INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common entrapment disorder, characterized by combinations of specific clinical presentations [
1]. Currently, diagnosis is made based on characteristics symptoms and confirmed by nerve conduction studies and electromyography. In clinical practice, the electro-diagnostic (EDX) test is the most common and reliable evaluation method though it is uncomfortable and does not provide anatomic information about the median nerve and surrounding tissues. More recently, ultrasonography has been used to diagnose CTS because it is non-invasive, easily accessible, and provides spatial information [
23].
Diabetes mellitus (DM) is reported as a significant independent risk factor for CTS [
4]. Some studies reported peripheral nerve changes in DM patients and described enlarged median nerve cross-sectional area (CSA) regardless of the presence of peripheral polyneuropathy [
5]. However, other reports showed no significant difference in CSA in the wrist in DM patients with axonal (including diabetic) polyneuropathy compared to that of healthy volunteers [
67]. At this point, whether the median nerve is altered in patients with DM remains unclear. In addition, the specific criteria for the application of ultrasonography in DM patients have not been well established.
In this study, we aimed to assess the ultrasonographic changes in the median nerve between non-DM and DM patients with CTS. The diagnostic value of the ultrasonographic parameters in the discrimination between non-DM and DM cases was also investigated.
MATERIALS AND METHODS
Subjects
This study was a retrospective observational study of patients who underwent electrodiagnostic and ultrasonographic tests for the diagnosis of CTS. We carried out a retrospective analysis of 256 wrists with EDX evidence of CTS and 97 wrists without CTS in a single center between January 1, 2008 and January 1, 2013. DM was diagnosed according to the World Health Organization criteria [
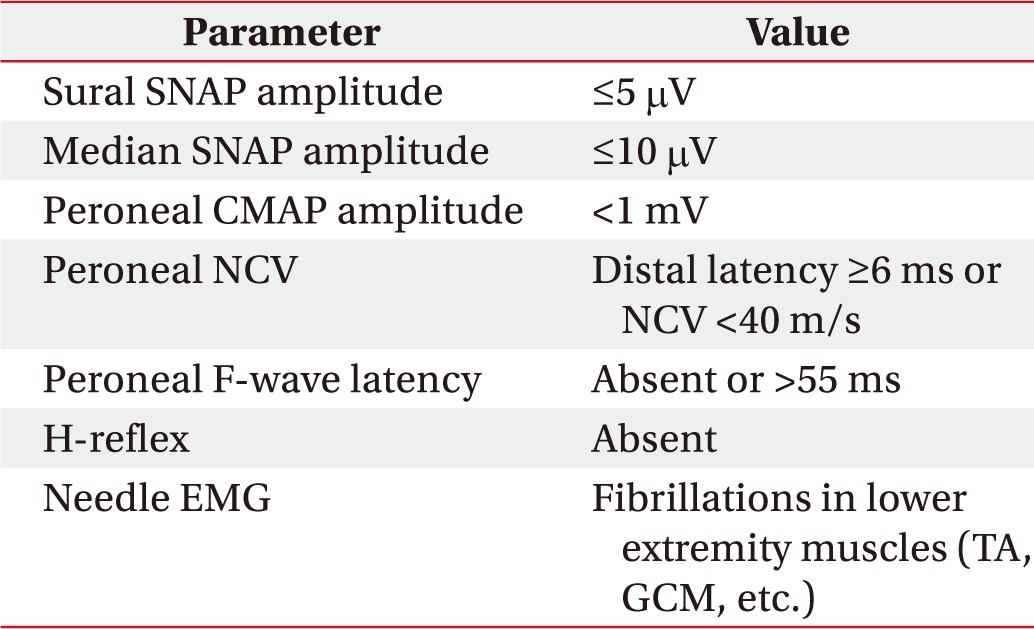
8]. Exclusion criteria for the study were as follows. (1) Patients with a clinical and electrophysiologic diagnosis of diabetic polyneuropathy. Clinical diagnosis was diagnosed based on the presence of one symptom (e.g., numbness, tingling, weakness, foot pain, or ataxia) or one sign (e.g., abnormal knee or ankle reflex). Diabetic polyneuropathy was electrophysiologically diagnosed by modified versions of the criteria suggested in the Diabetes Control and Complication Trial (
Table 1). And (2) Patients who underwent prior surgery for CTS, patients with cervical radiculopathy, and patients with any underlying metabolic disorders such as alcoholism, genetic disorders, gout, rheumatic arthritis or abnormal thyroid function related to peripheral neuropathy.
