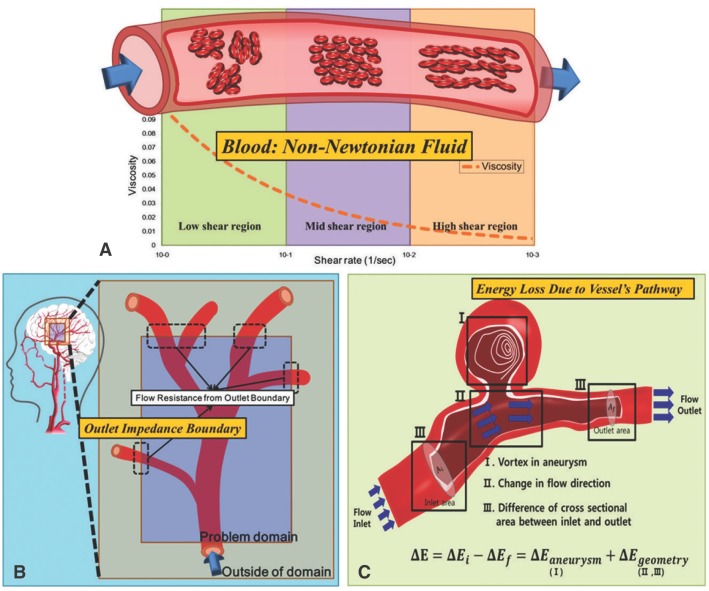
Non-Newtonian Properties
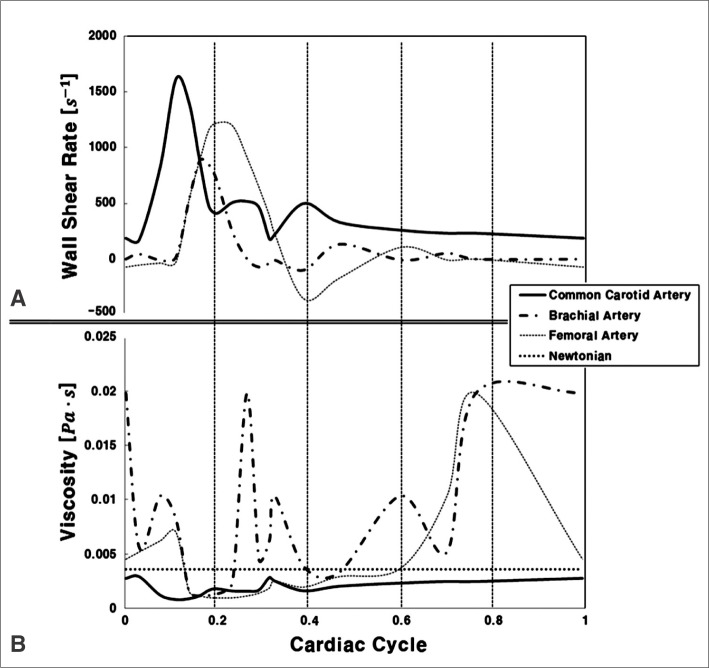 | Fig. 2
A. Wall shear rate predicted using the flow rate and radii common carotid, brachial, and femoral arteries reported by Stroev et al.[30] (Reprinted with permission) B. Viscosity calculated using shear rate from Carreau-Yasuda model (  = (1+(λη)a)(n-1)/a, µ0=0.0022 Paty c a=0.644, n=0.392, λ=0.110s) in common carotid, brachial, and femoral arteries compared to Newtonian viscosity[31]. = (1+(λη)a)(n-1)/a, µ0=0.0022 Paty c a=0.644, n=0.392, λ=0.110s) in common carotid, brachial, and femoral arteries compared to Newtonian viscosity[31]. |
Outlet Boundary Condition
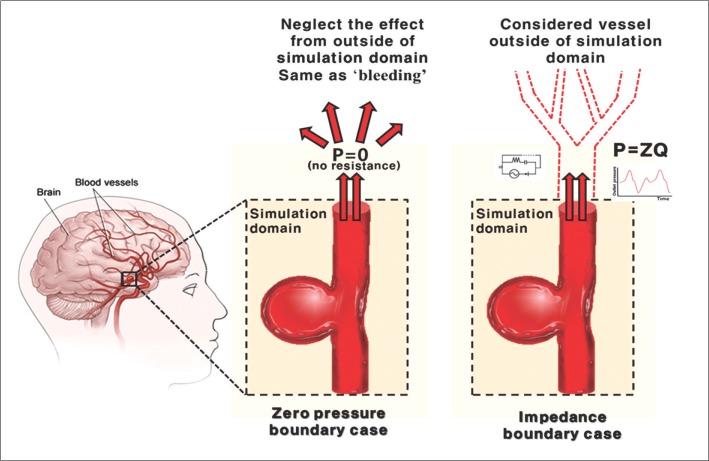 | Fig. 3Comparison between the zero pressure boundary condition and the impedance boundary condition. Zero pressure boundary condition assumes that pressure at the outlet boundary is zero, as if bleeding were occurring, without considering any influences from the vessels outside of the simulation domain. However, in impedance boundary case, as shown at right, the term Z is adopted to demonstrate the wave reflection caused by the outer domain. By regarding the blood flow of the whole vascular system as if it were electrical current running through a circuit, and so adopting the impedance term to express resistance of vessel to blood flow, the wave reflection is successfully accounted for at the outlet of the simulation domain. |
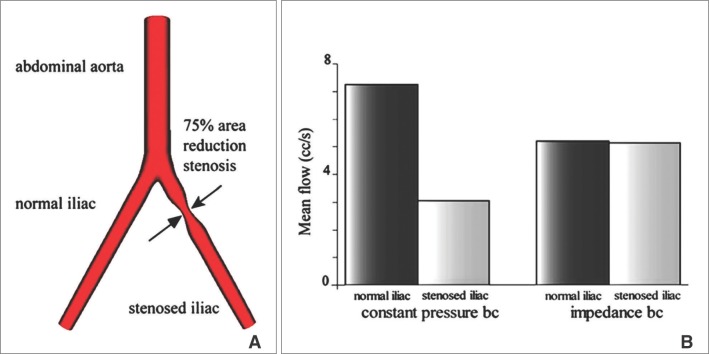 | Fig. 4The simulation of mean flow rate at the stenotic blood vessel with two different boundary conditions: the constant pressure and the impedance boundary condition [18]. (Reprinted with permission) A. Geometry of a bifurcated blood vessel with stenosis that reduces the cross sectional area by 75%. B. Flow distribution between normal and stenotic iliac vessels. Flow rate is calculated at the bottom end of each bifurcation. For the case of constant pressure boundary, the left branch of bifurcation with stenosis has a drastically different flow rate compared to the right branch, which is completely unrealistic. In the case of impedance boundary, however, the difference between the two branches is much smaller as the pressure from the outer domain has been applied properly. |
Energy Loss Due to the Vessel's Pathway
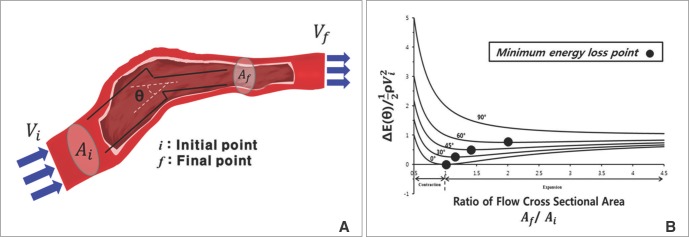 | Fig. 5