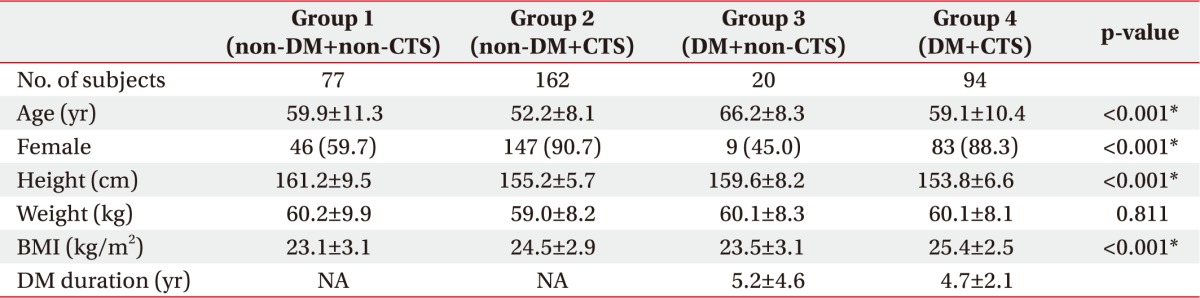
Patients were classified into four groups according to the presence of DM and CTS: group 1, non-DM and non-CTS patients; group 2, non-DM and CTS diagnosed patients; group 3, DM and non-CTS patients; and group 4, DM and CTS diagnosed patients.
Electro-diagnostic testing
The nerve conduction study was conducted using Nicolet Viking IV (Nicolet Biomedical, Madison, WI, USA). Skin temperature was maintained above 32℃. Standard tests included median sensory nerve conduction velocity within the 3rd digit/wrist segments and median distal motor latency from the wrist to the thenar eminence. When the standard tests were normal, further segmental tests were performed over a short distance of 7 cm or comparative median/ulnar studies. A median sensory nerve action potential was employed to record the initial latency and baseline to peak amplitude from the 3rd finger (active site), with retrograde stimulation being conducted at 14 cm proximal area from the recording site (wrist) and at 7 cm proximal area from the recording site (palm). The EDX criteria of CTS were determined as (1) median nerve distal sensory latency, upper limit of normal 3.7 ms; (2) difference between the median and ulnar nerve distal sensory latencies, upper limit of normal 0.4 ms; (3) distal motor latency over the thenar eminence, upper limit of normal 4.2 ms; (4) median motor nerve conduction velocity, lower limit of normal 49 m/s; (5) median sensory nerve conduction velocity, lower limit of normal 49 m/s; and (6) a ratio of proximal and distal onset latency >2.0.
Ultrasonography assessment
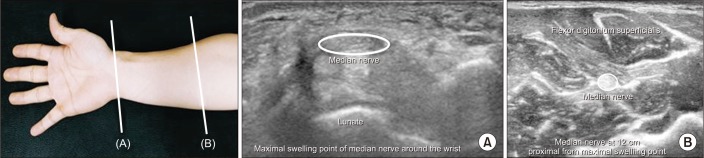
After the EDX, the median nerve on the wrist was examined with ultrasound performed by a skilled physiatrist with neuromuscular ultrasound experience. A physician, blinded to the EDX findings and clinical parameters, evaluated the ultrasonographic results. Imaging was performed using the HD15 ultrasonography system (Philips, Bothell, WA, USA) and a 7–12 MHz linear array transducer. The ultrasonography settings were optimized for nerve imaging, such as frequency, depth, and focal zone. The probe was maintained at a perpendicular angle during analysis to prevent anisotropy and median nerve deformation, and additional weight was not permitted when the pressure was applied to the skin surface with the probe. The CSA of the median nerve was measured by direct tracing with electronic calipers around the nerve circumference, excluding the hyperechoic epineuria rim. CSA was measured at two locations. The two locations of the median nerve ultrasonographic parameters included the maximal swelling point of the median nerve around the wrist and 12 cm proximal to the maximal swelling point (
Fig. 1). Following measurement, the CSA and the wrist to forearm ratio (WFR, defined as the ratio of the median nerve CSA at the maximal swelling site to its CSA at the 12 cm proximal site) were calculated.
Statistical analysis
Statistical analysis was performed using the SPSS statistical software version 22 for Windows (IBM, Armonk, NY, USA). All parameters were presented as the mean±standard deviation and compared among the groups. One-way ANOVA analysis was used to evaluate the differences in baseline characteristics among the groups. We used the analysis of covariance (ANCOVA) adjusting for baseline outcome values, for the comparison of the CSA and WFR. For post hoc testing, we used the Bonferroni correction. Receiver operating characteristics (ROC) curve analysis was used to determine the predictive CSA value for CTS. A p-value less than 0.05 was considered statistically significant.