A. Schematic representation of a stream of fluid traversing a vessel from an initial position i to a final position f. Uniform flow experiences a sudden change in its cross-sectional area A and direction θ. The symbols Ai and Af each represent the cross-sectional area, and Vi and Vf represent the corresponding average velocities of flow. B. The relationship between geometrical energy loss and cross-sectional area ratio. Each line represents the degree of change in flow angle. Each dot represents the point where the loss becomes minimum at the listed angles (0°, 30°, 45°, 60°, 90°).[26, 28] (Reprinted with permission) |
 the cross-sectional area change is larger at each change of angle. In the case of a change in 90°, energy loss decreases to
the cross-sectional area change is larger at each change of angle. In the case of a change in 90°, energy loss decreases to  without a minimum value.
without a minimum value.A. Change in cross-sectional area but no alteration in direction of flow
 , which is term of Bernoulli's equation.
, which is term of Bernoulli's equation. =
=  ' which represent cross-sectional area ratio.
' which represent cross-sectional area ratio.  is from the Bernoulli's equation and
is from the Bernoulli's equation and  is the loss factor based on ratio of change in cross sectional area. As observed in Fig. 6A,
is the loss factor based on ratio of change in cross sectional area. As observed in Fig. 6A,  gets smaller with increasing N, meaning that the greater the cross-sectional area changes, the less the energy loss is.
gets smaller with increasing N, meaning that the greater the cross-sectional area changes, the less the energy loss is.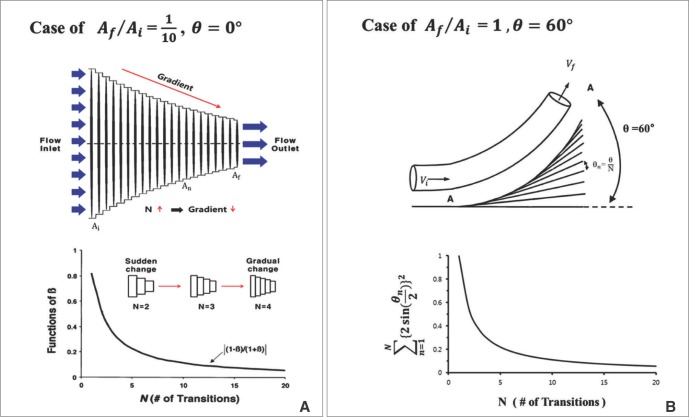 | Fig. 6
A. Gradual change of cross-sectional area and magnitude the function of β for increasing values of N (# of changes) at  = 1/10. B. Change in angle where there is no change in cross-sectional area. The graph at the bottom shows that a larger number of transitions causes the angle change to become more gradual resulting in lower 'loss factor'. Both cases have directional change of 60°[26]. (Reprinted with permission) = 1/10. B. Change in angle where there is no change in cross-sectional area. The graph at the bottom shows that a larger number of transitions causes the angle change to become more gradual resulting in lower 'loss factor'. Both cases have directional change of 60°[26]. (Reprinted with permission) |
B. No change in cross-sectional area but an alteration in direction of flow
 multiplied by 'energy loss factor'. This factor decreases as N increases (Fig. 6B). To sum up, the energy loss decreases as the angle change becomes more gradual
multiplied by 'energy loss factor'. This factor decreases as N increases (Fig. 6B). To sum up, the energy loss decreases as the angle change becomes more gradual



 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download