DISCUSSION
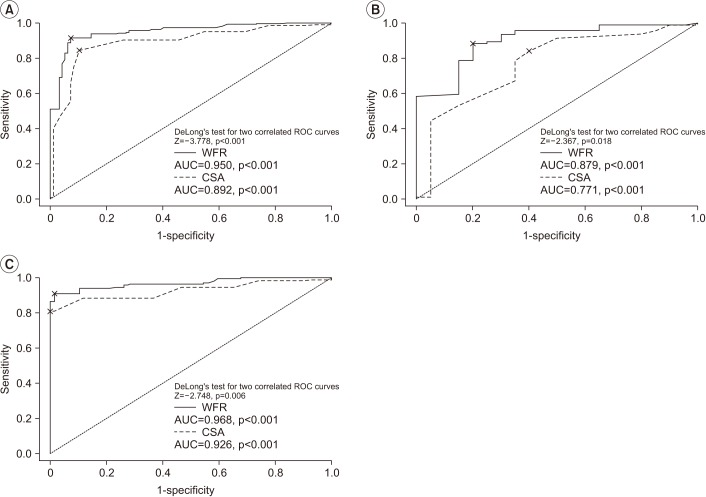
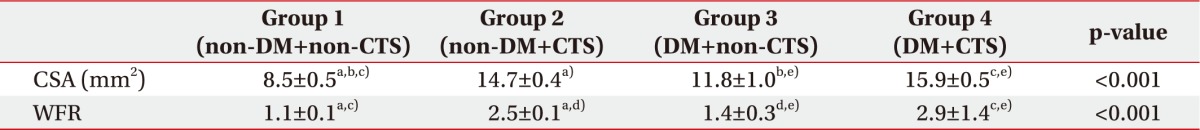
This study has several major findings. First, the CSA and WFR were larger in DM patients (excluding polyneuropathy) compared to non-DM patients in both non-CTS and CTS hands. Second, the diagnostic cut-off values of the CSA and WFR differed according to the presence or absence of DM. Lastly, based on the ROC analysis, WFR was observed to have a greater diagnostic value than the CSA of the median nerve at the maximal swelling site alone, irrespective of the DM status.
Numerous studies have shown the utility of ultrasound in the diagnosis of CTS [
910]. However, only a few studies have reported the importance of ultrasonographic measurements in discrimination between non-DM and DM patients with CTS, further confirmed by electrodiagnosis (excluding polyneuropathy).
Many studies have explained the enlargement of the median nerve in CTS employing a histopathological approach. In terms of the biologic response to compression of the peripheral nerve, it has been reported that the destruction of the blood-nerve barrier ischemia induces a cascade comprising of endoneurial edema, demyelination, perineural inflammation, axonal degeneration, generation of new axons, re-myelination, fibrosis, and thickening of the perineurium and endothelium [
1112]. Moreover, diabetes mellitus influences the susceptibility of the median nerve via the oxidative stress, (which initiates and amplifies neuro-inflammation) and/or the polyol pathway, (which includes glycation and proinflammatory reactions) [
1314]. Previous reports showed no significant difference in the wrist CSA of DM patients with axonal (including diabetic) polyneuropathy compared to that of the healthy volunteers [
67]. However, Pitarokoili et al. [
15] described the ultrasonographic changes in the peripheral nerves in diabetes and reported enlarged median nerve CSA at compression sites irrespective of the presence of peripheral polyneuropathy. Our results revealed larger CSA and WFR values in patients with DM than in non-DM patients. The differences in CSA and WFR between the two groups might be attributed to the increased vulnerability of the nerves of DM patients to external compression. The observed differences in the EDX parameters of CTS patients according to DM status corroborate that association.
Many reports have proposed a range of cut-off values for the CSA of the median nerve, and the thresholds reported for the diagnosis of CTS vary from 9 to 15 mm
2 [
16]. However, the currently established diagnostic cut-off values using ultrasonography were not tailored for patients with DM, which is considered an independent risk factor for CTS. We suggest the application of different cut-off values for patients with and without DM. Furthermore, the present study excluded DM patients with polyneuropathy, which was confirmed based on nerve conduction studies and medical record reviews in order to focus on the impact of DM alone. We determined the median nerve CSA cut-off value to be more than 10 mm
2 (sensitivity=88.3%, specificity=88.3%) for non-DM patients and 12.5 mm
2 (sensitivity=80.9%, specificity=80.0%) for DM patients.
The measurement of median CSA is accepted as the reliable diagnostic method but the CSA alone measurement may vary depending on the researchers and correlates with other patient's characteristics factors. Therefore, WFR has been suggested as a more accurate diagnostic index for CTS [
9]. In this study, CSA values were found to be higher in diagnosis either CTS or DM, though the diagnostic value of the CSA was not significantly different between groups 2 and 3. However, significant differences were observed in the diagnostic value of the WFR between groups 2 and 3. Consequently, the WFR was more highly associated with the diagnosis of CTS than the CSA. Moreover, the AUC value of the WFR obtained by ROC analysis was higher, especially in DM patients.
This study has some limitations. First, it was a relatively small-scale and single center-based study and the number of patients in group 3 was particularly small since the majority of DM patients visiting the outpatient clinic have clinical symptoms relevant to diabetic polyneuropathy and comes for confirmation of polyneuropathy. Second, ultrasonography is an operator-dependent test. The use of a single operator and the absence of repeated measurements are the weaknesses of this study. Third, it was not possible to exclude the association with factors related to symptoms, (e.g., the duration or, severity) of the DM or CTS. Therefore, future large-scale prospective studies are needed to confirm the role of DM in CTS pathophysiology.
In conclusion, DM patients showed increased CSA and WFR values compared to patients without DM. In the use of ultrasonographic assessment for the diagnosis of CTS, distinct cut-off values for patients with DM are necessary. Lastly, the ROC analysis revealed that a more precise diagnosis of CTS could be possible if WFR can be applied in place of CSA.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download